Testosterone, though often labeled a male hormone, is vital for women’s strength, mood, energy, sexual health, and bone density. Both low and high levels disrupt hormonal balance, causing symptoms like fatigue, low libido, or unwanted hair growth. Early recognition and proper management are essential for long-term well-being.
Key Takeaways
- Normal female testosterone levels range from 15–70 ng/dL (younger women) and drop with age or menopause.
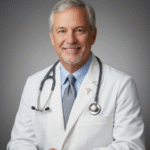
- Low testosterone causes fatigue, weak muscles, mood decline, low libido, and bone loss.
- High testosterone commonly results from PCOS, adrenal disorders, or tumors.
- Hormone testing (total/free T, LH, FSH, DHEA) confirms imbalance and guides treatment.
- Birth control or anti-androgen therapy lowers high testosterone; hCG or careful TRT may treat deficiency.
- Balanced diet, strength exercise, stress control, and quality sleep help maintain healthy hormone levels.
Normal Ranges: Testosterone Levels by Age and Life Stage
Testosterone levels in women are much lower than in men but remain important throughout life. Levels can change due to age, menopause, medical conditions, or medications. Knowing what is normal for your age helps spot problems early.
| Age Group | Total Testosterone (ng/dL) |
| 20-29 | 15–70 |
| 30-39 | 13–65 |
| 40-49 | 10–60 |
| 50+ (postmenopausal) | 7–45 |
Functions of Testosterone in Women
Testosterone influences many systems in the body. Here are the main roles it plays in women, with explanations:
- Muscle Strength and Mass : Testosterone supports building and maintaining muscle. This helps women stay strong, mobile, and independent as they age. Loss of muscle can lead to weakness and a higher risk of falls.
- Bone Density : Testosterone works with other hormones to protect bone strength. Low levels increase the risk of osteoporosis and fractures, especially after menopause.
- Sexual Desire and Satisfaction : This hormone helps maintain libido and arousal in women. Low testosterone can cause a drop in sexual interest, less satisfaction, or discomfort during intimacy.
- Mood and Cognitive Function : Testosterone contributes to stable mood, confidence, and mental sharpness. Low levels may be linked to depression, anxiety, or trouble concentrating.
- Red Blood Cell Production : Testosterone helps produce healthy red blood cells. Low levels can contribute to anemia and low energy.
- Fat Distribution : It helps control where the body stores fat. Changes in testosterone may cause more fat around the waist or hips.
Low Testosterone: Causes, Risks, and Symptoms in female
Women’s testosterone levels drop naturally with age, but other factors can lower them too. Common causes include ovary removal, certain medications, chronic illness, or problems with the adrenal glands or pituitary. Risks of low testosterone include weak bones, loss of muscle, mood changes, and low sexual drive. The following symptoms may appear:
- Persistent Fatigue and Loss of Motivation: Low testosterone can reduce energy levels, making you feel constantly tired even after adequate rest. This often comes with a lack of motivation to engage in daily tasks, exercise, or hobbies.
- Declining Muscle Mass and Strength: Testosterone plays a key role in building and maintaining muscle. Lower levels can lead to noticeable loss of muscle mass and a decline in strength, making physical activities feel more challenging.
- Thinning Hair and Dry Skin: Testosterone supports hair growth and skin health. Reduced levels may cause hair to thin on the scalp and body, while skin can become dry, less elastic, and more prone to irritation.
- Low Interest in Sex or Difficulty with Arousal: Testosterone directly influences libido. Men and women with low levels may notice reduced sexual desire or difficulty achieving arousal or maintaining erections.
- Mood Swings, Depression, or Irritability: Hormonal imbalance affects brain chemistry, which can lead to emotional changes such as irritability, anxiety, or depressive episodes. Small stressors may feel overwhelming, and mood may fluctuate frequently.
- Poor Focus or Memory: Testosterone supports cognitive function. Low levels can lead to trouble concentrating, slower mental processing, forgetfulness, and difficulty retaining new information.
