Stress creates immediate and long-lasting changes in your gut, affecting digestion, microbiome balance, inflammation, and the gut–brain axis. Understanding how stress influences your gut helps you recognize why emotional stress often leads to digestive problems, microbiome disruption, and chronic gut symptoms. This guide explains exactly how stress impacts your gut health, digestion, and microbial balance, and how to protect your digestive system during stressful periods.
Key Takeaways
- Stress disrupts gut function because the gut–brain axis instantly responds to emotional and physical stress signals.
- Cortisol alters digestion by slowing stomach emptying, reducing enzymes, and increasing intestinal inflammation.
- Stress creates microbiome imbalance by reducing beneficial bacteria and allowing harmful microbes to thrive.
- Emotional stress often triggers digestive issues such as bloating, cramps, nausea, and irregular bowel movements.
- Chronic stress weakens the gut barrier, increasing sensitivity, inflammation, and digestive discomfort.
- Managing stress supports long-term gut health by protecting microbiome diversity and improving digestive efficiency.
How Stress Influences Your Gut: Why the Gut Reacts Immediately
The gut responds instantly to stress because it is connected directly to the brain through the gut–brain axis, a communication system involving hormones, nerves, and neurotransmitters. This means emotional stress, mental pressure, or fear can produce physical digestive symptoms within seconds.Stress signals activate your nervous system and hormones, which immediately alter digestion.
- Stress triggers the fight-or-flight response, and this shifts blood flow away from digestion to prioritize survival functions.
- The brain sends emergency signals through the vagus nerve, and these signals slow digestion and trigger abdominal tension.
- Stress hormones such as cortisol disrupt gut movement, causing either slowed motility or rapid motility depending on the individual.
- Stress reduces the activity of digestive enzymes, which makes it harder to break down food efficiently.
- Emotional stress increases intestinal sensitivity, making normal sensations feel painful or uncomfortable.
How Stress Impacts Your Gut Health

Stress influences nearly every part of the digestive system. Short-term stress causes rapid digestive changes, while long-term stress contributes to inflammatory gut conditions, reduced microbial diversity, and chronic digestive symptoms.
Short-Term Effects of Stress on Gut Health
These immediate effects are common during stressful days or sudden emotional triggers.
- Stress can cause bloating and gas because the gut becomes more reactive and digestion slows.
- Stomach discomfort increases because stress elevates acid fluctuations and muscle tension.
- Quick shifts from diarrhea to constipation may occur due to inconsistent colon motility.
- Appetite may decrease or increase because stress alters hunger hormones.
- People may experience nausea because stress tightens the stomach muscles and reduces blood flow to the gut.
Long-Term Effects of Stress on Gut Health
Chronic stress creates deeper gut disruptions that accumulate over time.
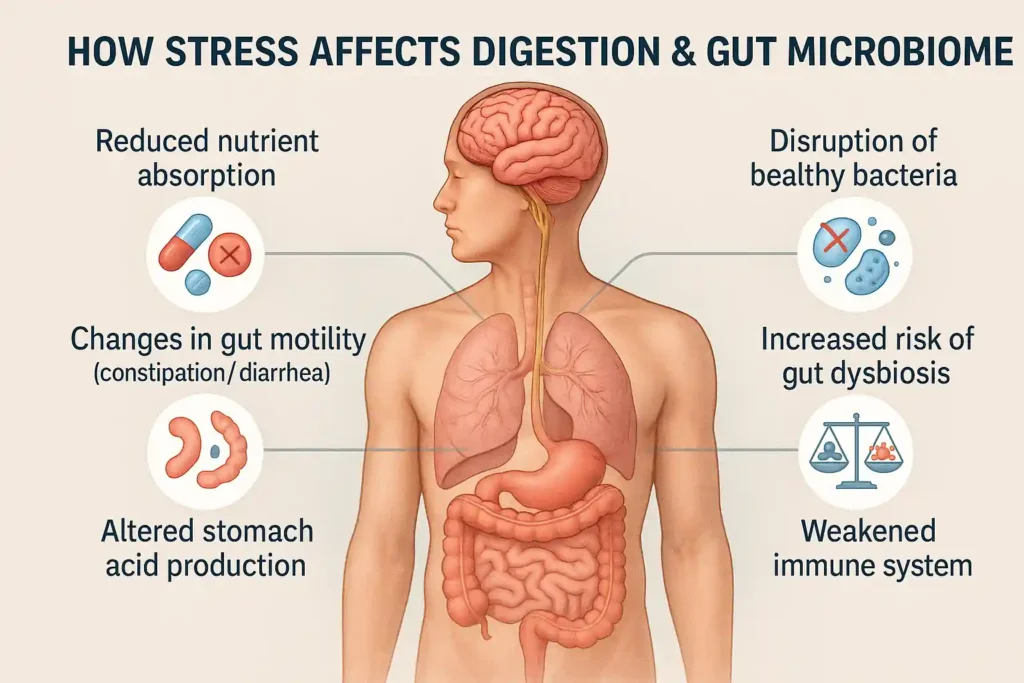
- Long-term stress increases inflammation in the gut lining, contributing to discomfort and digestive disorders.
