Menopause brings hormonal changes that can impact the urinary system, increasing the risk of infections, bladder sensitivity, and incontinence. Following practical daily habits, home remedies, and lifestyle changes, including key urinary tract health tips after menopause, can help support bladder function and enhance overall wellness for women over 50.
Key Takeaways
- Hormonal changes in menopause can weaken bladder tissues and increase infection risk.
- Practicing postmenopausal bladder care and menopause urinary care tips helps maintain bladder comfort.
- Simple habits like proper hydration, pelvic floor therapy, and bladder-friendly daily routines reduce urinary challenges post-menopause.
- Diet, lifestyle adjustments, and probiotics support mature women’s urinary tract health naturally.
- Regular medical checkups ensure early detection of issues and complement home remedies for urinary wellness after 50.
Understanding Urinary Health After Menopause
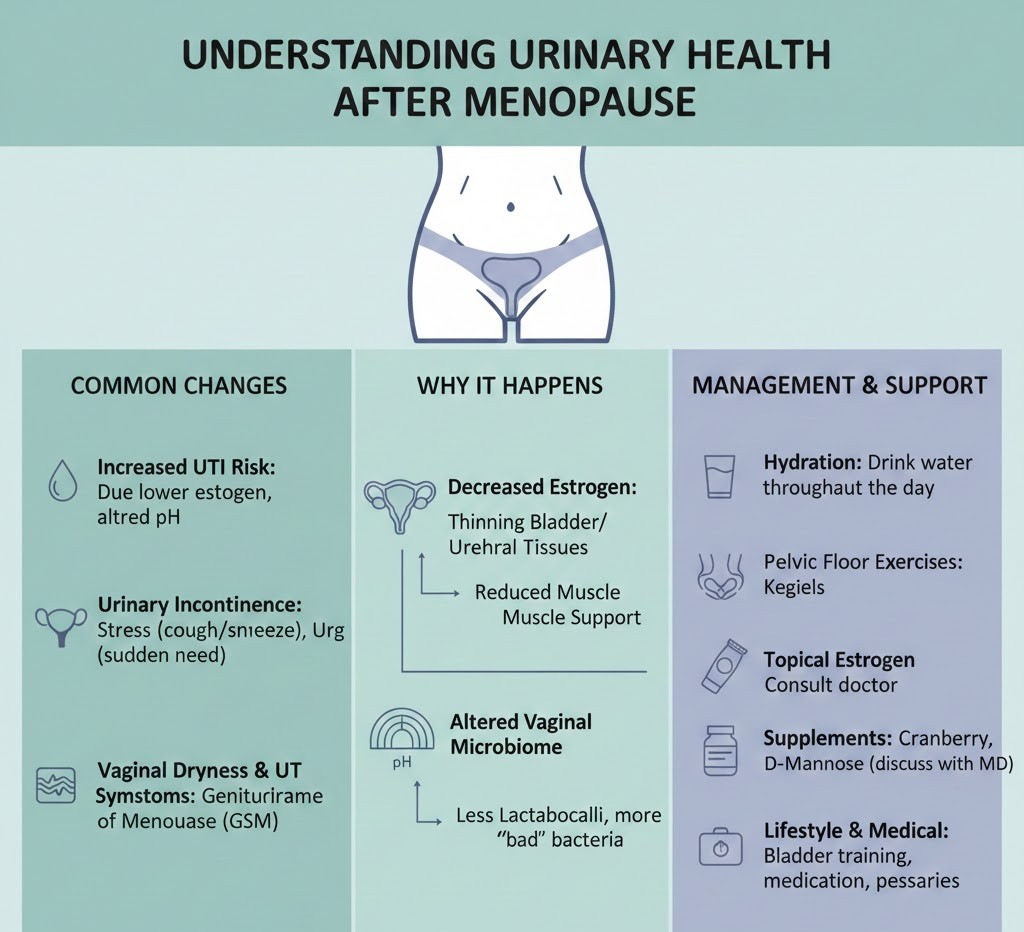
After menopause, declining estrogen levels significantly affect the urinary tract, leading to changes that many women are not prepared for. Estrogen normally helps maintain the strength, moisture, and elasticity of the bladder and urethral tissues. When these hormone levels drop, the urinary tract becomes more vulnerable to irritation, dryness, and bacterial infections. This is why issues such as urgency, frequent urination, burning sensations, and recurrent UTIs in postmenopause become more common. These hormonal shifts also influence the vaginal area, making vaginal dryness and UTIs closely connected for many mature women.
In addition to hormonal changes, aging naturally weakens pelvic floor muscles, which can lead to incontinence after menopause, reduced bladder control, and nighttime urination known as nocturia. These changes create common urinary challenges post-menopause, highlighting the importance of adopting proper bladder care routines. Understanding these factors helps women embrace effective urinary tract health tips after menopause, including pelvic floor therapy, proper hydration, probiotics, and lifestyle adjustments. With proactive care, urinary wellness after 50 is absolutely achievable.
