Bone density refers to the amount of minerals primarily calcium and phosphorus stored in your bones. Maintaining good bone density is essential for strong, resilient bones that can resist fractures. As we age, bone mass naturally decreases, but certain lifestyle habits, medical conditions, and hormonal changes can accelerate bone loss. Understanding how to improve bone density is key to preventing osteoporosis and maintaining long term skeletal health.
Key Takeaways
- Bone density (or Bone Mineral Density, BMD) reflects how strong and solid your bones are and how likely they are to fracture.
- Aging, hormonal changes (especially menopause), inactivity, smoking, alcohol, and poor diet all contribute to bone loss.
- Calcium and vitamin D intake, weight-bearing exercise for bones, and healthy lifestyle habits can help improve bone density.
- DEXA scans are the standard test to measure BMD and diagnose osteopenia or osteoporosis.
- Medications and nutritional supplements are available for people at high risk or already diagnosed with low bone density.
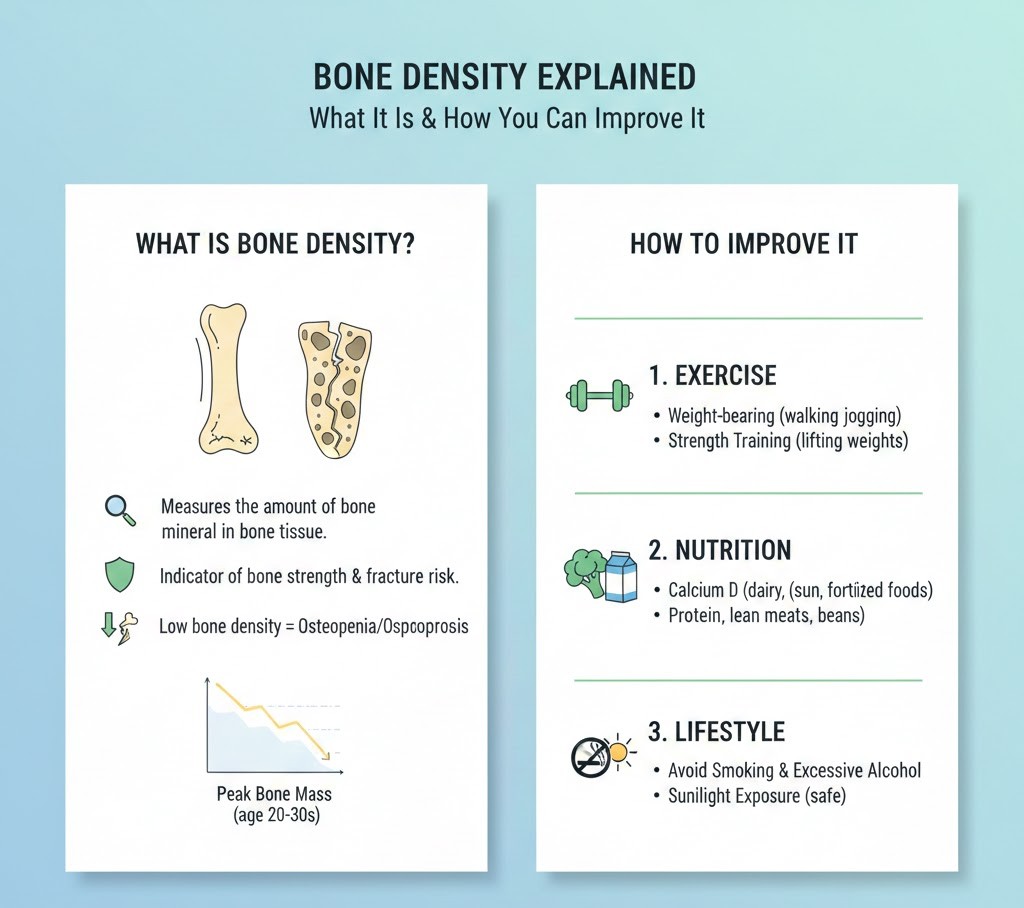
What Is Bone Density?

Bone density describes how tightly packed the minerals are in your bone tissue, usually measured in the spine and hip. Higher skeletal density generally means stronger bones that are better able to handle everyday stress, while lower density means the bone framework has become thinner, weaker, and more fragile. Clinically, Bone Mineral Density (BMD) is measured using a specialized X‑ray, and the results are compared to the bone density of a healthy young adult.