- Stress weakens the intestinal barrier, increasing the risk of leaky gut and food sensitivities.
- Chronic cortisol exposure disrupts digestion and slows nutrient absorption.
- Ongoing stress affects microbiome balance, reducing beneficial bacteria involved in digestion, immunity, and hormone production.
- Persistent stress increases the risk of IBS, gut dysbiosis, and stress-induced digestive problems.
The Connection Between Stress and Digestion
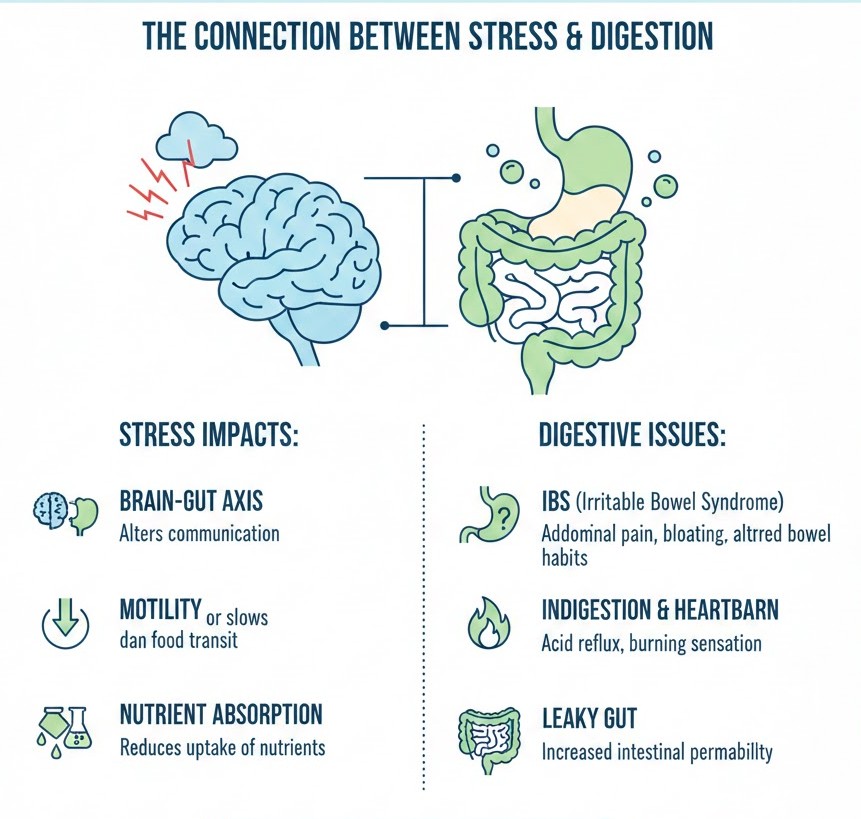
Understanding the connection between stress and digestion helps explain why your stomach reacts so strongly when your mind feels overwhelmed.
Stress changes digestion at multiple levels and interferes with every stage of the digestive process.
- Stress slows stomach emptying, causing fullness, pressure, and discomfort after eating.