Why Menopausal Women Need to Worry About Urinary Health
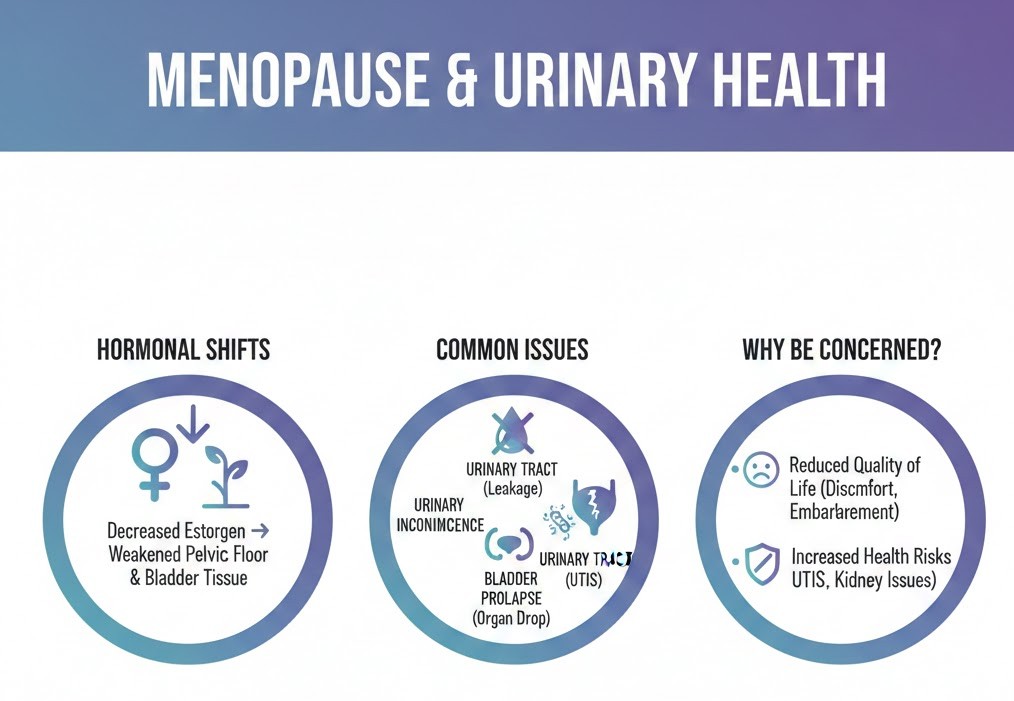
Menopausal women face increased urinary challenges because the drop in estrogen affects the bladder, urethra, and pelvic floor, making the urinary system more sensitive and prone to infections. As hormone levels decline, several changes occur that raise the risk of long-term urinary issues, which is why paying attention to bladder health becomes essential.
- Low estrogen levels thin the tissues of the bladder and urethra, causing dryness and irritation.
- Weak pelvic floor muscles reduce bladder control and may lead to leakage.
- Changes in vaginal flora decrease protective good bacteria, increasing UTI risk.
- Incomplete bladder emptying becomes more common, encouraging bacterial growth.
- Reduced immunity with age makes it harder for the body to fight urinary infections.
Common Urinary Problems After Post-Menopause
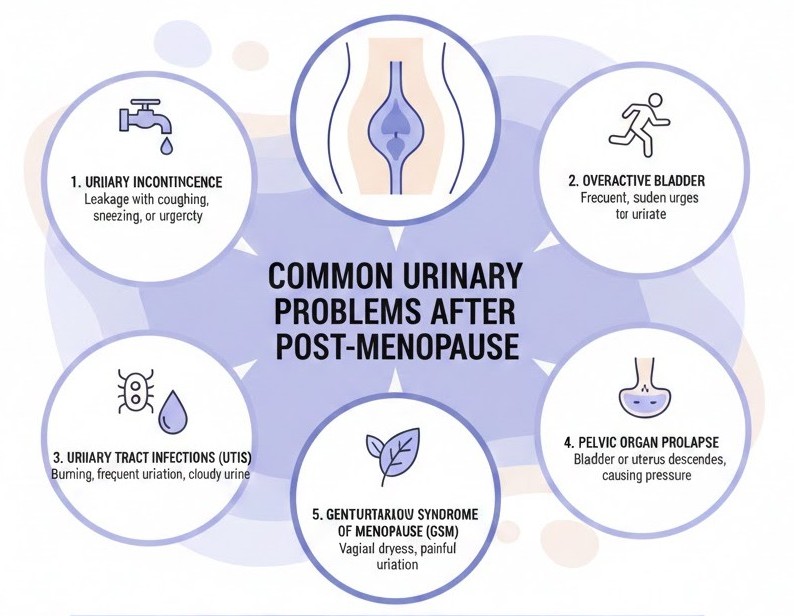
Urinary challenges after post-menopause occur due to hormonal changes, weakened pelvic tissues, and age-related factors, making it important to understand the root causes.
- Low Estrogen Levels: Declining estrogen weakens the bladder and urethral lining, leading to irritation and urinary discomfort.
- Weakened Pelvic Floor Muscles: Reduced muscle strength can cause leakage, especially during coughing, laughing, or lifting.
- Increased UTI Risk: Thinner vaginal and urethral tissues make infections more common and harder to prevent.
- Overactive Bladder: Sudden strong urges to urinate and frequent trips to the bathroom become more likely.
- Vaginal Dryness & Atrophy: Tissue thinning and dryness contribute to burning, urgency, and overall urinary irritation.
How to Reduce Your Risks of UTIs After Menopause
Lowering your risk of urinary tract infections after menopause is essential for long-term comfort, bladder health, and overall well-being. Hormonal changes make the urinary tract more vulnerable, but adopting simple daily habits can significantly improve protection and reduce recurring infections.
