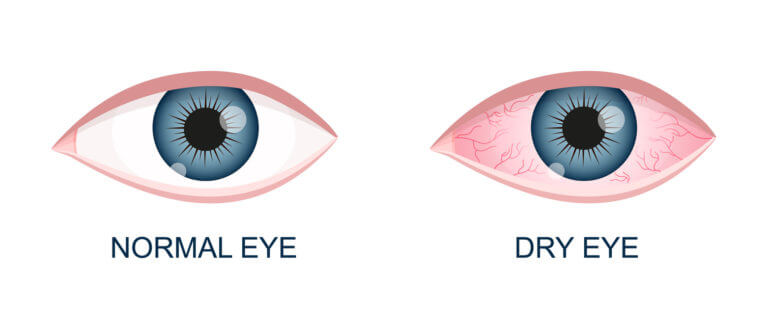
Dry eye syndrome occurs when tears are insufficient or evaporate quickly, destabilizing the tear film and irritating the eye surface. Multiple causes, from gland dysfunction to lifestyle disease, guide diagnosis, treatment, and prevention strategies.
Key Takeaways
- Tear film has lipid, aqueous, and mucin layers; disruption in any layer destabilizes the ocular surface and leads to discomfort, inflammation, and fluctuating vision.
- Major causes include age-related lacrimal decline, autoimmune disease, medications, Meibomian gland dysfunction, eyelid disorders, contact lenses, hormonal shifts, nutritional deficits, allergies, skin disease, and harsh, low-humidity or polluted environments.
- Diagnosis relies on history, slit-lamp inspection, tear breakup time, Schirmer’s strips, meibography of Meibomian glands, and tests for inflammatory markers to define subtype and severity.
- Management is cause-based: lubricants, anti-inflammatory drops, punctal plugs, warm compresses, lid hygiene, systemic and hormonal control, lifestyle changes, plus emerging drugs and biomarker-guided, personalized therapies targeting immune and glandular dysfunction.
What is Dry Eye Syndrome?
Dry eye syndrome happens when your eyes don’t produce enough tears or when the tears evaporate too quickly. Healthy tears are essential they keep the eye surface moist, protect against infections, and provide clear vision.
In recent years, dry eye has become more widespread. Lifestyle changes, especially increased screen use, along with aging and environmental stress, play a major role in its rising prevalence.
Tear Film Anatomy and Physiology
To understand why dry eye develops, it is important to know how the tear film works. The tear film is a very thin but essential layer that covers the surface of the eye. It keeps the eye moist, protects it from infections, and provides a smooth surface for clear vision. The tear film has three main parts, each with a unique role:
- Lipid layer: This is the outermost oily layer, produced by the Meibomian glands found along the eyelid margins. Its main function is to prevent tears from evaporating too quickly. Without a healthy lipid layer, tears dry out fast, leading to dry eye symptoms.
- Aqueous layer: The middle, watery layer is secreted by the lacrimal glands located above the outer corner of each eye. This layer supplies moisture, electrolytes, and important nutrients. It also flushes away debris and protects against infections.
- Mucin layer: This is the innermost layer, closest to the eye surface. It is made up of mucus-like substances that help the watery tears spread evenly across the eye. By attaching tears to the eye’s surface cells, the mucin layer ensures uniform hydration and lubrication.
All three layers work together in balance to keep eyes comfortable and functioning well. If any layer is deficient or disrupted, the tear film becomes unstable, leading to dryness, irritation, and potential damage to the eye surface. This understanding forms the basis for diagnosing and treating dry eye syndrome effectively.
Major Causes of Dry Eye Syndrome: Detailed Explanation
Dry eye syndrome is complex and rarely caused by a single issue. It typically results from multiple overlapping factors that affect tear quantity, quality, or both. Here is an in-depth look at the major causes of dry eye syndrome.
Aqueous Tear Deficiency
This type involves decreased tear production, meaning the eyes do not supply enough watery tears to keep the surface moist. Causes include:
- Aging: As people age, lacrimal glands that produce the aqueous layer naturally decline in function, reducing tear volume.
- Autoimmune Diseases: Conditions like Sjögren’s syndrome, rheumatoid arthritis, and lupus target and damage tear-producing glands, significantly reducing tears.
- Medications: Many common drugs reduce tear secretion, including antihistamines, antidepressants, some blood pressure medicines, diuretics, and hormonal therapies.
- Eye Surgeries: Procedures like LASIK and cataract surgery may temporarily impair tear gland function by damaging corneal nerves that stimulate tear production.
Evaporative Dry Eye
In this form, tear production may be normal, but tears evaporate too quickly due to disruptions in the outer oily layer. Key causes include:
- Meibomian Gland Dysfunction (MGD): Blockage or malfunction of eyelid oil glands reduces the lipid layer that prevents evaporation. This is the leading cause of evaporative dry eye.