- Stress reduces saliva and enzyme production, making digestion less efficient from the start.
- Cortisol interferes with the breakdown of fats, carbs, and proteins, creating digestive unease.
- Stress alters bowel movement patterns, creating constipation or diarrhea depending on gut response.
- Stress increases gut sensitivity, making normal digestion feel painful or exaggerated.
What Stress Does to Your Digestive System
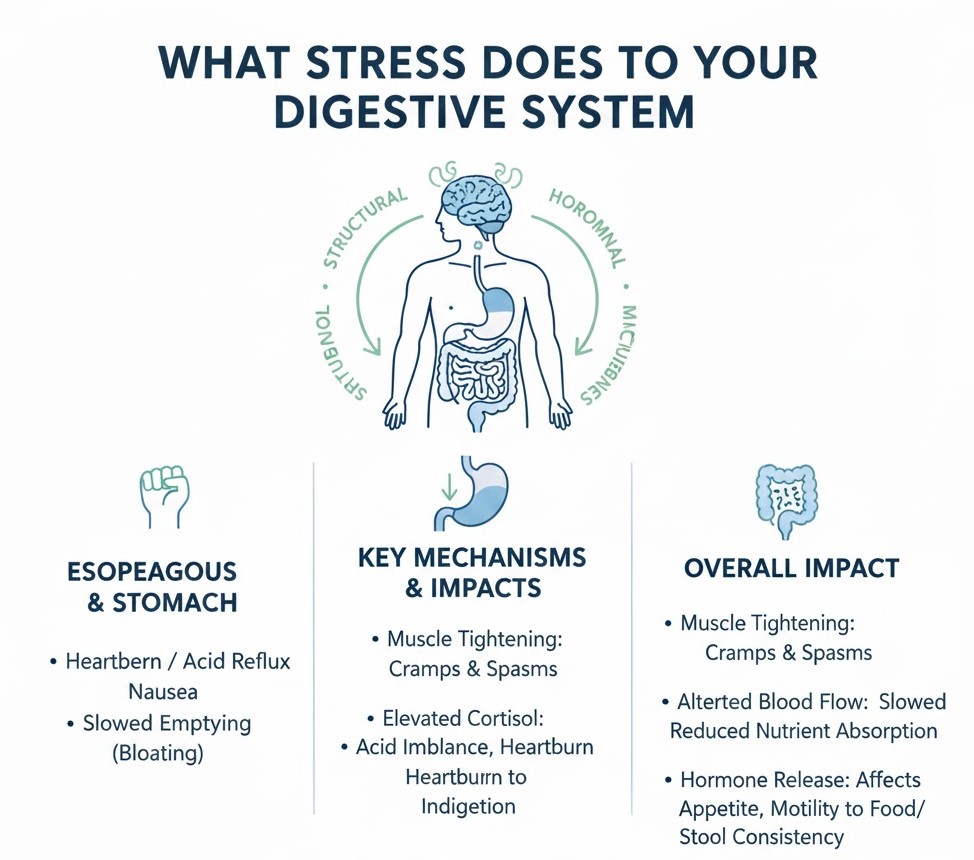
Stress does more than disrupt digestion; it physically changes gut function and shape over time. Stress creates structural, hormonal, and microbial changes.
- Stress tightens muscles in the stomach and intestines, creating cramps and spasms.
- Stress alters blood flow to the gut, slowing digestion and reducing nutrient absorption.
- Elevated cortisol disrupts stomach acid balance, increasing symptoms like heartburn or indigestion.
- Chronic stress increases nerve sensitivity in the intestines, making the gut overreact to food or stress triggers.
- Stress influences hormone release in the gut, affecting appetite, motility, and stool consistency.
How Stress Impacts Your Microbiome
The microbiome responds dramatically to stress. Beneficial gut bacteria support digestion, mood, immunity, and metabolic health, but stress disrupts this delicate balance.
Stress shifts the microbiome toward imbalance, inflammation, and reduced resilience.
- Stress reduces populations of beneficial gut bacteria, which weakens digestion and increases inflammation.