- Support Vaginal and Urinary Tissue Health: Using doctor-recommended vaginal estrogen can strengthen the vaginal walls, restore natural moisture, and promote healthy bacteria greatly lowering UTI risk. Maintaining hydration and choosing bladder-friendly foods also keep the urinary tract flushed and balanced.
- Improve Bladder Emptying: Taking time to fully empty your bladder helps prevent bacteria from multiplying. Practicing pelvic floor exercises strengthens the bladder muscles, improves control, and reduces leftover urine that can lead to infections.
- Boost Natural Immunity: A healthy immune system helps the body fight off harmful bacteria. Eating probiotic-rich foods, staying active, and managing stress naturally support urinary defenses. Many postmenopausal women also benefit from supplements like D-mannose or cranberry extract (with medical guidance).
- Maintain Good Hygiene Practices: Wiping front to back, avoiding harsh soaps, and wearing breathable cotton underwear prevent irritation and bacterial spread. Urinating after sexual activity also helps flush out bacteria before they cause infection.
- Stay Consistently Hydrated: Drinking enough water dilutes urine and helps wash out harmful bacteria, reducing infection risk. Adequate hydration also prevents irritation and supports overall urinary wellness after menopause.
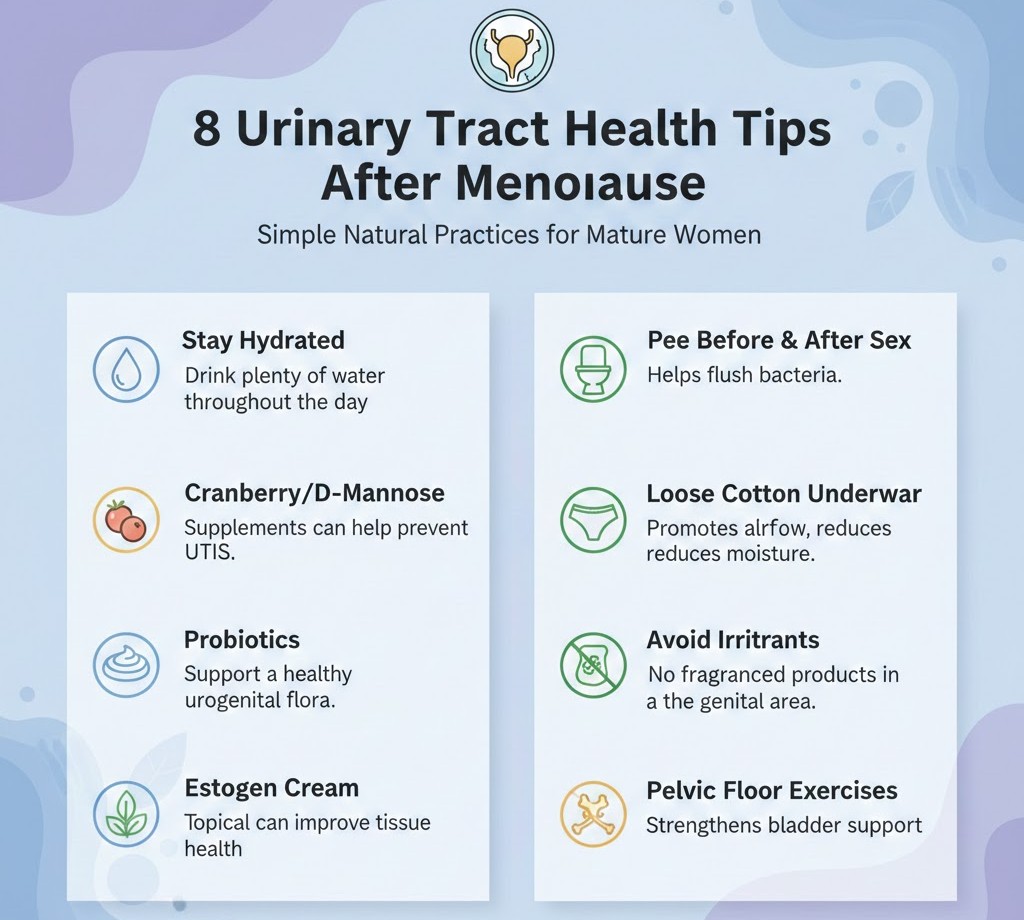
8 Urinary Tract Health Tips After Menopause
After menopause, changes in hormone levels, particularly decreased estrogen, can make the urinary tract more susceptible to infections, irritation, and bladder control issues. Women may experience dryness, increased urgency, or recurrent urinary tract infections (UTIs) during this stage of life. Following these urinary tract health tips after menopause can help maintain bladder comfort, reduce infection risks, and support long-term urinary wellness. Incorporating these practices into daily routines strengthens bladder function, supports overall urinary system health, and improves quality of life.
1. Stay Hydrated

Drinking sufficient water is one of the simplest and most effective ways to maintain urinary health after menopause. Adequate hydration helps flush bacteria and toxins from the urinary tract, dilutes urine, and prevents urinary irritation or kidney stones. Herbal teas without caffeine, such as chamomile, peppermint, or fennel tea, can provide hydration while soothing the bladder and reducing inflammation. Staying hydrated also supports the body’s natural detoxification processes, improves circulation, and keeps urinary tract tissues healthy.
Tips for Staying Hydrated:
- Drink at least 8–10 glasses of water daily.
- Include water-rich fruits like watermelon, cucumber, oranges, and berries.
