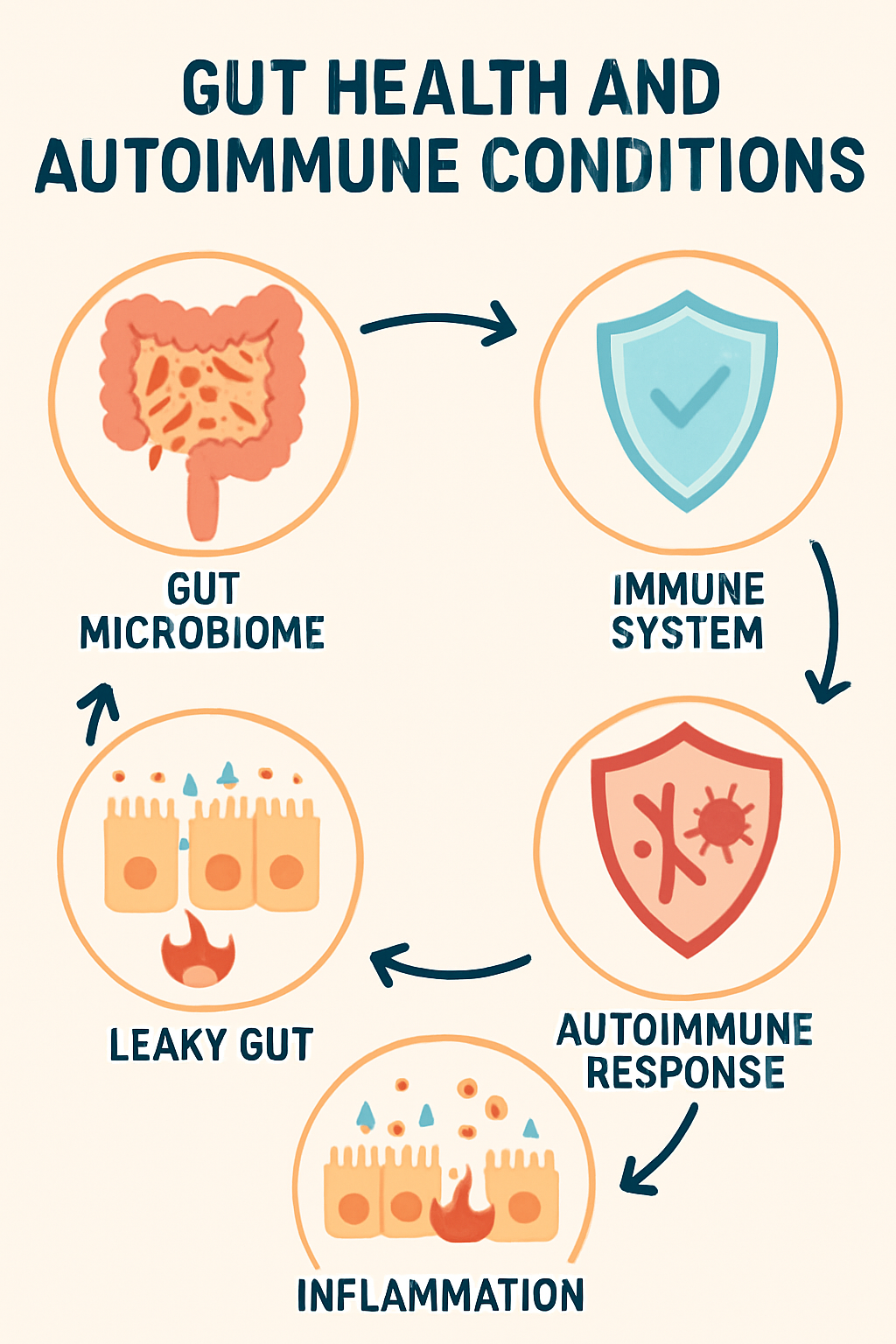
Gut health plays a central role in immune regulation. Imbalance in the gut microbiome or a damaged intestinal barrier can trigger inflammation and abnormal immune responses, contributing to the development or worsening of autoimmune diseases.
Key Takeaways
- Over 70% of immune cells reside in the gut, linking microbiome balance directly to immune health.
- Dysbiosis and leaky gut promote chronic inflammation and autoimmune activation.
- Autoimmune diseases like IBD, lupus, and rheumatoid arthritis show strong gut-microbiome connections.