High Testosterone: Causes, PCOS, Adrenal Disorders, Symptoms
High testosterone in women is less common but can cause significant health problems. The main causes include:
- Polycystic Ovary Syndrome (PCOS)
PCOS is the most common reason for high testosterone in women. It affects hormone balance, ovulation, and often causes irregular periods, excess hair growth, acne, and infertility. - Adrenal Disorders
Tumors or disorders of the adrenal glands can increase testosterone production. This may cause rapid changes in hair growth, deepening voice, or clitoral enlargement. - Congenital Adrenal Hyperplasia
This genetic condition can lead to lifelong high androgen levels.
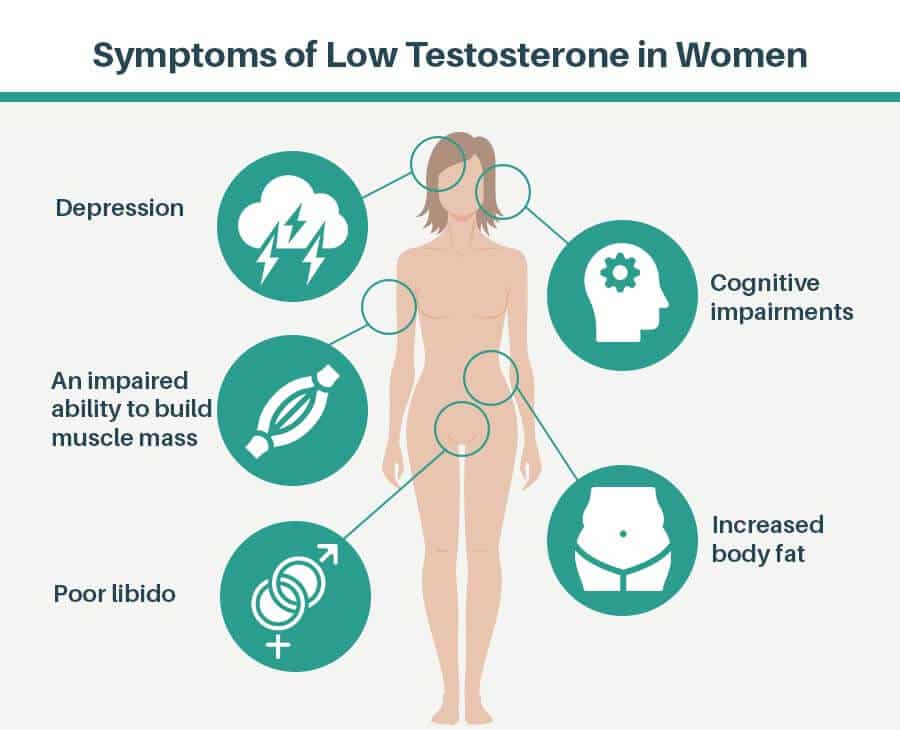
Symptoms of high testosterone in female
High testosterone in women causes excess body hair, acne, voice deepening, irregular periods, and fertility issues. These symptoms often signal hormonal imbalance needing medical attention.
| Symptom | What to Look For |
|---|---|
| Unwanted Facial or Body Hair | Excessive hair growth on face, chest, back, or other areas |
| Thinning Scalp Hair / Baldness | Male-pattern baldness or noticeable hair thinning on the scalp |
| Oily Skin or Severe Acne | Increased oiliness and frequent or severe acne breakouts |
| Irregular or Missed Periods | Changes in menstrual cycle, skipped or unpredictable periods |
| Deepening of the Voice | Voice becomes lower or more masculine in tone |
| Enlargement of the Clitoris | Noticeable growth of clitoris in females |
| Fertility Problems | Difficulty conceiving due to hormonal imbalance |
How Hormonal Imbalance Affects Menstrual, Sexual, and Bone Health
A hormonal imbalance, especially involving testosterone, can have wide-reaching effects on women’s health. High testosterone or disorders like PCOS may cause irregular or missed menstrual cycles. Low testosterone can lead to reduced sexual desire, discomfort during intimacy, and decreased satisfaction. Bone health is also at risk, as low testosterone especially when combined with low estrogen after menopause can weaken bones and raise the chance of fractures. These changes may develop gradually but can greatly impact daily life and long-term well-being. Clinical studies show that restoring hormonal balance can help normalize menstrual cycles, improve sexual health, and increase bone strength, contributing to a better quality of life for women facing these hormone-related issues.