- Consume herbal teas and infused water to maintain hydration.
- Limit sugary drinks, caffeinated beverages, and sodas that can irritate the bladder.
2. Practice Good Hygiene

Maintaining proper hygiene is essential to prevent bacterial infections and irritation, which become more common after menopause due to hormonal changes. Gentle cleansing, correct wiping techniques, and breathable clothing create a protective environment for the urinary tract. Avoiding harsh soaps or chemical washes prevents irritation, while timely changing of wet clothing, especially after exercise or swimming, reduces bacterial growth and helps maintain comfort.
Practical Hygiene Steps:
- Wipe from front to back to prevent bacterial contamination.
- Use mild, fragrance-free soap or hypoallergenic wipes.
- Wear clean, breathable cotton underwear and loose clothing.
- Change wet swimsuits, sweaty workout clothes, or damp garments promptly to avoid bacterial proliferation.
3. Strengthen Pelvic Floor Muscles
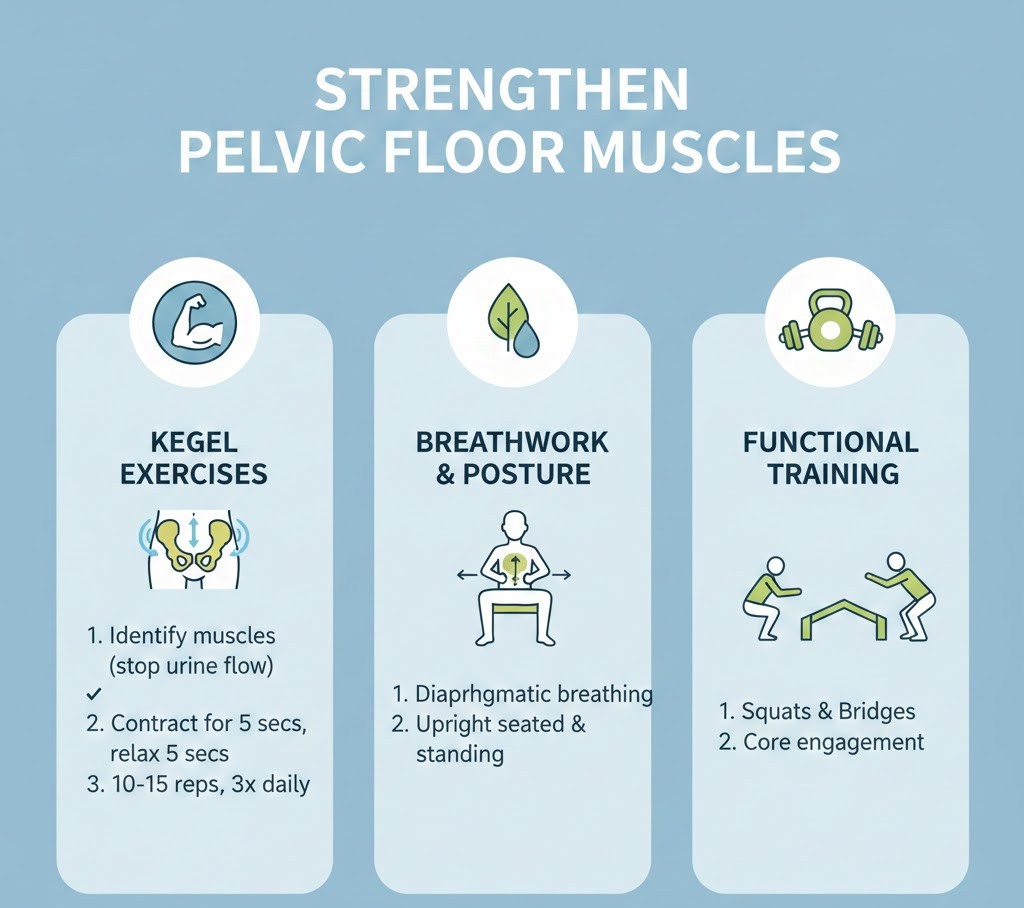
Pelvic floor muscles tend to weaken with age and hormonal changes, which can lead to bladder leakage, urgency, or reduced urinary control. Regular pelvic floor exercises, such as Kegel exercises, help strengthen these muscles, improve bladder support, and enhance overall urinary function. Strengthening these muscles can also reduce the severity of incontinence, improve sexual health, and enhance core stability. Women can also benefit from guided pelvic floor therapy if they experience significant weakness or recurrent urinary issues.
Pelvic Floor Tips:
- Perform daily Kegel exercises for at least 5–10 minutes.
- Incorporate light stretching or yoga to increase pelvic circulation and flexibility.
- Consult a physiotherapist or pelvic health specialist for personalized exercises.
- Combine pelvic floor exercises with a healthy diet and hydration for better results.