When bone density falls below normal but is not yet in the osteoporosis range, the condition is called osteopenia. If bone density drops further, it becomes osteoporosis, a disease marked by fragile bones and a much higher fracture risk. Improved Bone Density focuses on slowing bone loss, maintaining existing bone mass, and in some cases, slightly rebuilding lost bone to restore bone resilience and integrity.
How Bone Density Changes with Age
Bones are living tissues that continuously remodel, replacing old bone with new bone. During childhood and early adulthood, bone formation is faster than bone breakdown, allowing bone mass to increase and reach its peak between the late teens and late twenties. After about age 30, this balance gradually shifts, and adults begin to lose more bone than they build. These age related changes become more noticeable after 40 and accelerate further with advancing age, especially in women after menopause.
As people get older, several factors contribute to declining bone density, increasing the risk of osteoporosis and fractures. Reduced physical activity, hormonal changes, smaller appetites, and chronic medical conditions all play a role. Protecting Bone Strength and Bone Structure Health through proper nutrition, exercise, and healthy habits becomes essential to maintaining strong bones throughout midlife and beyond.
Factors that accelerate bone density loss with age:
- Menopause and declining estrogen
- Low testosterone in older men
- Low calcium and vitamin D intake
- Sedentary lifestyle or reduced activity
- Chronic health conditions or long term medication use (e.g., steroids)
- Reduced appetite or nutrient absorption in older adults
Bone Density and Osteoporosis
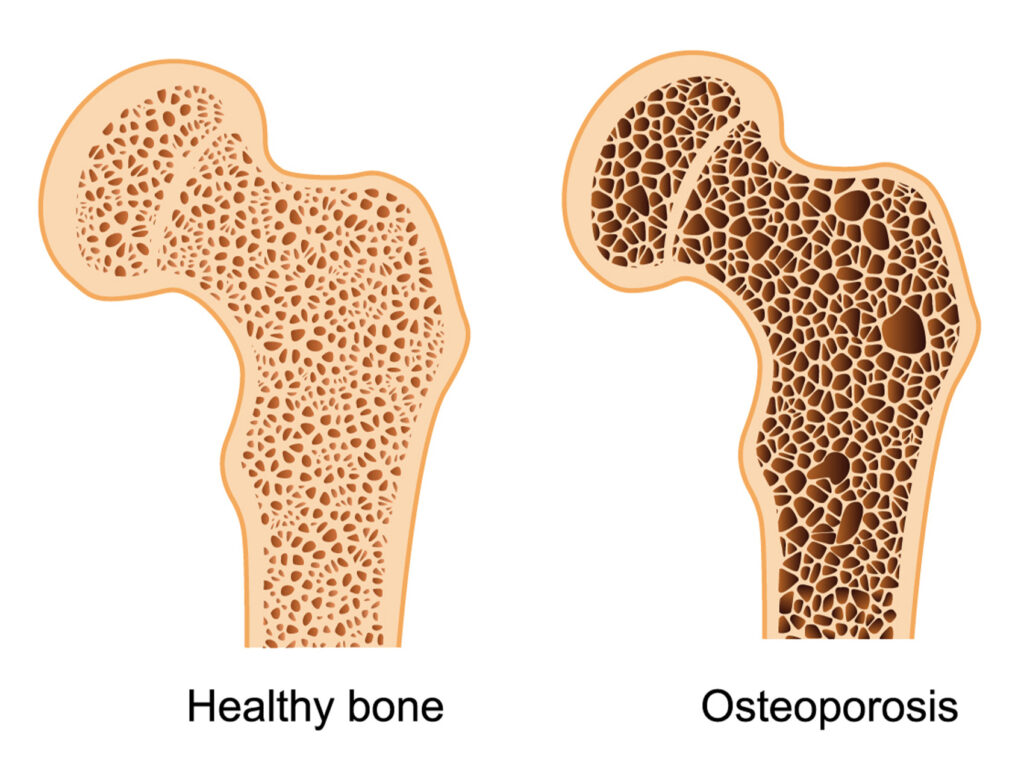
Osteoporosis is a disease characterized by low bone mass and deterioration of bone micro architecture, leading to fragile bones that fracture easily. It is sometimes called a “silent disease” because bone density can decline for years without symptoms until a fracture occurs. Common sites of osteoporotic fractures include the hip, spine, and wrist, which can greatly impact quality of life and independence.