- Harmful bacteria gain the opportunity to grow when stress weakens microbial diversity.
- Stress-induced microbiome imbalance affects vitamin production, digestive enzyme availability, and gut healing.
- Emotional stress disrupts short-chain fatty acid production, which normally protects the gut lining.
- Lower microbial diversity increases the risk of digestive disorders and immune system dysregulation.
The Link Between Emotional Stress and Gut Issues
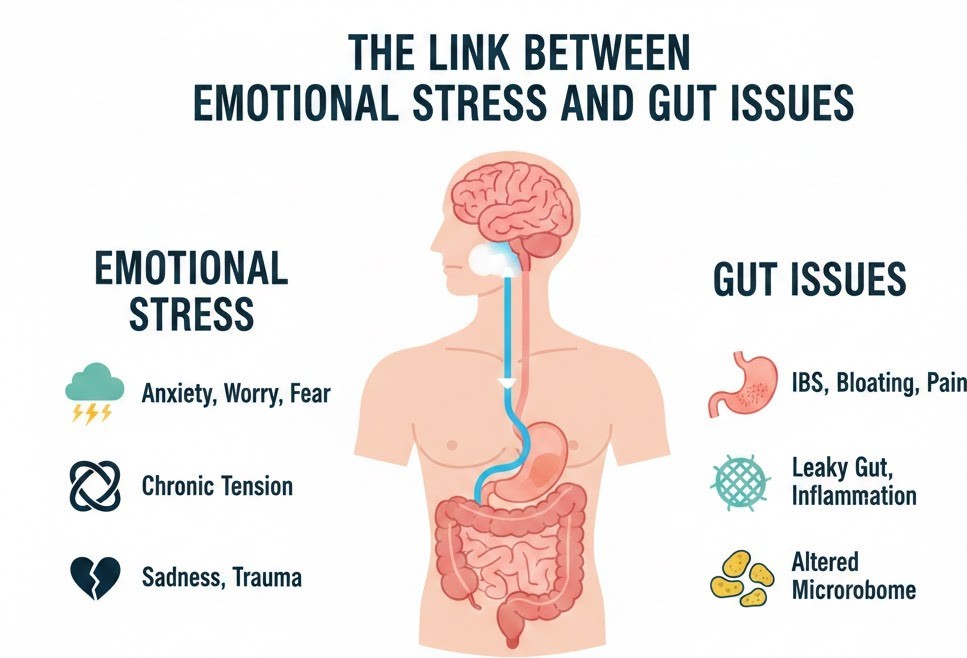
Emotional stress is one of the most common triggers of digestive discomfort. Negative emotions directly influence gut activity, gut bacteria, and the gut–brain axis.
Emotional stress affects digestion through nerves, hormones, and chemical messengers.
- Stress activates the sympathetic nervous system, which slows digestion and increases gut tension.
- Emotional stress heightens gut sensitivity, making mild digestive sensations feel uncomfortable.
- Stress influences serotonin, most of which is produced in the gut, altering bowel movement patterns.
- Emotional distress increases gut inflammation, worsening digestive symptoms.
- Anxiety and worry often worsen gut symptoms by creating a feedback loop between the brain and digestive system.
Stress-Induced Digestive Problems
Symptoms caused by stress can appear quickly or develop gradually over time. These stress-induced digestive problems are among the most common reasons people seek gut-health advice. These symptoms reflect how stress directly impacts gut and digestive processes.
- Constipation occurs when the stress response slows the colon and reduces motility.
- Diarrhea occurs when stress speeds up intestinal contractions and increases sensitivity.
- Bloating occurs when digestion slows and gas builds up due to reduced enzyme activity.
- Heartburn increases because stress disrupts stomach acid balance and tightens abdominal muscles.
- Abdominal pain appears when stress raises nerve sensitivity in the gut.
Cortisol and Digestion: Understanding the Stress Hormone
Cortisol is one of the main hormones linking stress and gut health. It affects motility, inflammation, enzyme production, and microbial balance. Cortisol has widespread influence on digestive function.
- Elevated cortisol slows digestion, contributing to feelings of heaviness after meals.