4. Monitor Diet and Avoid Bladder Irritants
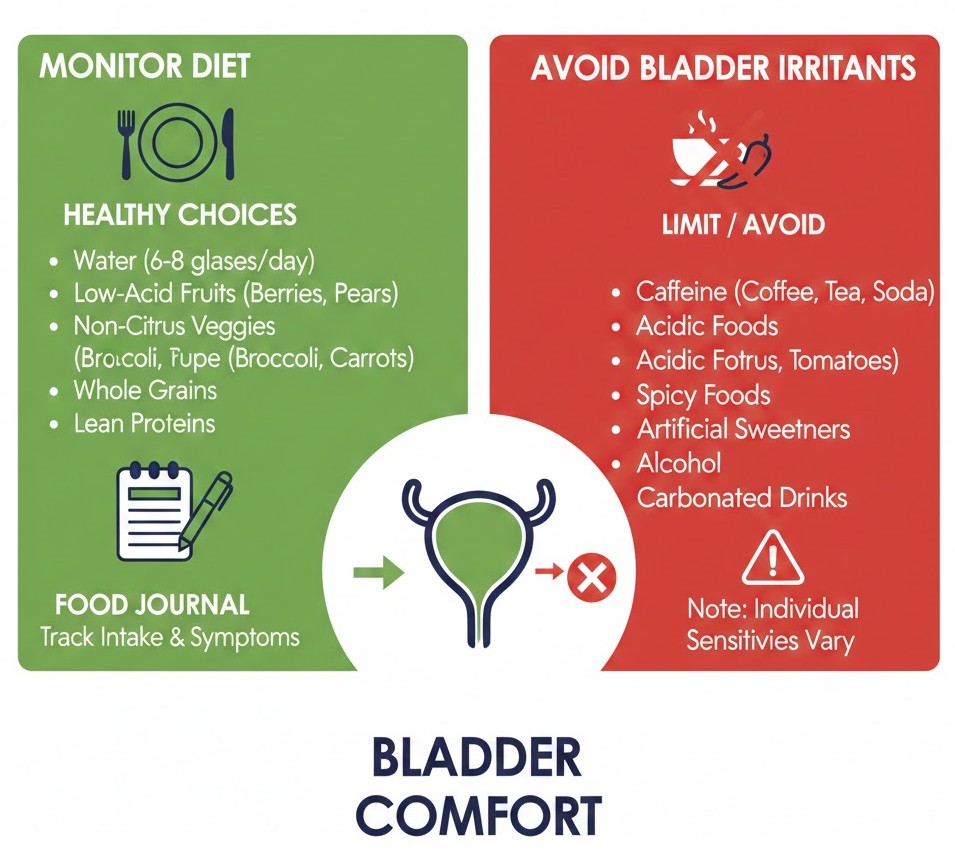
Certain foods and beverages can irritate the bladder, increase urgency, or worsen incontinence. Limiting bladder irritants while including urinary-friendly foods can significantly reduce postmenopausal urinary discomfort and lower the risk of recurrent UTIs. Foods like cranberries and blueberries contain compounds that help prevent harmful bacteria from adhering to the urinary tract. Eating a nutrient-rich, anti-inflammatory diet strengthens immunity, reduces inflammation, and promotes overall urinary tract health.
Diet Tips:
- Limit caffeine, alcohol, carbonated beverages, and highly acidic or spicy foods.
- Include cranberry juice, blueberries, and other antioxidant-rich fruits to prevent infections.
- Focus on a diet rich in vegetables, leafy greens, whole grains, and lean proteins.
- Avoid processed foods, excess sugar, and artificial sweeteners that can irritate the bladder.
5. Consider Hormonal Support
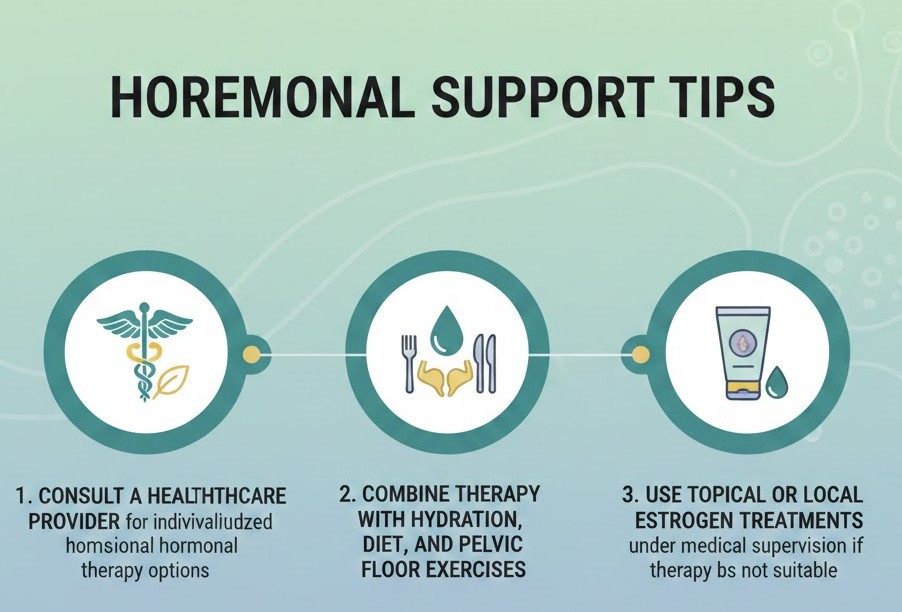
Vaginal estrogen therapy, prescribed by a healthcare professional, can restore urinary tissue health and improve bladder support. Reduced estrogen levels after menopause contribute to thinning of the urethral and vaginal tissues, increasing susceptibility to infections and dryness. Hormonal support can relieve these symptoms, improve bladder function, and reduce discomfort during urination. Women considering therapy should discuss benefits and risks with their doctors to ensure safe and effective treatment.
Hormonal Support Tips:
- Consult a healthcare provider for individualized hormonal therapy options.
- Combine therapy with hydration, diet, and pelvic floor exercises.