- Diet diversity, probiotics, and anti-inflammatory foods help restore gut integrity and immune tolerance.
- Chronic stress, poor sleep, and medication misuse disrupt gut balance and increase autoimmune risk.
- Managing gut health through nutrition, lifestyle, and mindful medical use reduces inflammation and supports long-term immune stability.
What Is Gut Health?
Gut health refers to the proper function and balance of your digestive system, particularly the gut microbiome, a complex community of trillions of microorganisms living in your intestines. These microbes help break down food, absorb nutrients, produce essential vitamins, support immune function, and regulate inflammation.
A healthy gut features a diverse population of beneficial bacteria and a strong intestinal lining that acts as a barrier, preventing harmful substances from entering the bloodstream. When gut health is compromised due to a poor diet, stress, lack of sleep, or medications like antibiotics it can lead to digestive issues, weakened immunity, chronic inflammation, and even contribute to autoimmune diseases. Maintaining good gut health through a balanced, fiber-rich diet and healthy lifestyle is essential for digestion, immune defense, and overall well-being.
Why Is It Important to Have Great Gut Health?
Great gut health is essential because the gastrointestinal system is deeply involved in nearly every aspect of your physical and mental well-being. Here’s why maintaining optimal gut health matters:
1. Immune System Support
Supporting your immune system involves a combination of healthy lifestyle habits, proper nutrition, and sometimes targeted supplements. Here’s a comprehensive overview of ways to support your immune system.
- Approximately 70% of your immune cells are located in the gut.
- A diverse and balanced gut microbiome helps your immune system distinguish between harmful invaders and safe substances, reducing your risk of infections and chronic inflammation.
2. Digestive Efficiency and Nutrient Absorption
Supporting digestive efficiency and nutrient absorption is key to getting the most from your food and maintaining overall health including immune health. Here’s how you can improve both.
- Healthy gut bacteria break down food and help absorb essential vitamins and minerals like vitamin B12, vitamin K, magnesium, and short-chain fatty acids.
- Good gut health prevents problems like bloating, constipation, diarrhea, and indigestion.
3. Inflammation Control
Controlling inflammation is essential for long-term health, especially to prevent chronic diseases and support immunity. Here’s a breakdown of effective strategies.
- Balanced gut bacteria help maintain low levels of inflammation in the body, lowering the risk of chronic diseases such as diabetes, obesity, cancer, and heart disease.
- Imbalances, known as gut dysbiosis, are linked to higher inflammatory markers associated with autoimmune disease .
4. Mental Health and Mood
Supporting mental health and mood involves nurturing the brain, managing stress, and creating emotional balance. Here’s a comprehensive approach.
- The gut brain axis allows gut bacteria to influence brain chemistry and mood by producing neurotransmitters like serotonin and gamma-aminobutyric acid (GABA).
- Poor gut health is associated with increased risk of anxiety, depression, and cognitive decline.
5. Barrier Protection
Barrier protection refers to the body’s first line of defense against pathogens mainly the skin, mucous membranes, and gut lining. Strengthening these barriers is crucial for immune resilience and overall health.
- The gut lining acts as a physical and chemical barrier, controlling what enters the bloodstream.
- If the barrier is compromised (sometimes called “leaky gut”), larger, unwanted particles can escape, prompting immune reactions and potentially contributing to allergies or autoimmunity.
6. Weight Management and Metabolic Health
Supporting weight management and metabolic health is foundational to overall well-being and plays a direct role in immune function, energy levels, and disease prevention. Here’s a practical and science-backed approach.
- An optimal gut microbiome aids in proper metabolism and appetite regulation.
- Certain bacteria can affect how your body stores fat and balances blood sugar, influencing your risk for obesity and metabolic syndrome.
Dos and Don’ts for a Healthy Gut
A balanced gut promotes better digestion, immunity, and overall well-being, especially as we age. Use the table below for practical tips on what to do and what to avoid for healthy gut function.
| Dos for Gut Health | Don’ts for Gut Health |
| Eat high-fiber foods (whole grains, fruits, veg) | Rely on processed snacks and sugary foods |
| Include fermented foods (yogurt, kimchi, kefir) | Overuse antibiotics unnecessarily |
| Stay hydrated by drinking water consistently | Skip hydration or drink too many sugary sodas |
| Choose anti-inflammatory foods (berries, fish, nuts) | Eat lots of red meats and fried foods |
| Diversify your diet with various plant foods | Stick to the same restricted food routine |
| Exercise regularly—brisk walks, swimming, or cycling | Lead a consistently sedentary lifestyle |
| Manage stress with breathing or gentle activities | Ignore long-term stress and poor coping habits |
| Get 7–8 hours of quality sleep each night | Sacrifice rest and have irregular sleep patterns |
| Focus on prebiotics (bananas, garlic, onions) | Avoid fresh produce and fiber-rich foods |
| Seek medical advice for ongoing gut symptoms | Self-diagnose persistent digestive complaints |
What Does Your Gut Health Affect?