Osteoporosis prevention centers on minimizing bone loss and maximizing bone quality before fractures occur. Improved Bone Density strategies involve nutrition, activity, and often medical treatment for high‑risk individuals. Even if osteoporosis is already present, targeted interventions can help stabilize BMD, reduce fracture risk, and maintain Bone Integrity.
Common Causes and Risk Factors of Low Bone Density
Low bone density develops gradually and is influenced by a combination of lifestyle habits, medical conditions, and natural aging processes. Understanding these risk factors can help you take preventive steps early and protect long term bone strength.
- Aging: Bone naturally becomes thinner with age as bone breakdown begins to exceed bone formation. This process speeds up after age 40 and significantly increases fracture risk.
- Low estrogen or testosterone: Estrogen in women and testosterone in men help maintain bone strength. When these hormone levels drop especially after menopause. Bone loss accelerates rapidly.
- Nutrient deficiencies (calcium & vitamin D): Calcium builds bone structure, while vitamin D helps the body absorb it. Deficiencies weaken bones, reduce mineralization, and raise osteoporosis risk.
- Sedentary lifestyle: Bones require regular weight bearing activity to stay strong. Long periods of sitting or lack of exercise slow bone rebuilding and contribute to bone loss.
- Smoking: Chemicals in cigarettes interfere with bone forming cells and reduce blood flow to bone tissue. Smokers have significantly lower bone density and higher fracture risk.
- Excessive alcohol use: Heavy drinking disrupts calcium balance and hormone levels. It also impairs bone building cells and increases risk of falls and injuries.
- Long term steroid use: Medications like prednisone weaken bones by blocking calcium absorption and slowing new bone formation. Even moderate doses over time can cause bone loss.
- Family history of osteoporosis: Genetics strongly influence bone density. Having a parent or sibling with osteoporosis makes low bone mass more likely.
- Low body weight: Being underweight or having very low body fat reduces estrogen levels and decreases the stress that strengthens bones. This leads to lower bone mass.
- Digestive disorders affecting nutrient absorption: Conditions like celiac disease, Crohn’s disease, and ulcerative colitis prevent proper absorption of bone building nutrients, leading to gradual bone weakening.
How to Improve Bone Density
Improving bone density involves strengthening the bones you have while helping your body slow bone loss and build new bone tissue. This requires a combination of proper nutrition, targeted exercise, healthy lifestyle habits, and, in some cases, medical treatments. Supporting Bone Structure Health consistently over time is the most effective way to prevent osteoporosis and maintain lifelong skeletal strength.
1. Increase Calcium and Vitamin D Intake

Calcium is the primary mineral that forms the foundation of strong bones, while vitamin D enables your body to absorb calcium efficiently. Without enough of these nutrients, bones become brittle, weak, and more prone to fractures. Getting adequate amounts daily is essential for preserving skeletal density and preventing long term bone loss.
Good Sources of Calcium
- Dairy products
- Leafy greens
- Almonds
- Fortified foods
Good Sources of Vitamin D
- Sunlight
- Fatty fish
- Egg yolks
- Supplements (if recommended)
Recommended Daily Intake
- 1,000–1,200 mg of calcium for most adults
- 600–800 IU of vitamin D, though many people require more if levels are low
2. Do Weight-Bearing and Strength Training Exercises

Exercise is one of the most powerful ways to improve bone density because physical stress signals your body to strengthen bone tissue. Weight-bearing exercises force your bones to support your body weight, while strength training increases muscle mass and enhances the skeletal load, stimulating bone formation even further.