- Use topical or local estrogen treatments under medical supervision if systemic therapy is not suitable.
6. Incorporate Probiotics
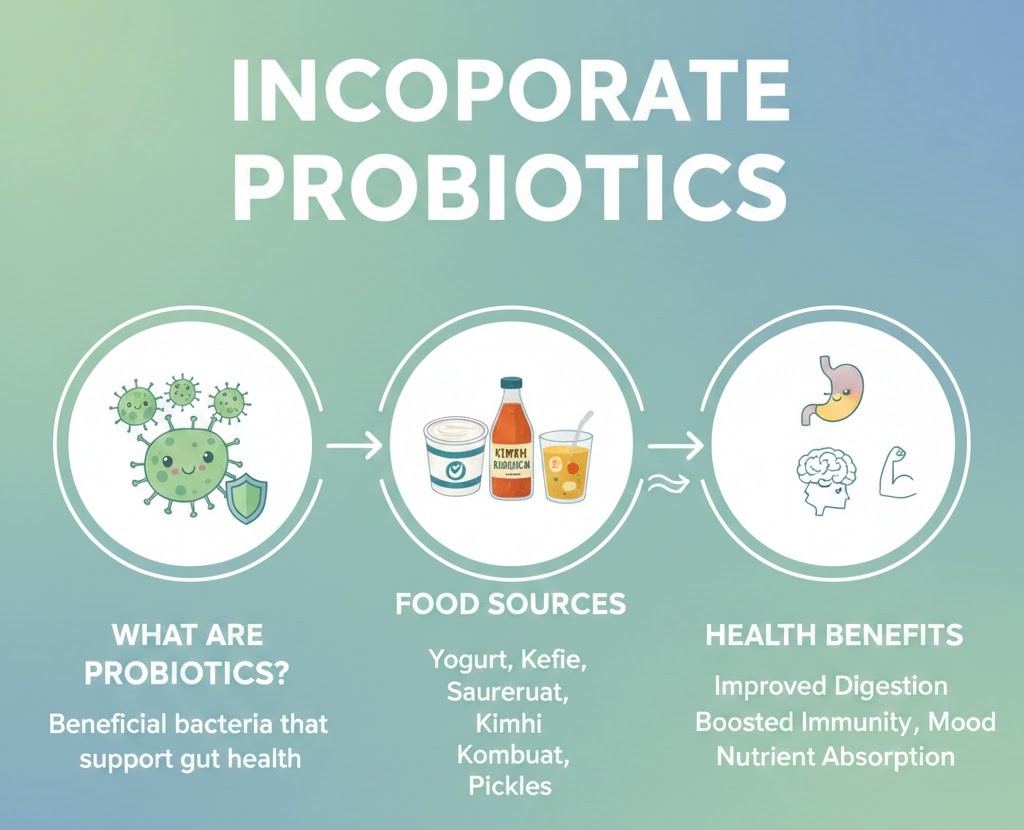
Probiotics help maintain a healthy balance of bacteria in the gut and urinary tract, which strengthens natural defenses against infections. Postmenopausal women may experience changes in microbiota due to hormonal shifts, making probiotic support even more important. Regular consumption of probiotic-rich foods or supplements can reduce the risk of recurrent UTIs, support immune function, and improve overall digestive and urinary wellness.
Probiotic Tips:
- Include yogurt, kefir, fermented vegetables, or probiotic supplements.
- Discuss with your healthcare provider before starting high-dose supplements.
- Maintain a balanced diet to support probiotic efficacy.
7. Maintain Regular Medical Checkups
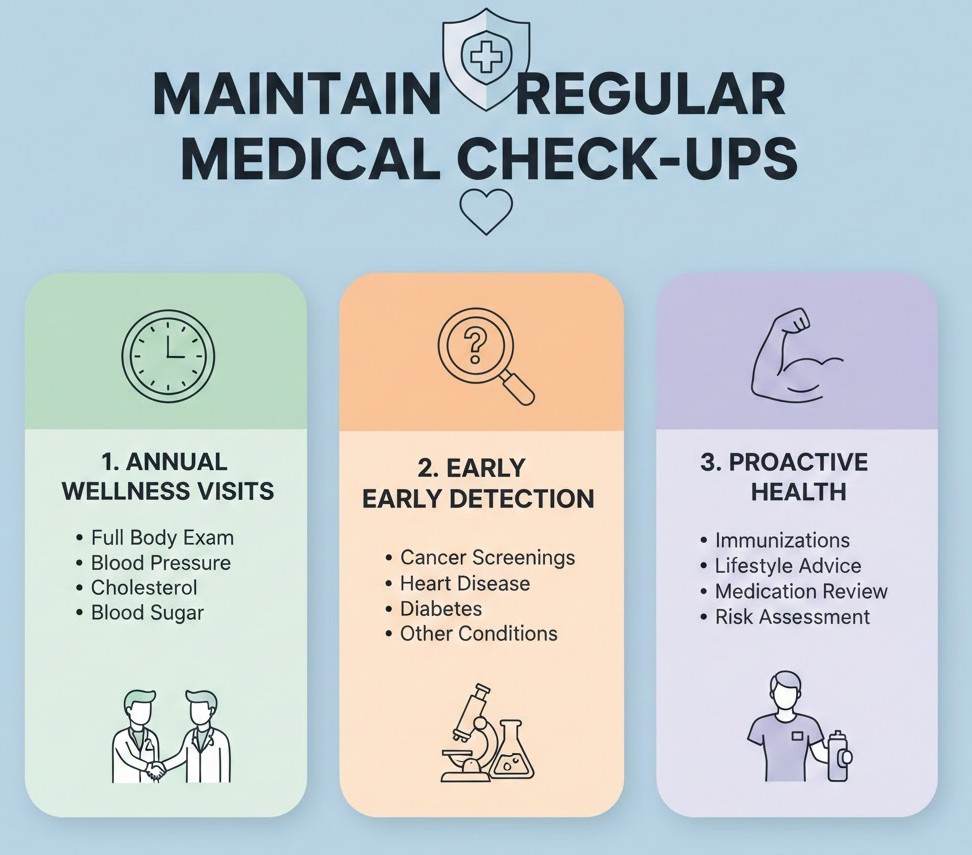
Routine medical visits help detect urinary challenges early, allowing timely treatment and preventing complications. Doctors may recommend urine tests, pelvic examinations, or imaging studies to monitor urinary tract health after menopause. Regular checkups are also an opportunity to discuss lifestyle modifications, preventive strategies, and therapies that improve bladder function and reduce infection risks.