Your gut health affects nearly every system in your body. The gut microbiome a complex community of trillions of microorganisms has wide-reaching influence, including:
- Immune function: Over 70% of the immune system is located in the gut.
- Digestion: Gut microbes help break down food and synthesize nutrients.
- Mood and brain health: The gut-brain axis links gut health to anxiety, depression, and cognition.
- Weight and metabolism: The balance of bacteria can influence fat storage and hunger hormones.
- Hormonal balance: Gut bacteria help regulate estrogen, cortisol, thyroid hormones, and more.
- Skin health: diseases like eczema, acne, and psoriasis are often tied to gut inflammation.
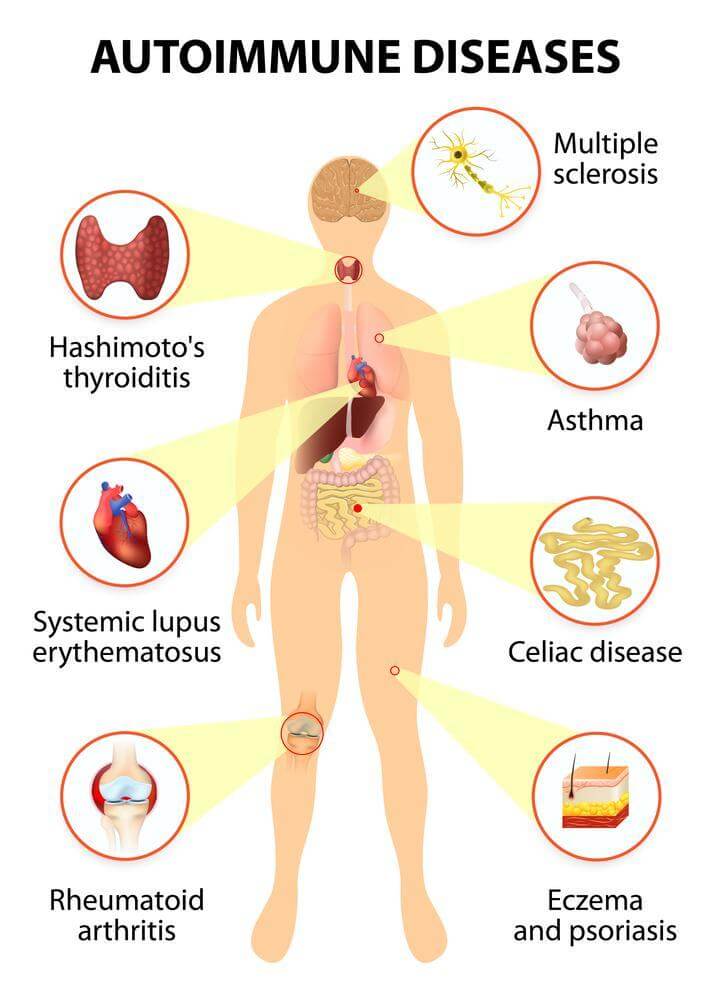
- Autoimmunity: Poor gut health is a major contributor to autoimmune disorders such as Hashimoto’s, rheumatoid arthritis, and lupus.
The Gut’s Role in Autoimmune Disorders

Autoimmune disorders occur when the immune system mistakenly attacks the body’s own tissues. The gut-immune connection is central to the development and progression of these diseases:
- Dysbiosis: An imbalance of gut microbes (loss of beneficial bacteria, overgrowth of harmful microbes) can alter immune responses, increasing inflammation and risk of autoimmunity.
- Molecular Mimicry: Some gut bacteria have structures similar to human cells, confusing the immune system and potentially leading to an attack on healthy tissues.
- Increased Permeability: When the gut barrier is compromised, larger molecules and microbes may cross into the bloodstream, triggering an abnormal immune response.
- Chronic Inflammation: Persistent gut imbalances keep the immune system activated, which can damage tissues and promote autoimmune processes.