Weight-Bearing Activities
- Walking
- Jogging
- Hiking
- Dancing
- Jump rope
Strength Training
- Dumbbells
- Resistance bands
- Bodyweight exercises
3. Adopt Lifestyle Habits That Support Bone Health
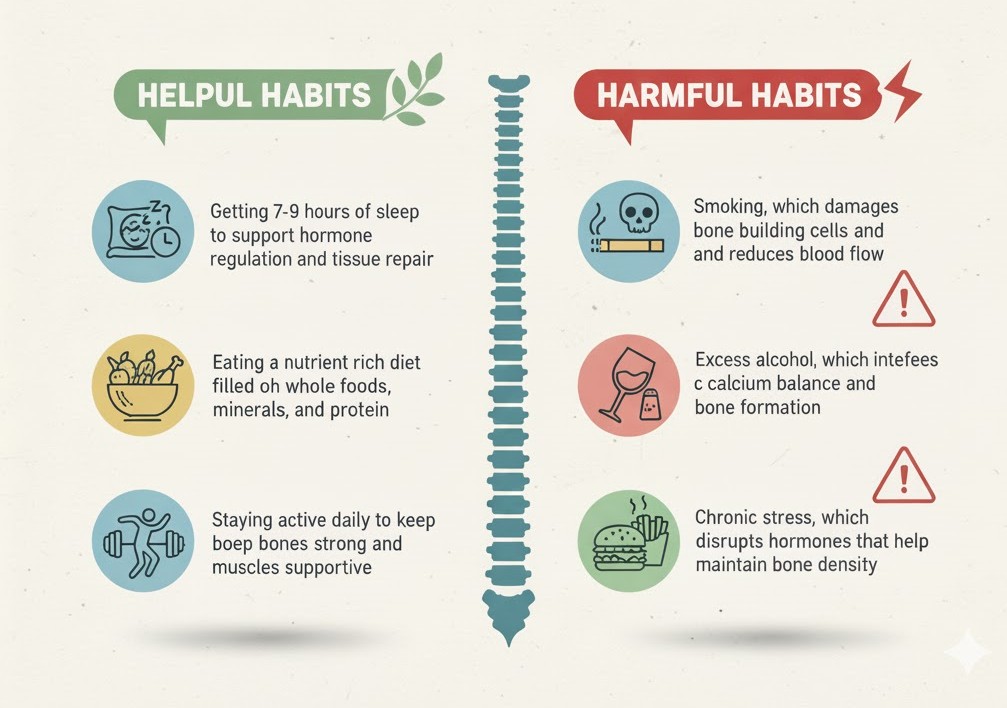
Daily habits play a major role in maintaining strong bones. Positive lifestyle changes can boost bone quality, while harmful habits accelerate bone loss. Supporting your bone resilience requires consistent, healthy routines that nourish and protect your skeletal system.
Helpful Habits
- Getting 7-9 hours of sleep to support hormone regulation and tissue repair
- Eating a nutrient rich diet filled with whole foods, minerals, and protein
- Staying active daily to keep bones strong and muscles supportive
Harmful Habits
- Smoking, which damages bone building cells and reduces blood flow
- Excess alcohol, which interferes with calcium balance and bone formation
- High sodium processed foods, which increase calcium loss
- Chronic stress, which disrupts hormones that help maintain bone density
4. Consider Supplements for Bone Strength
When dietary intake is insufficient, supplements can help fill nutritional gaps that affect bone mineral density. They provide essential nutrients that support bone remodeling, mineralization, and repair especially for individuals with deficiencies, restricted diets, or medical conditions that impair nutrient absorption.
Common supplements include:
- Calcium for structural foundation
- Vitamin D3 to boost calcium absorption
- Magnesium for bone mineralization
- Vitamin K2 to direct calcium into bones instead of soft tissues
- Collagen peptides to support bone matrix and flexibility
- Omega-3 fatty acids to reduce inflammation that contributes to bone loss
5. Medications That Improve Bone Density
For people with osteopenia or osteoporosis, medications may be necessary to prevent fractures or restore lost bone mass. These treatments work by slowing bone breakdown, increasing bone formation, or helping the body retain important minerals.
Types Include:
- Bisphosphonates reduce bone loss and lower fracture risk
- Denosumab slows bone breakdown by targeting specific bone destroying cells
- Hormone replacement therapy (HRT) restores estrogen in postmenopausal women to prevent rapid bone loss
- Selective estrogen receptor modulators (SERMs) mimic estrogen’s protective effects on bones
- Parathyroid hormone analogs stimulate new bone growth and increase bone density
6. Improve Hormonal Balance
Hormones play a major role in regulating bone remodeling, the process where old bone is replaced with new bone. When hormones like estrogen, testosterone, thyroid hormones, or parathyroid hormone fall out of balance, bone breakdown speeds up and bone formation slows down. Maintaining healthy hormone levels through medical guidance, regular checkups, and lifestyle habits can help slow bone loss, especially during menopause or age related hormonal decline.