- Eyelid Problems: Conditions such as ectropion (outward turning of the eyelid) or entropion (inward turning) prevent proper tear distribution.
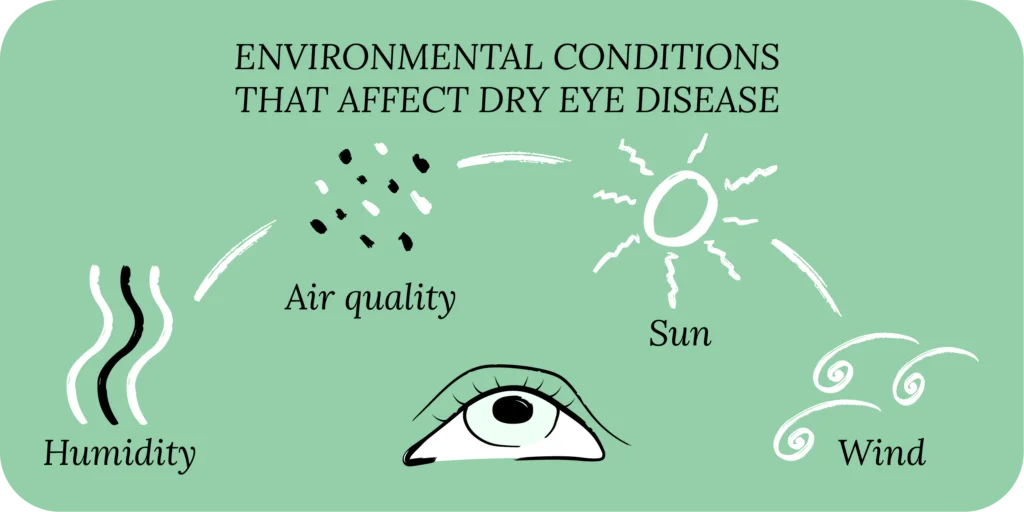
- Environmental Stress: Exposure to dry air, wind, pollution, smoke, or indoor heating and air conditioning lowers humidity and speeds tear evaporation.
- Prolonged Screen Use: Reduced blinking during computer or smartphone use causes faster tear loss.
- Preservatives in Eye Drops: Long-term use of certain artificial tears containing preservatives can irritate the eye surface and worsen dry eye.
Hormonal and Systemic Influences
Systemic health and hormonal changes significantly affect tear production and quality:
- Postmenopausal Hormonal Changes: Declines in estrogen and androgen levels lead to thinner tear film and lower production.
- Thyroid Disorders: Imbalances can influence gland function associated with tear secretion.
- Contact Lens Wear: Continuous use interferes with tear film stability and reduces oxygen supply to the cornea, increasing dryness risk.
Other Contributors
Several less obvious factors also influence dry eye:
- Nutritional deficiencies : such as vitamin A deficiency impair mucin production vital for tear stability. A diet rich in foods that boost eye health supports better tear film quality.
- Allergic Eye Disease: Chronic inflammation from allergies reduces tear quality.
- Skin Conditions: Disorders like rosacea and seborrheic dermatitis inflame eyelids and meibomian glands, impairing oily tear layer production.
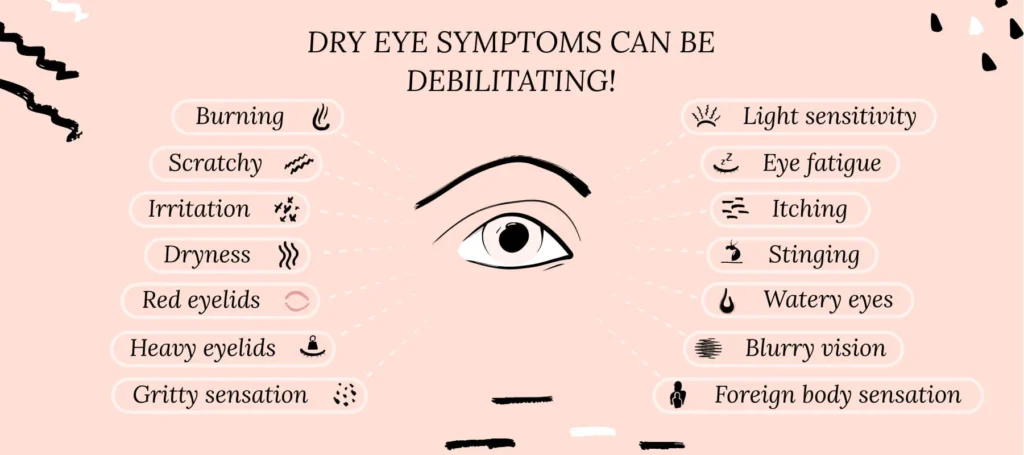
Each of these causes disrupts the delicate balance of the tear film, leading to symptoms like itchy dry eyes, irritation, burning, and fluctuating vision. Identifying the interplay of these factors is crucial for effective diagnosis and individualized treatment strategies for dry eye syndrome.