Examples of Autoimmune disease Linked to Gut Health
- Inflammatory bowel diseases (IBD): Includes Crohn’s disease and ulcerative colitis, both marked by an abnormal immune response to gut microbes.
- Type 1 diabetes: Gut microbiome shifts are observed before disease onset, suggesting a role in immune dysfunction.
- Rheumatoid arthritis, lupus, and multiple sclerosis: Research identifies specific gut microbial changes and increased gut permeability in many patients.
Ways to Improve your Gut Health

Supporting your gut health is a powerful way to moderate immune system activity and lower the risk of autoimmune flare-ups. Here’s a comprehensive guide to fostering a balanced, resilient gut microbiome and strengthening your body’s defenses,
1. Eat a Diverse, Whole-Food Diet
Microbial diversity is a hallmark of a healthy gut. Improved diversity helps maintain balance, suppress harmful bacteria, and support overall health.
- Aim for variety: Strive to eat 30+ different plant-based foods weekly, including vegetables, fruits, legumes, nuts, seeds, and herbs.
- Prebiotic-rich foods: Garlic, onions, leeks, asparagus, and bananas fuel healthy gut bacteria.
- Polyphenols for the microbiome: Include berries, green tea, olive oil, and dark chocolate for their powerful antioxidant and gut-supporting properties.
- Resistant starches: Add cooked-and-cooled potatoes, green bananas, and lentils, which reach the colon undigested and feed good microbes.
2. Use Probiotics for Gut Health
Probiotics are live, beneficial microorganisms that help restore microbial balance and support gut integrity.
Key probiotic strains:
- Lactobacillus rhamnosus GG: Enhances gut lining and immune function
- Bifidobacterium longum: Reduces inflammation
- Lactobacillus plantarum: Strengthens the gut barrier
- Saccharomyces boulardii: Protects against harmful pathogens
- Bifidobacterium infantis: Reduces IBS symptoms and systemic inflammation
Sources of probiotics:
- Fermented foods: Yogurt, kefir, kimchi, sauerkraut, miso, kombucha
- High-quality supplements: Aim for 10+ billion CFUs, covering several strains.
3. Prioritize the Best Foods for Gut Health
Select foods proven to nourish beneficial bacteria and build a resilient gut:
- Leafy greens (spinach, kale)
- Fermented foods (see above)
- Berries (antioxidant-rich)
- Bone broth (contains amino acids like glutamine for repair)
- Fatty fish (salmon, sardines, rich in omega-3s)
- Turmeric and ginger (natural anti-inflammatories)
4. Avoid the Worst Foods for Gut Health
Certain foods undermine gut barrier function and foster harmful bacteria, particularly problematic for those with autoimmunity.
- Refined sugars, artificial sweeteners
- Processed foods and additives (emulsifiers, preservatives)
- Gluten and dairy (if sensitive)
- Fried or fast food
- Excess alcohol and caffeine
- Large amounts of red and processed meat
5. Manage Stress Levels
Chronic stress increases levels of the hormone cortisol, which can disrupt the balance of your gut microbiome and weaken the protective gut barrier. To support gut and immune health, integrate regular stress management practices:
- Meditation and deep breathing: Calms the nervous system and reduces stress hormones.
- Yoga, walking, and time in nature: Physical movement and exposure to natural environments reduce psychological stress and benefit gut diversity.
- Journaling and gratitude practices: Help process emotions and cultivate a positive mindset, further lowering stress’s physiological impact.
6. Prioritize Quality Sleep
Quality sleep is essential for gut microbial stability and effective immune function.
- Target 7–9 hours each night: Sleep enables repair and balancing of gut bacteria.
- Limit screen time before bed: Blue light can disrupt sleep hormones.
- Maintain a consistent schedule and environment: Stick to regular bedtimes and create a cool, dark, quiet space to support restful sleep.
7. Exercise Regularly
Moderate, consistent exercise encourages a more diverse and balanced gut microbiome and reduces inflammation.
- Aim for 30 minutes of activity daily: Walking, swimming, or cycling are excellent choices.
- Avoid overtraining: Excessive exercise can damage the gut barrier and impair immune response. Balance movement with adequate rest.
8. Use Antibiotics and Medications Wisely
While sometimes necessary, antibiotics can eliminate both beneficial and harmful gut bacteria.
- Take only as prescribed: Avoid unnecessary antibiotic use.