7. Reduce Inflammation Through Diet and Lifestyle
Chronic inflammation affects how the body absorbs nutrients and can accelerate the activity of bone resorbing cells, increasing the rate of bone loss. An anti inflammatory lifestyle supports healthier bone remodeling and protects against skeletal weakening. Incorporating foods like leafy greens, berries, fatty fish, nuts, and olive oil along with stress management and regular movement can help lower inflammation and promote stronger, more resilient bones.
How Bone Density Is Measured
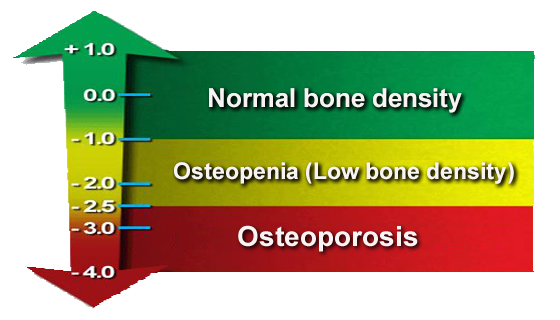
A DEXA scan (Dual-Energy X-ray Absorptiometry) is the standard test used to measure bone density. It is quick, painless, and uses very low radiation. The scan checks areas most likely to fracture such as the hip and spine and provides a T-score that compares your bone mass to that of a healthy young adult.
T-Score Breakdown
| T-Score | Assessment |
| ≥ -1.0 | Normal bone density |
| -1.0 to -2.5 | Osteopenia (low bone mass) |
| ≤ -2.5 | Osteoporosis |
Your report may also include a Z-score, which compares your bone density to people of the same age, helping detect unusual bone loss.
Regular Screening Is Recommended For:
- Women age 65+
- Men age 70+
- Postmenopausal women under 65 with risk factors
- Anyone with a history of fractures
- People on long term steroids or certain medications
- Those with medical conditions affecting bone health
Long Term Complications of Low Bone Density

Left unaddressed, low bone density can weaken bones over time and lead to progressive health issues. As bone strength declines, even minor falls or everyday movements may cause fractures or long term pain. These complications can significantly impact mobility, independence, and overall quality of life.
- Osteoporosis: A severe loss of bone mass that makes bones fragile and highly susceptible to fractures, especially in the spine, hip, and wrists.
- Frequent fractures: Weaker bones break more easily, even from minimal trauma such as bending, coughing, or light falls.
- Loss of height: Compression fractures in the spine can cause the vertebrae to collapse, resulting in noticeable height loss.
- Spinal curvature: Kyphosis, or a forward rounding of the spine, can develop from repeated spinal fractures and weaken posture.
- Chronic back pain: Persistent pain often results from compressed vertebrae or structural changes in the spine.
- Reduced mobility: Pain, stiffness, and fractures can limit your ability to move freely, impacting daily activities.
- Increased disability risk: Severe bone weakness raises the chance of long term disability and dependence on others for everyday tasks.
How to Prevent Osteoporosis
Osteoporosis prevention focuses on strengthening bones early in life and maintaining bone supportive habits throughout adulthood. While some risk factors like age and genetics cannot be changed, lifestyle choices have a major impact on bone health. You can significantly reduce your risk through:
- Daily weight-bearing exercise: Activities like walking, jogging, dancing, or stair climbing stimulate bone growth and slow age related bone loss.
- Adequate calcium & vitamin D: These nutrients are essential for bone mineralization. Aim for regular intake through diet or supplements if needed.
- Avoiding smoking and excess alcohol: Both habits impair bone building cells, lower hormone levels, and accelerate bone loss.
- Strength training: Lifting weights or using resistance bands enhances muscle strength and puts positive stress on bones to keep them dense and durable.
- Bone healthy diet rich in whole foods: Include plenty of vegetables, fruits, lean protein, nuts, seeds, and whole grains to support nutrient absorption and bone repair.
