
Hormones regulate vital skin functions like oil control, hydration, elasticity, and pigmentation. Estrogen, progesterone, and androgens influence collagen, sebum, and firmness, while hormonal shifts during puberty, pregnancy, or menopause trigger issues like acne, melasma, dryness, and aging. Balanced hormones are key to healthy, glowing skin.
Key Takeaways
- Estrogen boosts collagen, elasticity, and hydration; its decline causes dryness and wrinkles.
- Progesterone supports firmness; androgens increase oil, leading to acne and breakouts.
- Growth hormone and IGF-1 aid repair but excess triggers acne.
- Melatonin and MSH protect from oxidative stress and regulate pigmentation.
- Hormonal changes in menstrual cycle, pregnancy, and menopause alter skin condition.
- Treatments include HRT, antiandrogens, and topical hormones under medical guidance.
- Balanced diet, quality sleep, stress control, and non-disruptive skincare maintain hormonal skin balance.
Skin as an Endocrine Organ
The skin is not only a protective barrier, it also functions like a small hormone factory. It can produce, store, and respond to hormones. This means the skin does not just react to internal hormonal changes but also has its own regulatory system. Receptors in skin cells allow hormones to trigger specific changes like oil production, elasticity, and pigmentation which is why skin care myths often oversimplify this complexity
Key Hormones and How Hormones Affect skin Health
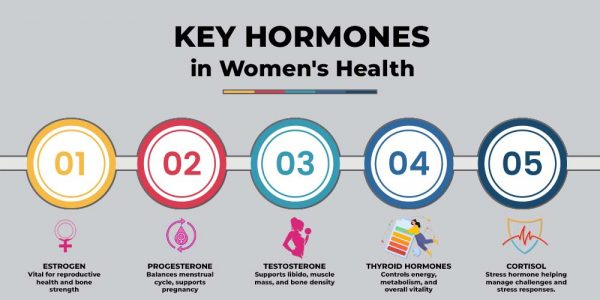
Hormones act differently depending on life stage and health condition. Some promote youthful glow while others contribute to breakouts or sagging. Below are the most important hormones for skin health.
Estrogen
Estrogen is often called the skin’s natural moisturizer. It increases collagen, elastin, and hyaluronic acid, all of which keep the skin plump and firm. It also supports good blood flow and helps wounds heal faster. During menopause, when estrogen levels drop, women often notice wrinkles, dryness, and thinning skin (read more about menopause skin changes). Hormone replacement therapy can sometimes restore these qualities but must be used under medical guidance.
Progesterone
Progesterone supports skin elasticity and firmness. Research shows that topical progesterone creams may improve hydration and reduce fine lines. Unlike estrogen, its main effect is not on thickness but on keeping skin tight and smooth. Low levels of progesterone can contribute to dull or sagging skin, which is why choosing the right natural or synthetic skincare products also matters.
Androgens
Androgens like testosterone and DHT stimulate oil glands. This is why teenagers often get acne when androgen levels spike during puberty. Excessive androgen activity can lead to oily skin, clogged pores, and deep acne. In women, conditions like PCOS often come with androgen-driven breakouts and unwanted facial hair a common cause of teen skin care struggles.
Growth Hormone and IGF-1
Growth hormone and IGF-1 promote skin regeneration and thickness. They support wound healing and overall renewal. However, excess IGF-1 is linked to acne, especially when combined with diets high in dairy or sugar one of the skincare mistakes people overlook.
Melatonin
Melatonin is best known as the sleep hormone, but it also protects the skin from free radicals. It helps prevent early wrinkles and supports the skin’s natural repair cycle overnight, making restful sleep critical for skin health.
Melanocyte-Stimulating Hormone
This hormone regulates melanin, the pigment that gives skin its color. During pregnancy, higher levels can lead to melasma — dark patches on the face. Using the right sunscreen is key for protecting against worsening pigmentation.
Clinical and Therapeutic Insights
Doctors often use hormone-based therapies to improve skin health. These treatments must be carefully matched to the person’s condition and hormone levels.
- Hormone replacement therapy (HRT): Restores estrogen and progesterone in menopausal women to reduce wrinkles and dryness.
- Antiandrogens: Drugs like spironolactone or certain birth control pills lower androgen activity and control acne in women.
- Topical hormones: Creams with estrogen or progesterone are being studied for firming and anti-aging effects.
- Xeno-hormones caution: Some skincare and household products contain hormone-mimicking chemicals that may disrupt natural balance and worsen skin issues.