- Replenish good bacteria: After a course, consume probiotic-rich foods or supplements.
- NSAIDs caution: Medications like ibuprofen can irritate the gut lining—use sparingly and consult your healthcare provider for alternatives.
9. Consider Functional Testing
If you experience ongoing digestive or immune issues:
- Consult a functional medicine provider: Specialized practitioners can assess gut health more comprehensively.
- Investigate imbalances: Testing can reveal gut microbiome disruptions, increased intestinal permeability (“leaky gut”), food sensitivities, and nutrient deficiencies so you can receive personalized recommendations.
Conclusion
Optimizing gut health is key to immune balance and lowering the risk of autoimmune disease . A diverse, well-supported microbiome regulates immune responses, strengthens the gut barrier, and limits inflammation.A nutrient-dense, whole-food diet, targeted probiotics, stress management, quality sleep, consistent exercise, and careful medication use all contribute to a healthy gut environment. For ongoing symptoms, functional testing and expert guidance can offer deeper insight.
Beyond immune health, a strong gut supports digestion, energy, skin clarity, and emotional stability via the gut-brain axis. As research continues to uncover its central role in everything from metabolism to mental resilience, gut health stands out as a cornerstone of long-term well-being. Investing in your microbiome is one of the most impactful strategies for lifelong vitality and disease prevention.
Frequently Asked Questions
Can improving gut health reverse autoimmune diseases?
Improving gut health may reduce symptoms and inflammation but usually does not reverse autoimmune diseases. A balanced gut supports immune regulation and can enhance quality of life.
Is it safe to take probiotics with autoimmune disease ?
Probiotics are generally safe and beneficial, but those with severely compromised immune systems should consult a doctor before use.
How do antibiotics influence gut health and autoimmunity?
Antibiotics can disrupt gut bacteria, leading to dysbiosis and weakened barrier function. Probiotics or fermented foods are recommended after antibiotic use.
Can children’s gut health affect their risk for autoimmune diseases?
Early gut health is crucial for immune development. Microbiome disruptions in childhood are linked to higher autoimmune risk later in life.
Are food intolerances a sign of poor gut health or autoimmunity?
Food intolerances may result from gut damage or immune dysregulation. Frequent intolerances should prompt a gut health evaluation.
Do all autoimmune patients need to follow a strict elimination diet?
Not all require strict diets. Some benefit from removing triggers, while others improve with broader dietary diversity and gut-friendly habits.
Are gluten and dairy always harmful for gut health in autoimmune disease?
Some individuals benefit from avoiding gluten or dairy; others may tolerate moderate amounts. Consultation with a healthcare provider is advised.
Can stress alone trigger gut and immune problems?
Chronic stress can disrupt the gut microbiome, weaken the gut lining, and worsen autoimmune activity. Stress management is important.
Is there a link between gut health and skin or mental health?
Gut imbalances can contribute to skin disease and affect mood through the gut-brain axis. Improving gut health often helps these symptoms.
Should I avoid exercise when experiencing an autoimmune flare?
Gentle movement is generally safe and helpful. Intense exercise during flares can worsen symptoms. Follow medical advice and listen to your body.
Reference
- Gut Microbiota, Leaky Gut, and Autoimmune Diseases – PMC
- Autoimmunity and the Gut – PMC
- Emerging role of gut microbiota in autoimmune diseases – Frontiers in Immunology
- Exploring the role of gut microbiome in autoimmune diseases – ScienceDirect
- Autoimmune diseases exhibit shared alterations in the gut microbiome – Rheumatology
- Gut microbiota and autoimmune diseases: mechanisms, treatment, challenges, and future recommendations
- Exploring the role of gut microbiome in autoimmune diseases: A comprehensive review – PubMed
- The Relationship Between Autoimmune Disease and the Gut Microbiome – Autoimmune Institute
- Role of gut microbiota in the development of autoimmune diseases – DovePress
- Autoimmune Diseases: Types, Symptoms & Treatments – Cleveland Clinic
Dr. Emily Zhang, MD, is a gastroenterologist and integrative medicine specialist with 10 years of clinical experience in digestive health and microbiome science. She completed her medical degree at University of Chicago Pritzker School of Medicine and fellowship at Massachusetts General Hospital. Dr. Zhang specializes in gut-brain interactions, microbiota diversity, and nutrition-driven gut repair. She has contributed to NIH-funded studies on probiotics and authored patient education resources on functional gut disorders.