- Chronic cortisol reduces stomach acid, impairing nutrient breakdown and absorption
- High cortisol increases gut inflammation, worsening symptoms such as cramping or discomfort
- Cortisol suppresses beneficial gut bacteria, creating microbiome imbalance from stress.
- Ongoing cortisol release worsens digestive efficiency and contributes to long-term gut issues.
The Gut-Brain Axis and Stress
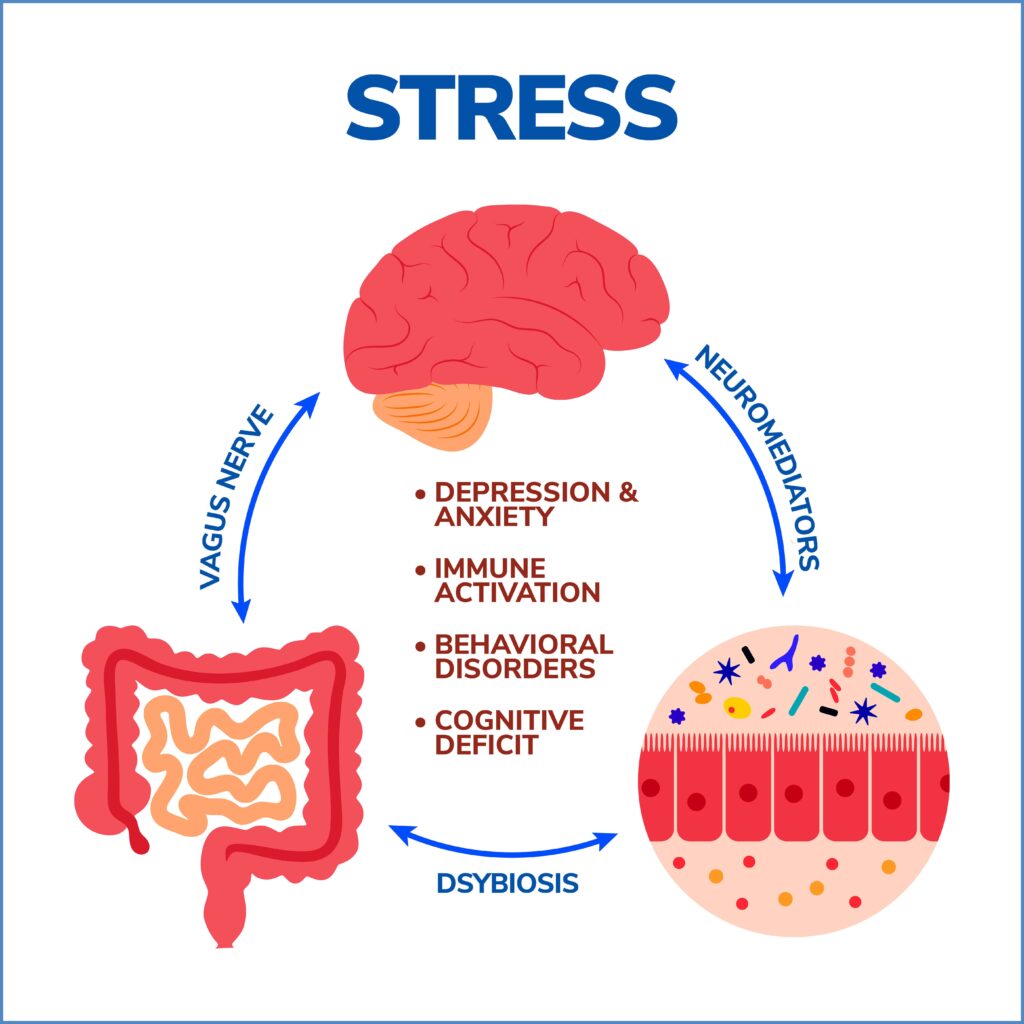
The gut and brain communicate constantly. When one becomes imbalanced, the other responds. Stress disrupts this communication and contributes to chronic gut symptoms. Stress affects neurotransmitters, nerves, and microbial signals that connect the gut and brain.