Diagnosis: Blood Tests, Medical Evaluation, Ruling Out Other Issues
Diagnosis begins with a conversation about symptoms and a detailed health history. Your doctor will ask about your energy, mood, menstrual cycles, sexual health, weight changes, and any family history of hormone disorders to get a clear overview of your situation.
- Blood Tests
A morning blood sample is taken to measure total and sometimes free testosterone. Doctors often check additional hormones, including DHEA, LH, FSH, and estradiol, to see how your whole hormone system is working and identify the cause of symptoms. - Other Lab Work
Testing thyroid function, fasting blood glucose, and insulin levels helps find related issues, such as thyroid disease or insulin resistance, which can mimic or worsen hormone imbalance symptoms and affect overall hormone health. - Imaging
An ultrasound of the ovaries or imaging of the adrenal glands may be ordered if your doctor suspects tumors, cysts, or structural problems that could be raising or lowering testosterone or other hormone levels.
Lifestyle Strategies: Diet, Exercise, Stress, Sleep
Healthy lifestyle choices support hormone balance and can relieve many mild symptoms. Here are proven strategies:
- Balanced Diet
Include protein, healthy fats, and a variety of fruits and vegetables. Avoid extreme diets or high sugar intake. - Regular Exercise
Aim for both aerobic activity and strength training. Exercise helps regulate hormones, supports healthy weight, and improves mood. - Stress Management
Chronic stress can disturb hormone production. Activities like yoga, meditation, and deep breathing help reduce stress. - Sleep Hygiene
Get seven to eight hours of quality sleep each night. Poor sleep can disrupt hormone signals.
Medical Treatments: When and What to Consider
Medical treatment is sometimes needed if symptoms are severe or lifestyle changes do not work. Options depend on the underlying cause.
- For Low Testosterone
Testosterone therapy is not FDA-approved for women except in specific cases, such as severe sexual dysfunction that does not respond to other treatments, particularly after menopause. In these cases, some hormone specialists may prescribe a very low dose of testosterone, carefully monitoring for side effects or complications. The risks and benefits must be discussed in detail with a doctor, as long-term safety in women is not fully established. - For High Testosterone
In most cases, such as with Polycystic Ovary Syndrome (PCOS), doctors may recommend birth control pills to help regulate periods and lower androgen levels. Anti-androgen medications like spironolactone can reduce unwanted hair growth and acne by blocking the effects of excess testosterone. If insulin resistance or diabetes is also present, medications such as metformin may be added. For cases caused by adrenal or ovarian tumors, surgery or more targeted therapy may be needed to correct hormone levels. All medical treatments require close monitoring by a healthcare provider to ensure safety and effectiveness.
Prevention and Long-Term Well-Being
Regular medical checkups and maintaining a healthy lifestyle are key to preventing hormone problems before they become serious. Women should avoid starting hormone supplements or using testosterone boosters from stores or online without first talking to a healthcare provider. Staying active, eating a balanced diet, managing stress, and getting enough sleep all support hormone balance. Paying attention to new symptoms and seeking help early can prevent bigger issues later, especially those affecting bone and heart health. Early action often leads to better health outcomes and an improved quality of life.