Diagnostic Approaches to Identify Causes
Pinpointing the exact cause of dry eye is crucial for effective treatment. Eye doctors use a combination of methods:
- Medical history: Reviewing symptoms, lifestyle, and health conditions.
- Slit lamp exam: Checking eye surface and glands under magnification.
- Tear Breakup Time (TBUT): Measuring how quickly tears evaporate.
- Schirmer’s test: Gauging tear volume with special strips of paper.
- Meibography: Imaging to assess Meibomian gland structure.
- Inflammation markers: Detecting immune-related problems in tear composition.
Lifestyle & Environmental Risk Factors for Dry Eye
Daily habits and surroundings often worsen dry eye. Common risks include:
- Low-humidity environments: Indoor settings with air conditioning or heating systems dry out the air, accelerating tear evaporation. This dry air disrupts the natural tear film and causes the eyes to feel gritty and irritated.
- Excessive screen time: Prolonged use of computers, smartphones, and tablets reduces the blink rate. Blinking moistens the eyes and spreads tears evenly; fewer blinks result in faster tear evaporation and worsened dryness.
- Poor sleep: Lack of restful sleep limits the eyes’ natural overnight repair processes. During sleep, tear production and eye surface healing occur. Poor sleep disrupts this and can worsen dry eye symptoms.
- Smoking: Tobacco smoke contains toxins that damage the tear film and eye surface. Smoking increases oxidative stress and inflammation, making eyes more vulnerable to dryness.
- For lifestyle-related issues: Dietary improvements like adding omega-3 fatty acids for dry eyes support better tear quality. Taking regular screen breaks following the 20-20-20 rule reduces evaporative stress. Humidifiers add moisture to dry indoor air. Avoiding exposure to smoke and pollutants protects tear film integrity.
Managing and Preventing Dry Eye Based on Cause
Treatment depends on addressing the root problem rather than just soothing symptoms.
- For tear deficiency: When tear production is low, increasing moisture on the eye surface is essential. Artificial tears or lubricating eye drops replenish fluids. Punctal plugs may be used to partially block tear drainage ducts, helping retain natural tears longer. Anti-inflammatory eye drops reduce inflammation that impairs tear production.
- For evaporative dry eye: This form stems from problems with the oily lipid layer that prevents tear evaporation. Warm compresses applied to the eyelids help melt blocked oils in Meibomian glands. Regular eyelid hygiene, including gentle cleaning, can reduce inflammation and bacterial buildup. Specific medical treatments may target Meibomian Gland Dysfunction directly to restore oil secretion.
- For hormonal or systemic factors: Hormonal imbalances like those in menopause affect tear quality. Supporting these patients with hormone therapies or supplements can improve symptoms. Thyroid disorders should be managed with appropriate medical care. Reviewing medications that contribute to dry eye and adjusting them under supervision also helps.
- For lifestyle-related issues: Dietary improvements like adding omega-3 fatty acids support better tear quality. Taking regular screen breaks following the 20-20-20 rule reduces evaporative stress. Humidifiers add moisture to dry indoor air. Avoiding exposure to smoke and pollutants protects tear film integrity.
Future Directions and Research in Dry Eye Causes
Advances in eye research continue to uncover new insights into dry eye. Current areas of focus include:
- Research in dry eye syndrome is rapidly evolving, revealing new insights that promise improved diagnosis and treatment. Key areas of focus include:
- Immune and Inflammatory Pathways
Scientists are gaining a deeper understanding of how the immune system contributes to chronic dry eye. Inflammation plays a central role in damaging tear glands and eye surface tissues. Targeting these pathways can reduce symptoms and prevent progression. - Tear Biomarkers for Early Detection
Advanced tests analyzing tear chemistry aim to identify specific biomarkers. These biomarkers help detect dry eye earlier and classify its subtypes, allowing for timely and precise treatment before severe damage occurs. - Next-Generation Drugs
New medications are being developed to directly stimulate Meibomian gland function, reduce inflammation, and restore tear film stability. These drugs offer hope for more effective management compared to traditional artificial tears. - Personalized Medicine Approaches
Future treatments will be tailored to individual patients based on their unique tear film profiles, underlying causes, and genetic factors. This personalized approach aims to maximize treatment efficacy and minimize side effects.
Conclusion
Dry eye syndrome happens when tear production is insufficient or tears evaporate too fast, leading to dryness and irritation. Tears keep eyes moist and protect vision. The tear film has three layers oily, watery, and mucin each vital to eye health. Lifestyle factors like increased screen time, aging, and environment contribute to dry eye’s rise. Disruption in any tear layer can cause symptoms and damage. Knowing this helps target treatments for lasting relief and eye comfort.