Here is a clear comparison of major hormone-based approaches for skin and overall health, with their main benefits, risks or concerns, and who they are best suited for:
| Therapy Type | Main Benefits | Risks or Concerns | Best Suited For |
| Hormone Replacement Therapy (HRT) | Restores estrogen & progesterone, improves hydration, reduces wrinkles, slows collagen loss | May increase risk of blood clots, breast cancer, or heart disease if not carefully managed | Women in menopause with significant dryness, thinning, and wrinkles |
| Antiandrogens | Controls oil production, reduces hormonal acne, prevents jawline breakouts | Side effects may include irregular periods, dizziness, or potassium imbalance | Women with persistent hormonal acne, especially related to PCOS |
| Topical Hormones | Improves elasticity, hydration, and firmness in early studies | Long-term safety not fully established, available only in limited settings | Women seeking non-invasive anti-aging options under medical care |
| Avoiding Xeno-Hormones | Prevents disruption of natural hormone balance, reduces risk of skin flare-ups | Requires label reading and product awareness | Anyone wanting safer skincare and lifestyle choices |
How Menstrual Cycle, Pregnancy, and Menopause Affect Your Skin
Hormone levels rise and fall throughout life, which explains why the skin looks different at each stage.
Menstrual Cycle
In the first half of the cycle, rising estrogen levels improve skin hydration, elasticity, and clarity, often resulting in a glowing complexion. However, in the second half, just before menstruation, progesterone and androgens increase, causing the skin to produce more oil and leading to breakouts and pimples commonly experienced before periods.
- Estrogen boosts collagen production, enhancing skin firmness and reducing wrinkles.
- Higher estrogen levels increase skin’s ability to retain moisture, making it feel plumper and softer.
- Progesterone stimulates oil glands, increasing sebum production, which can clog pores.
- Androgens further aggravate oiliness and inflammation, triggering acne flare-ups.
- Premenstrual hormonal shifts may also increase skin sensitivity and redness in some individuals.
Pregnancy
During pregnancy, estrogen and progesterone levels surge to high levels. This can create a radiant, plump “pregnancy glow” for some women. However, others may experience skin challenges like melasma (dark patches), worsening acne, or eczema flare-ups. These changes are usually temporary, resolving after childbirth but can be distressing during pregnancy.
- Elevated estrogen and progesterone enhance blood flow, leading to a brighter, healthier-looking complexion.
- Increased hormone levels stimulate oil glands, which may trigger acne flare-ups in some women.
- Melasma (“mask of pregnancy”) appears as brown patches, especially on the cheeks, nose, and forehead, due to heightened pigmentation.
- Eczema may worsen or improve depending on individual hormonal responses.
- Changes in skin may also include increased sensitivity, spider veins, or stretch marks.
- Most pregnancy-related skin changes resolve after delivery, but sun protection and gentle skincare are important during this period.
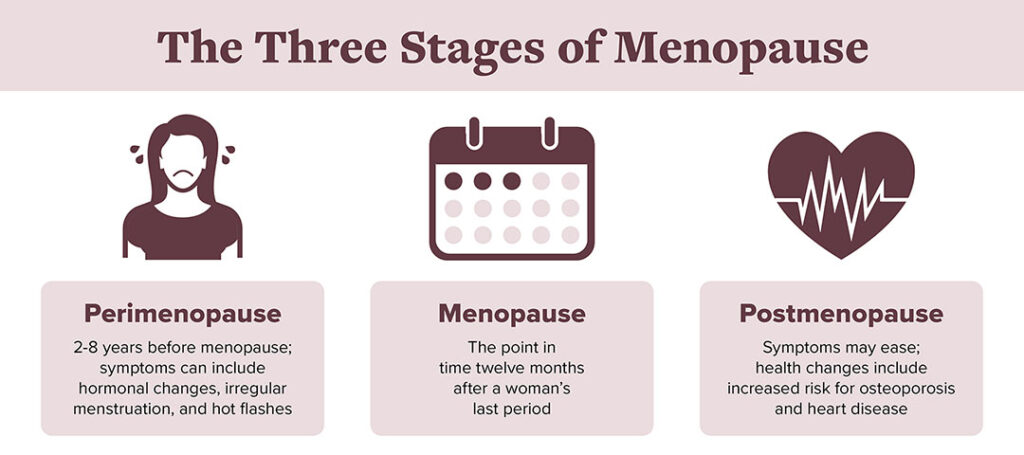
Menopause
When estrogen levels fall, collagen drops sharply. Skin becomes thinner, drier, and more prone to sagging. Fine lines and wrinkles appear faster. Hormone therapy or supportive skincare with hydrating and collagen-boosting ingredients may help.