Checkup Tips:
- Schedule periodic urinary health evaluations.
- Discuss any changes in urination patterns, discomfort, or leakage with your doctor.
- Follow medical guidance for preventive care, including vaccines or supplements if recommended.
8. Respond to Urinary Urges Promptly
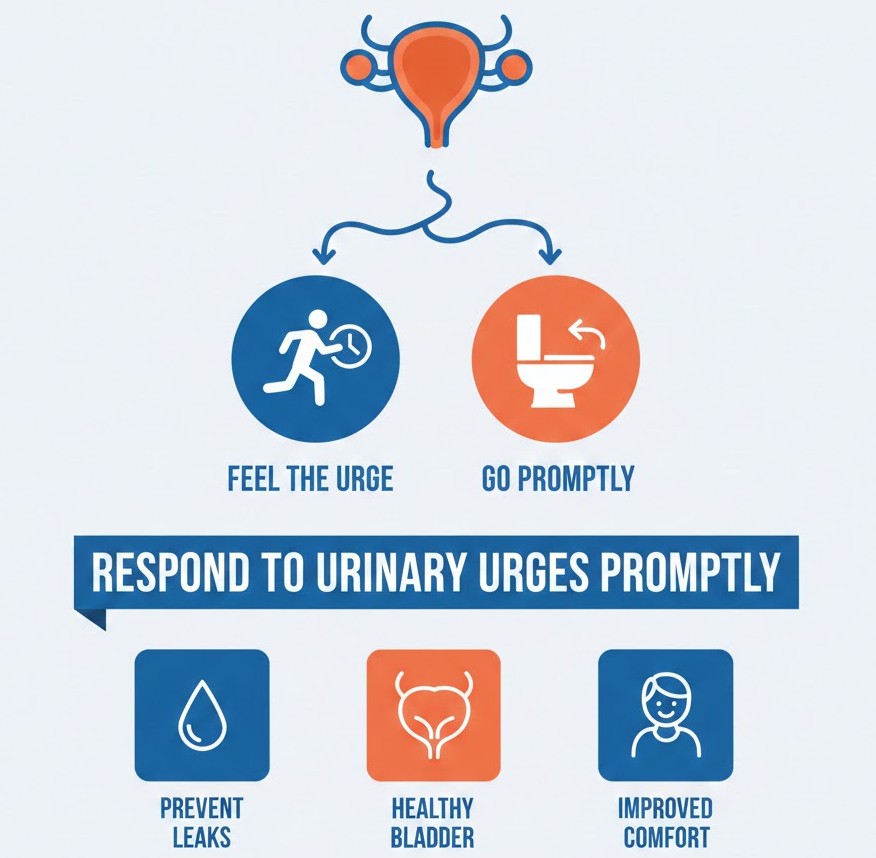
Delaying urination for long periods can encourage bacterial growth, weaken bladder muscles, and increase discomfort. Responding promptly to the urge to urinate helps maintain bladder tone, prevent overdistension, and reduce the risk of infections. Establishing regular bathroom routines also supports long-term bladder health and prevents unnecessary urinary complications.
Urination Tips:
- Aim to urinate every 3–4 hours during the day.
- Avoid holding urine for long periods.
- Encourage consistent bathroom habits in daily routines to maintain bladder health.
Lifestyle Adjustments for Postmenopausal Urinary Wellness
After menopause, hormonal changes and aging can weaken the bladder and pelvic floor muscles, increasing the risk of urinary tract infections, incontinence, and bladder discomfort. Making simple lifestyle adjustments can help maintain urinary health, strengthen bladder function, and reduce urinary challenges. Incorporating daily habits, diet modifications, exercise, and proper routines can support long-term urinary wellness and improve overall quality of life for postmenopausal women.
- Stay Active: Low-impact exercises like walking, yoga, or swimming support pelvic floor strength, improve circulation, and reduce stress-related urinary urgency.
- Maintain Healthy Weight: Managing weight through diet and exercise reduces pressure on the bladder and pelvic muscles, lowering incontinence risk.
- Limit Bladder Irritants: Reduce caffeine, alcohol, carbonated, spicy, or acidic foods to prevent bladder irritation and promote comfort.