FAQs
What is the difference between aqueous-deficient and evaporative dry eye?
Aqueous-deficient dry eye occurs when the lacrimal glands produce an insufficient amount of watery tears, leading to dryness and irritation due to inadequate eye surface hydration. This can be caused by aging, autoimmune diseases like Sjögren’s syndrome, certain medications, or eye surgeries that affect tear production.
At what age does dry eye become more common?
Dry eye becomes increasingly common with age. Studies show prevalence rises significantly after age 50, affecting about 30% or more of people over 65. Women, especially postmenopausal, are more often affected due to hormonal changes that reduce tear production. Aging reduces lacrimal gland function and thins the tear lipid layer, both leading to instability of the tear film.
Can autoimmune diseases cause dry eye?
Yes, autoimmune conditions are major contributors. Sjögren’s syndrome specifically targets the tear and saliva glands, causing severe dry eye and mouth symptoms. Rheumatoid arthritis, lupus, and other autoimmune disorders can also impair tear gland function through chronic inflammation, resulting in reduced tear production and ocular surface damage.
Does screen time cause dry eye?
Extended screen time is a significant risk factor. When focusing on digital devices, the blink rate decreases by up to 60%, reducing tear spread and causing faster evaporation. Screens also increase exposure to blue light and dry air from cooling systems, worsening symptoms. Taking frequent breaks and consciously blinking can help mitigate these effects.
Are certain medications linked to dry eye?
Many medications can reduce tear production or alter tear composition. Common ones include antihistamines used for allergies, antidepressants, blood pressure medications like beta-blockers, diuretics, and hormonal drugs. It’s important for patients on these medications to monitor symptoms and discuss alternatives with healthcare providers if dry eye develops.
How do hormonal changes impact dry eye?
Hormonal fluctuations, particularly decreases in estrogen and androgen levels after menopause, play a major role. These hormones regulate tear gland secretion and the quality of the tear film, including the oil layer. Thyroid disorders can similarly affect gland function and tear production, contributing to dry eye.
Can contact lenses worsen dry eye?
Yes. Contact lenses interrupt the natural tear film, causing mechanical irritation and reducing the supply of oxygen to the cornea. This disrupts tear stability and increases evaporation, making dry eye symptoms worse, especially if lenses are worn long hours or overnight.
Can eyelid problems cause dry eye?
Eyelid conditions like blepharitis (inflammation of eyelid margins) and malpositions such as entropion or ectropion impair Meibomian gland function and tear distribution. This leads to reduced lipid layer secretion and uneven tear spread, promoting dryness and irritation.
Is diet important for dry eye prevention?
Diet plays a key role. Omega-3 fatty acids found in fish and flaxseed support healthy Meibomian gland function and improve tear quality. Vitamin A is essential for mucin production, helping tears adhere to the eye surface. Deficiencies in these nutrients worsen dry eye symptoms.
How do environmental factors influence dry eye?
Environmental conditions greatly impact tear evaporation. Dry, windy, and polluted air increase tear film break-up and ocular surface stress. Indoor climate control systems often reduce humidity, leading to faster tear evaporation. Protecting eyes from harsh environments helps maintain tear stability and reduce symptoms.
Reference
- Mayo Clinic: Dry Eyes – Symptoms & Causes
https://www.mayoclinic.org/diseases-conditions/dry-eyes/symptoms-causes/syc-20371863 - National Eye Institute (NEI): Dry Eye
https://www.nei.nih.gov/learn-about-eye-health/eye-conditions-and-diseases/dry-eye - Cleveland Clinic: Dry Eyes – Types, Symptoms, Causes & Treatment
https://my.clevelandclinic.org/health/diseases/24479-dry-eye - Healthline: Types of Dry Eye – Evaporative vs. Aqueous-Deficient
https://www.healthline.com/health/types-of-dry-eye - PubMed Central (PMC): Dry Eye Syndrome – StatPearls
https://www.ncbi.nlm.nih.gov/books/NBK470411/ - WebMD: Dry Eye Irritants and Environmental Factors
https://www.webmd.com/eye-health/dry-eye-irritants - EyeWiki: Dry Eye Syndrome
https://eyewiki.org/Dry_Eye_Syndrome
Dr. Amiah Rainey researches diet–disease relationships with expertise in vitamins, minerals, and biomarker methods. She earned a PhD from Harvard T.H. Chan School of Public Health (2019) and completed a postdoctoral fellowship at the NIH/NIDDK. With ~20 peer-reviewed publications (example) and experience on NIH-funded cohort studies, Amiah translates complex evidence into practical guidance. She advises on study design, evidence grading, and data transparency. Profiles: ORCID, Google Scholar; list affiliations and any disclosures.