- Reduced estrogen leads to a significant decline in collagen and elastin, diminishing skin firmness and elasticity.
- Skin loses moisture more easily, increasing dryness, flakiness, and potential for irritation.
- Thinner skin is more susceptible to bruising, slower wound healing, and increased sensitivity.
- Prominent fine lines and deeper wrinkles may develop more rapidly after menopause.
- Sagging around the jawline, cheeks, and neck becomes more common.
- Supportive measures may include hormone replacement therapy (HRT), intensive moisturizers, retinoids, peptides, and products that boost collagen production.
Hormone-Sensitive Skin Disorders
Hormones have profound effects on the skin, influencing not only its appearance but also the severity and timing of many chronic conditions. Here’s a detailed explanation of how hormones interact with specific skin disorders and why understanding this link can improve management and treatment.
Hormonal Acne
Hormonal acne is characterized by breakouts that predominantly appear on the lower face, jawline, and chin.
- Why it happens: Androgens (male hormones present in all genders, including testosterone) stimulate sebaceous (oil) glands, increasing oil production and clogging pores.
- Typical patterns: It often flares up a few days before menstruation when estrogen and progesterone levels drop and the androgen effect rises. It’s common in puberty, PCOS, pregnancy, and menopause.
- Treatment focus: Addressing the hormonal imbalance is key—oral contraceptives, antiandrogens (like spironolactone), and lifestyle adjustments (stress reduction, diet) may help manage symptoms.
Eczema (Atopic Dermatitis)
Eczema is an inflammatory skin condition causing itchy, red, and scaly patches.
- Why it happens: Estrogen and progesterone have anti-inflammatory and skin-protective roles. Their drop before menstruation or during menopause can worsen skin barrier function, leading to eczema flares. Pregnancy brings hormonal fluctuations that can either worsen or temporarily improve eczema.
- Management: Strategies may include intensified moisturizing, anti-inflammatory creams, and anticipating and treating premenstrual flares more proactively.
Hidradenitis Suppurativa (HS)
HS causes painful lumps, boils, and abscesses in areas with skin folds, such as armpits, groin, and under breasts.
- Why it happens: Androgen hormones promote increased sweat, oil gland activity, and hair follicle changes, fueling the inflammation seen in HS.
- Patterns: Flares may worsen around menstruation, puberty, or conditions associated with high androgens (such as PCOS).
- Treatment: Antiandrogen medications, weight loss, and sometimes hormonal regulation through medications can reduce severity.
Psoriasis and Atopic Dermatitis
These chronic inflammatory conditions present as red, scaly, or itchy plaques and patches.
- Why it happens: Estrogen and progesterone promote anti-inflammatory activity. Their decline (such as before periods or at menopause) can worsen these skin conditions. Flare-ups are also common during hormonal shifts in pregnancy or puberty.
- Management: Doctors may recommend closer monitoring and tailored therapies around hormonal transitions, such as changes in birth control or menopause.
Supporting Skin Through Lifestyle
While medical therapies target hormones directly, lifestyle also makes a big difference in maintaining healthy skin and mitigating hormone-related issues.
- Balanced diet: Limiting high-sugar foods and dairy may help lower insulin-like growth factor 1 (IGF-1) spikes, reducing the risk of acne breakouts. Consuming antioxidant-rich fruits, vegetables, and omega-3 fatty acids can support overall hormone balance and provide nutrients vital for skin repair.
- Quality sleep: Regular, restorative sleep boosts melatonin and growth hormone production, both of which are crucial for skin cell regeneration, healing, and maintaining a healthy glow.
- Stress management: Chronic stress elevates cortisol levels, which weakens the skin’s protective barrier and promotes inflammation. Techniques such as relaxation, regular exercise, and mindfulness practices can help lower cortisol and support resilient skin.
- Skincare choices: Opt for gentle, scientifically backed skincare ingredients including retinoids (to stimulate collagen and cell renewal), hyaluronic acid (for hydration), and peptides (to support repair). Avoid cosmetics and personal care products containing endocrine-disrupting chemicals, which can interfere with hormone function and affect skin health.
Future Research and Innovations
The field of dermatology is rapidly evolving, with new studies exploring hormones and biologically active compounds beyond just estrogen and androgens. These emerging therapies could significantly advance skin repair and anti-aging strategies.