- Stress alters vagus nerve activity, reducing communication between the gut and brain.
- Stress disrupts neurotransmitter production, especially serotonin and GABA, which regulate digestion.
- Microbiome imbalance from stress interferes with gut–brain signaling.
- Emotional stress triggers inflammation that spreads through the gut–brain axis.
- Disrupted gut–brain communication increases the likelihood of stress-induced digestive problems.
Protecting Your Gut During Stress
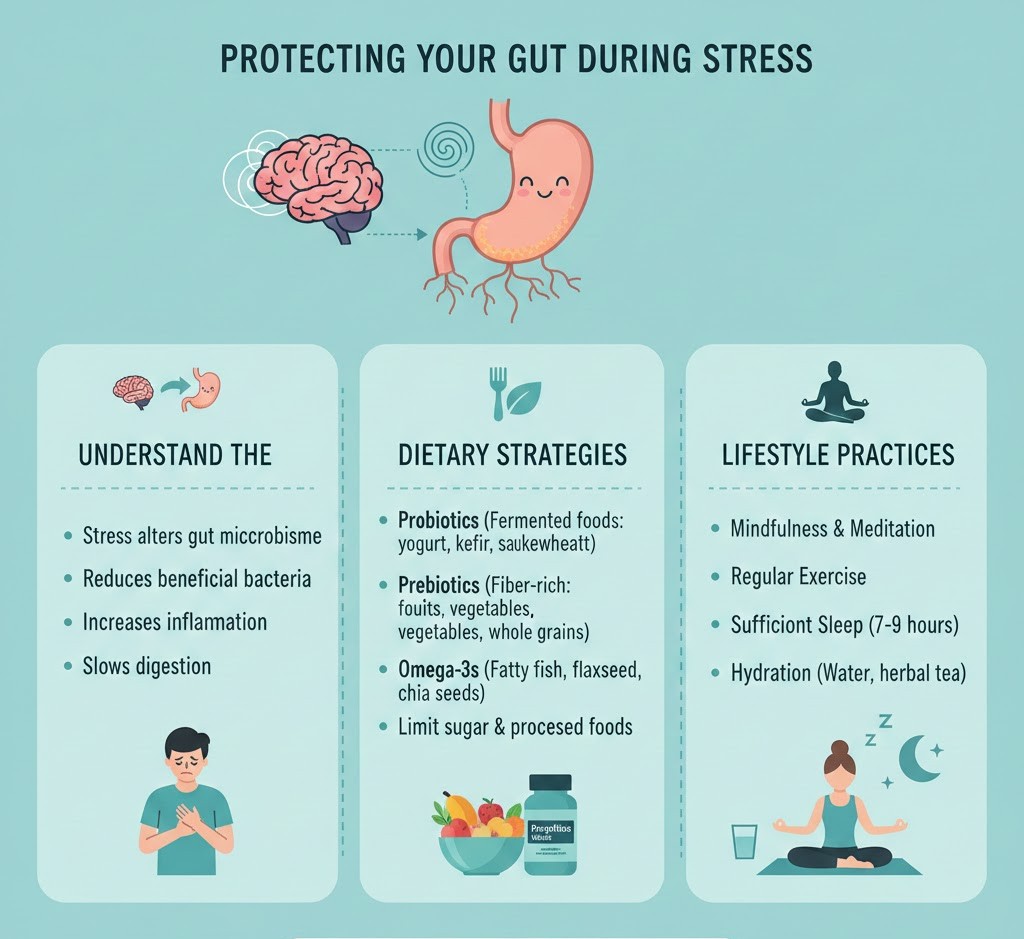
Managing stress is essential for long-term digestive stability, microbiome balance, and overall gut health. These evidence-based strategies help reduce the effects of stress on digestion.
- Regular deep breathing activates the parasympathetic nervous system, improving digestion.
- Eating slowly reduces digestive strain and improves nutrient absorption.
- Prioritizing whole, fiber-rich foods helps maintain microbiome balance and reduce inflammation.
- Limiting caffeine and sugar reduces nervous system overstimulation and prevents additional gut irritation.