Conclusion
Testosterone is a vital hormone for women, supporting muscle strength, emotional well-being, sexual health, and strong bones. Both low and high levels of testosterone can lead to problems such as fatigue, mood swings, low libido, bone loss, or unwanted hair growth. However, most hormone imbalances are manageable with awareness and proper care. Recognizing symptoms early and seeking medical advice allows for accurate diagnosis and the right treatment plan. Healthy lifestyle choices such as balanced nutrition, regular exercise, good sleep, and stress management play a key role in keeping hormone levels steady. When needed, expert medical support can address underlying conditions or provide targeted therapies. By staying attentive to changes and making informed decisions, women can maintain hormonal balance, protect their long-term health, and stay active and independent at every stage of life.
FAQs
1. What causes high testosterone in women?
Common causes are PCOS, adrenal gland disorders, certain tumors, and genetic conditions like congenital adrenal hyperplasia. Overuse of supplements or medications can also contribute. A thorough evaluation is needed to find the exact cause.
2. How does low testosterone affect women’s health?
It can cause fatigue, low mood, muscle weakness, bone loss, low sexual interest, and poor concentration. Over time, low testosterone may raise the risk of osteoporosis and affect overall quality of life.
3. Can testosterone imbalance cause weight changes?
Yes, both low and high testosterone can change the way the body stores fat. High testosterone may increase abdominal fat, while low testosterone is linked to muscle loss and weight gain.
4. What are the signs of hormonal imbalance in women?
Signs include irregular periods, unwanted hair growth, thinning scalp hair, acne, mood changes, low libido, and changes in weight or energy. Lab tests help confirm the diagnosis.
5. Are there natural ways to balance testosterone?
Yes, a healthy diet, regular exercise, stress management, and good sleep habits support hormone balance. Severe imbalances may need medical care, but lifestyle is always the foundation.
6. Is testosterone therapy safe for women?
Testosterone therapy is not FDA-approved for women except in rare cases. It can have risks and should only be used under specialist supervision for severe symptoms after other treatments fail.
7. Does birth control affect testosterone?
Yes, birth control pills often lower testosterone levels and reduce symptoms of high testosterone. They are commonly used to treat PCOS and related problems.
8. Can diet and exercise alone restore balance?
For mild imbalances, diet and exercise can be enough. More severe or persistent cases often need medical evaluation and treatment in addition to healthy habits.
9. How often should women check hormone levels?
Routine hormone testing is not needed unless symptoms appear. Women with hormone-related health problems should follow their doctor’s recommendations for follow-up.
10. Does menopause always lower testosterone?
Testosterone usually drops after menopause, but levels vary by person. Some women maintain moderate levels, while others experience a sharper decline.
References
- Cleveland Clinic: Low Testosterone in Women Mayo Clinic
- Mayo Clinic: Polycystic Ovary Syndrome (PCOS) Mayo Clinic+4Mayo Clinic+4Mayo Clinic+4
- Wikipedia: Testosterone CCJM+4Cleveland Clinic+4Cleveland Clinic+4
- PMC: Testosterone in Women Cleveland ClinicCleveland Clinic
- Medical News Today: Normal Testosterone Levels in Women
- ScienceDirect: Testosterone WikipediaCCJM
- Harvard Health: Women and Testosterone Cleveland ClinicCCJM
- Verywell Health: Diagnosing Hormonal Imbalance in Women Cleveland Clinic
- WebMD: Testosterone in Women Cleveland Clinic+5Cleveland Clinic+5Cleveland Clinic+5
- Endocrine Society: Clinical Guidelines on Testosterone in Women
Dr. Ethan Ward, MD, is a board-certified urologist with over 12 years of clinical experience specializing in men’s health, hormone optimization, and sexual wellness. He earned his MD from Johns Hopkins University School of Medicine and completed his urology residency at Cleveland Clinic. Dr. Ward focuses on testosterone therapy, erectile function, and metabolic contributors to hormonal imbalance. His work includes peer-reviewed research on andropause management and patient-centered approaches to male vitality.