- Melatonin creams: Investigated for their antioxidant properties, melatonin-based topical products may protect skin from oxidative stress, promote overnight repair, and reduce visible signs of aging.
- Oxytocin sprays: Known as the “bonding hormone,” oxytocin is being explored in topical formulations for its potential to enhance skin barrier function, elasticity, and wound healing.
- Endocannabinoid-based products: Leveraging molecules related to the body’s own cannabinoid system, these new formulations aim to soothe inflammation, balance sebum production, and support skin homeostasis.
- Integration with traditional skincare: As research expands, the future of dermatology may combine conventional ingredients (like retinoids, vitamin C, and peptides) with innovative hormone- and bioactive-targeted therapies for personalized, highly effective solutions.
Conclusion
Hormones deeply influence skin health across all life stages. The skin acts as both a barrier and a hormone-responsive organ, with estrogen, progesterone, and androgens shaping hydration, elasticity, and oil production. Fluctuations during periods, pregnancy, and menopause result in breakouts, dryness, or glow. Growth hormone, melatonin, and melanocyte-stimulating hormone also affect repair and pigmentation.
Common issues like hormonal acne, eczema, and melasma arise from hormone changes. Treatments include HRT, antiandrogens, and topical hormones, but lifestyle diet, sleep, stress, and thoughtful skincare remain crucial in maintaining balanced, healthy, and radiant skin.
FAQs
1. How does estrogen keep skin youthful?
It increases collagen, hydration, and elasticity, making the skin plump and firm.
2. Why does acne flare before periods?
Androgen and progesterone levels rise, causing more oil production and clogged pores.
3. Is hormonal acne different from teenage acne?
Yes, hormonal acne usually affects the lower face and jawline, while teenage acne appears on the forehead and cheeks.
4. Can progesterone improve aging skin?
Topical progesterone may improve firmness, though research is still limited.
5. What role does melatonin play in skin repair?
It works as a strong antioxidant and boosts the skin’s nighttime healing cycle.
6. How does menopause change skin?
Lower estrogen causes thinner, drier, and more wrinkled skin.
7. What treatments work for hormonal acne?
Antiandrogen drugs, certain birth control pills, and topical retinoids are commonly used.
8. Can hormones worsen eczema?
Yes, many women experience flare-ups before menstruation or during pregnancy.
9. Are hormone creams safe for skin?
They may help but should only be used with medical supervision to avoid side effects.
10. How can lifestyle help balance skin hormones?
Good sleep, stress management, and a balanced diet support healthy hormone levels and better skin.
Reference
- The skin acts as a hormone-responsive organ, producing and reacting to hormones.
https://bendderm.com/hormones-and-how-they-affect-your-skin/ - Estrogen boosts collagen and hydration, promoting plump and firm skin.
https://bendderm.com/hormones-and-how-they-affect-your-skin/ - Menopause-related estrogen decline leads to dryness, thinning, and wrinkles.
https://bendderm.com/hormones-and-how-they-affect-your-skin/ - Androgens like testosterone stimulate oil glands, causing acne and oiliness.
https://bendderm.com/hormones-and-how-they-affect-your-skin/ - Hormonal fluctuations during menstrual cycles and pregnancy cause breakouts and pigment changes.
https://bendderm.com/hormones-and-how-they-affect-your-skin/ - Growth hormone and IGF-1 help skin regeneration; excess may trigger acne.
https://bendderm.com/hormones-and-how-they-affect-your-skin/ - Melatonin protects skin from free radicals and supports overnight repair.
https://bendderm.com/hormones-and-how-they-affect-your-skin/ - Hormone changes can worsen conditions like eczema, melasma, and rosacea.
https://bendderm.com/hormones-and-how-they-affect-your-skin/ - Balanced diet, sleep, and stress management support hormonal skin health.
https://bendderm.com/hormones-and-how-they-affect-your-skin/ - Future skin therapies may include hormone-targeted creams and advanced actives.
https://bendderm.com/hormones-and-how-they-affect-your-skin/
Chance Jones is a clinical biochemist with a PhD in Clinical Biochemistry from the University of Toronto (2014) and 11 years in assay development and reference-range validation. Their expertise spans nutrient biomarkers (e.g., 25(OH)D, B12, ferritin) and lab quality standards (CLIA/CAP). Chance audits evidence behind test-guided supplementation and explains lab variability for readers. Profiles: ORCID, ResearchGate; selected publications and method validations.