- Follow a Bathroom Routine: Urinate regularly and respond promptly to urges to maintain bladder muscle tone and prevent bacterial growth.
- Practice Pelvic Floor Therapy: Daily Kegel exercises or guided pelvic floor therapy strengthen bladder-supporting muscles, improving urinary control and reducing leakage.
- Balance Sleep and Hydration: Adequate sleep and proper daytime hydration support immunity, flush bacteria, and reduce nighttime urination.
When to Seek a Doctor
While lifestyle adjustments and home remedies can greatly improve urinary wellness after menopause, it’s important to recognize warning signs that require professional medical attention. Timely intervention helps prevent complications, detect underlying issues, and ensure proper treatment.
Seek medical advice if you experience:
- Persistent burning or pain during urination.
- Frequent urges to urinate, sudden urinary urgency, or leakage.
- Cloudy, foul-smelling, or bloody urine.
- Lower abdominal, pelvic, or back pain.
- Fever, chills, or nausea, which may indicate kidney involvement.
- Sudden worsening of incontinence or inability to fully empty the bladder.
- Recurrent urinary tract infections despite home care measures.
Conclusion
After menopause, lower estrogen weakens the bladder and pelvic floor, increasing risks of UTIs, incontinence, and irritation. Staying hydrated, practicing good hygiene, and strengthening pelvic floor muscles with Kegels support urinary health. Avoiding bladder irritants like caffeine, alcohol, and spicy foods, along with consuming cranberry, blueberry, and probiotic-rich foods, helps maintain bladder comfort. Vaginal estrogen therapy under medical guidance can restore tissue health, while regular checkups, exercise, balanced sleep, and weight management further support long-term urinary wellness. Seek a doctor if you experience persistent pain, burning, cloudy or bloody urine, frequent urgency, or recurrent infections.
FAQs
Why does menopause increase urinary problems?
Menopause lowers estrogen levels, which thins bladder and urethral tissues, weakens pelvic floor muscles, and reduces protective vaginal bacteria, increasing the risk of infections, irritation, and incontinence.
How can I prevent urinary tract infections (UTIs) after menopause?
Drink plenty of water, practice good hygiene, strengthen pelvic floor muscles, avoid bladder irritants, consume cranberry or blueberry products, and consider doctor-recommended vaginal estrogen or probiotics.
What are common urinary issues after menopause?
Frequent urination, urgency, bladder leakage, recurrent UTIs, overactive bladder, and vaginal dryness or irritation are common postmenopausal urinary problems.
How does hydration help urinary health?
Adequate water intake flushes out bacteria, dilutes urine, reduces irritation, and helps maintain bladder and kidney function. Herbal teas without caffeine also soothe the urinary tract.
What role do pelvic floor exercises play?
Kegel exercises and guided pelvic floor therapy strengthen bladder-supporting muscles, improve control, reduce leakage, and enhance overall urinary function.
Which foods and drinks should I avoid for bladder health?
Limit caffeine, alcohol, carbonated drinks, spicy or acidic foods, and artificial sweeteners, as they can irritate the bladder and worsen incontinence.
Can probiotics help postmenopausal urinary health?
Yes, probiotics maintain healthy gut and urinary tract bacteria, strengthen natural defenses against infections, and support immune function.
When should I seek medical attention?
Consult a doctor if you experience persistent burning, pain, cloudy or bloody urine, frequent urgency, leakage, pelvic pain, fever, or recurrent UTIs despite home care.
How can lifestyle changes improve urinary wellness?
Regular exercise, weight management, balanced sleep, hydration, avoiding irritants, and following a bathroom routine strengthen bladder muscles and reduce infection risk.
Is vaginal estrogen therapy safe for urinary health?
Under medical guidance, vaginal estrogen can restore tissue health, reduce dryness, improve bladder support, and lower UTI risk, complementing lifestyle and home remedies.
References
- How to Maintain Bladder Health During Menopause: Tips for Staying Healthy. (2025, January 10). Criticare Hospital. Retrieved December 12, 2025, from https://www.criticarehospital.co.in/how-to-maintain-bladder-health-during-menopause-tips-for-staying-healthy/
- Kate Labat Jacobs. (2025, August 4). How Menopause Impacts Urinary Tract Health. Uqora. Retrieved December 12, 2025, from https://uqora.com/blogs/urinary-tract-infections/how-menopause-impacts-urinary-tract-health?srsltid=AfmBOopFhyuW-5IzwOzTeF-hYkHoNb49-VRiGyEs7szSaqeTnCO0y5jH
- Menopause and UTIs: Understanding the Link. (2025, October 8). Evvy. Retrieved December 14, 2025, from https://www.evvy.com/blog/menopause-and-utis
- UTIs Are More Common After Menopause: Here’s What You Can Do. (n.d.). Advanced Urogynecology. Retrieved December 12, 2025, from https://www.advancedurogynecology.com/blog/utis-are-more-common-after-menopause-heres-what-you-can-do
Eryn Ellison is a PharmD with 8 years in hospital and ambulatory care. A graduate of the UNC Eshelman School of Pharmacy (2017), Eryn completed a PGY-1 Pharmacy Residency at Cleveland Clinic and holds BCPS certification from the Board of Pharmacy Specialties. They evaluate supplement efficacy, safety, and interactions with common prescriptions. Eryn has authored formulary reviews for P&T committees and consults on deprescribing protocols within large health systems. Credentials: state pharmacist license, BCPS ID, and professional profiles.