- Regular DEXA scans: Early screening helps detect bone loss before a fracture occurs and allows for timely treatment or lifestyle adjustments.
- Maintaining a healthy body weight: Being underweight increases fracture risk, while a balanced weight supports hormone levels and bone strength.
- Getting enough sleep and managing stress: Poor sleep and chronic stress can disrupt bone remodeling hormones and weaken bone over time.
Conclusion
Bone density refers to the mineral strength of your bones and determines how resistant they are to fractures. It naturally declines with age, especially after menopause, but poor diet, inactivity, smoking, alcohol, and certain medical conditions can accelerate bone loss. Improving bone density involves getting enough calcium and vitamin D, doing weight-bearing and strength training exercises, and maintaining healthy lifestyle habits. Supplements or medications may be needed for those at higher risk. DEXA scans measure bone density and diagnose osteopenia or osteoporosis. Preventing bone loss early helps reduce fractures, maintain mobility, and support long term skeletal health.
FAQs
What is bone density and why is it important?
Bone density measures how much mineral is stored in your bones. Higher bone density means stronger bones that can resist fractures, while low bone density increases the risk of osteopenia, osteoporosis, and long term mobility issues.
What causes low bone density?
Low bone density can develop due to aging, hormonal changes, nutrient deficiencies, inactivity, smoking, excessive alcohol use, long term steroid use, or medical conditions that affect nutrient absorption.
How can I naturally improve my bone density?
Eating enough calcium and vitamin D, doing weight-bearing exercises, lifting weights, managing stress, and avoiding smoking and alcohol all help build and maintain bone mass.
What foods are best for bone health?
Dairy products, leafy greens, almonds, fortified foods, fatty fish, eggs, nuts, seeds, and whole grains provide essential nutrients like calcium, vitamin D, magnesium, and protein that support bone strength.
How do weight-bearing exercises improve bone density?
Activities like walking, jogging, dancing, and strength training place controlled stress on bones, stimulating them to grow stronger and denser over time.
What is a DEXA scan and who needs one?
A DEXA scan measures bone density using a low radiation X-ray. It is recommended for women 65+, men 70+, postmenopausal women under 65 with risk factors, or anyone with fractures or long term steroid use.
What is the difference between osteopenia and osteoporosis?
Osteopenia is mild bone loss where bone density is below normal but not yet severe. Osteoporosis is advanced bone loss that greatly increases fracture risk, especially in the spine, hip, and wrist.
Can bone density increase after age 50?
Yes, while it is more challenging, bone density can improve at any age with proper nutrition, strength training, sufficient vitamin D, and medical treatment when needed.
Do supplements help strengthen bones?
Supplements such as calcium, vitamin D3, magnesium, vitamin K2, collagen, and omega-3s can support bone health when dietary intake is inadequate or nutrient absorption is poor.
How does menopause affect bone density?
After menopause, estrogen levels drop sharply, causing faster bone breakdown. This makes women more susceptible to osteoporosis and fractures.
References
- Anila Lijo. (2025, Sep 30). Bone Density: How To Build Strong Bones. UC Davis. Retrieved Nov 20, 2025, from https://www.ucdavis.edu/research/labs-to-lives/blog/childrens-community-health/bone-density
- Bard, S. (n.d.). How to increase bone density naturally: 11 methods. Medical News Today. Retrieved November 20, 2025, from https://www.medicalnewstoday.com/articles/325903
- Bone Density: What It Is and How to Keep What You’ve Got. (2021, October 14). HSS. Retrieved November 20, 2025, from https://www.hss.edu/health-library/move-better/bone-density
- Osteoporosis: Symptoms, Causes and Treatment. (n.d.). Cleveland Clinic. Retrieved November 20, 2025, from https://my.clevelandclinic.org/health/diseases/4443-osteoporosis
Aubrey Carson is an RDN with 9 years across hospital, outpatient, and private practice settings. They earned an MS in Clinical Nutrition from Tufts University – Friedman School (2016) and completed a Dietetic Internship at Mayo Clinic. Aubrey specializes in micronutrient assessment, evidence-based supplementation, and patient education. Their work includes CE presentations for the Academy of Nutrition and Dietetics and collaborations with Mass General Brigham on nutrition education resources.