- Gentle movement such as walking or yoga helps regulate the gut–brain axis and reduce cortisol.
Conclusion
Understanding How Stress Influences Your Gut helps explain why emotional stress often leads to digestive discomfort, microbiome imbalance, and long-term gut issues. Stress affects your gut health by altering motility, hormone balance, microbial composition, inflammation levels, and gut–brain communication. By managing stress, supporting the microbiome, and practicing gut-friendly habits, you can significantly improve digestion and protect your long-term gut health.
FAQs
Can stress really affect your gut health?
Yes, stress can strongly affect your gut health because the gut–brain axis reacts instantly to stress signals. This can change digestion, hormone levels, and the balance of good and bad bacteria in your gut. Over time, this can lead to symptoms like bloating, discomfort, or irregular bowel movements.
Why does stress cause digestive problems?
Stress causes digestive problems by slowing down gut motility, reducing important digestive enzymes, and increasing inflammation in the gut lining. These changes make it harder for your body to break down food properly, which can lead to gas, pain, or stomach discomfort.
How does cortisol interfere with digestion?
Cortisol, the body’s main stress hormone, interferes with digestion by slowing stomach emptying, lowering stomach acid levels, and throwing off the balance of your gut microbiome. This makes it harder for your digestive system to function smoothly, especially during long periods of stress.
Can emotional stress make gut symptoms worse?
Yes, emotional stress can make gut symptoms worse because it increases your gut’s sensitivity. This means normal digestive sensations may feel more intense or painful, leading to issues like cramps, bloating, or stomach tightness.
Does stress impact the gut microbiome?
Stress does impact the microbiome by reducing beneficial bacteria, increasing harmful microbes, and lowering overall microbial diversity. When the microbiome becomes unbalanced, digestion, immunity, and nutrient absorption can all be affected.
Why do I get diarrhea or constipation when stressed?
Stress affects colon motility, causing it to speed up in some people—leading to diarrhea—or slow down in others, which leads to constipation. These rapid shifts happen because stress hormones disrupt the gut’s normal rhythm.
Can stress cause bloating?
Yes, stress can cause bloating because it slows digestion, causes gas to build up, and reduces enzyme activity needed for proper food breakdown. Stress also makes the gut more sensitive, so mild bloating may feel worse.
Is long-term stress harmful to gut health?
Long-term stress is harmful because it increases gut inflammation, weakens the intestinal barrier, and disrupts digestion over time. This can contribute to chronic issues such as IBS, acid reflux, or persistent stomach discomfort.
Can managing stress improve digestion?
Yes, managing stress can improve digestion by restoring normal gut motility, lowering inflammation, and supporting a healthier balance of microbes. Techniques like deep breathing, exercise, and proper sleep can make a noticeable difference.
Does anxiety affect the gut the same way as stress?
Anxiety affects the gut in a similar way to stress because it activates the same nervous system pathways, including the fight-or-flight response. This can disrupt digestion, increase sensitivity, and trigger symptoms like nausea, diarrhea, or stomach tightness.
References
- Harvard Medical School – The gut–brain connection
https://www.health.harvard.edu/diseases-and-conditions/the-gut-brain-connection - Cleveland Clinic – How stress affects digestion
https://health.clevelandclinic.org/why-stress-causes-digestive-problems - American Psychological Association – Stress and the gut https://www.apa.org/monitor/2012/09/gut-feeling
- National Institute of Diabetes and Digestive and Kidney Diseases – Digestive health
https://www.niddk.nih.gov/health-information/digestive-diseases - Johns Hopkins Medicine – The microbiome and gut health
https://www.hopkinsmedicine.org/health/wellness-and-prevention/the-microbiome
Dr. Emily Zhang, MD, is a gastroenterologist and integrative medicine specialist with 10 years of clinical experience in digestive health and microbiome science. She completed her medical degree at University of Chicago Pritzker School of Medicine and fellowship at Massachusetts General Hospital. Dr. Zhang specializes in gut-brain interactions, microbiota diversity, and nutrition-driven gut repair. She has contributed to NIH-funded studies on probiotics and authored patient education resources on functional gut disorders.

