
Your liver silently supports detoxification, metabolism, and digestion but when stressed, it signals through subtle symptoms like fatigue, dark urine, itching, or jaundice. Identifying these early can prevent serious damage such as cirrhosis or liver failure. Most liver issues are reversible when detected and managed promptly through screening, lifestyle adjustments, and medical care.
Key Takeaways
- Early warning signs: jaundice, dark urine, pale stools, persistent fatigue, unexplained itching.
- High-risk groups: people with obesity, diabetes, alcohol use, or multiple medications.
- Fatty liver disease progresses silently and is common in metabolic syndrome.
- Certain drugs, alcohol, and supplements can cause hidden liver injury.
- Routine liver tests and ultrasound enable early diagnosis and prevention.
- Timely lifestyle correction—healthy diet, weight control, and limited alcohol can reverse early liver stress.
Key Takeaways
- Early symptoms include jaundice, dark urine, pale stools, persistent fatigue, and unexplained itching.
- Fatty liver disease is often silent, especially in people with obesity or diabetes.
- Medication, alcohol, or certain supplements can trigger liver injury.
- Routine blood tests and ultrasound can detect liver damage early.
- Seek urgent care for jaundice with fever, confusion, or internal bleeding signs.
- Healthy habits and timely screening can reverse or prevent liver disease progression.
Why Early Detection Matters
Your liver is central to detoxifying the blood, processing nutrients, storing energy, and producing vital proteins involved in clotting. It also plays a key role in regulating metabolism and maintaining your body’s overall chemical balance. When damage begins to build up, liver function gradually declines often long before any noticeable symptoms appear. Detecting these changes early can make a major difference, allowing time for reversal or stabilization before more serious conditions like cirrhosis, liver failure, or liver cancer develop.
What the Liver Does in Everyday Life
Your liver works quietly behind the scenes, performing hundreds of vital tasks every single day to keep your body functioning smoothly. Even when you’re resting, it’s busy cleaning your blood, managing nutrients, and supporting digestion. Without it, your body couldn’t process food, store energy, or filter out toxins effectively.
Your liver’s jobs include:
- Filtering toxins, drugs, and waste from blood
- Metabolizing fats, proteins, carbohydrates
- Producing bile to digest fats
- Storing vitamins, iron, glycogen
- Synthesizing clotting factors and key proteins
Who Is at Higher Risk
While anyone can experience liver problems, certain factors make some people more vulnerable than others. Understanding your personal risk can help you recognize early warning signs and take preventive steps before serious damage occurs. Often, these risks overlap, increasing the strain on your liver over time.
Common risk factors include:
- Metabolic risks: obesity, insulin resistance, type 2 diabetes, high cholesterol; these raise risk of fatty liver disease.
- Alcohol and toxin use: heavy drinking, long-term exposure to chemicals, misuse of supplements or medications like acetaminophen.
- Viral, autoimmune, or genetic causes: hepatitis B or C, autoimmune hepatitis, hemochromatosis, Wilson disease, primary biliary or sclerosing cholangitis.
- Cholestatic or bile-duct issues: gallstones, bile duct strictures or blockages.
Early Signs of Liver Stress
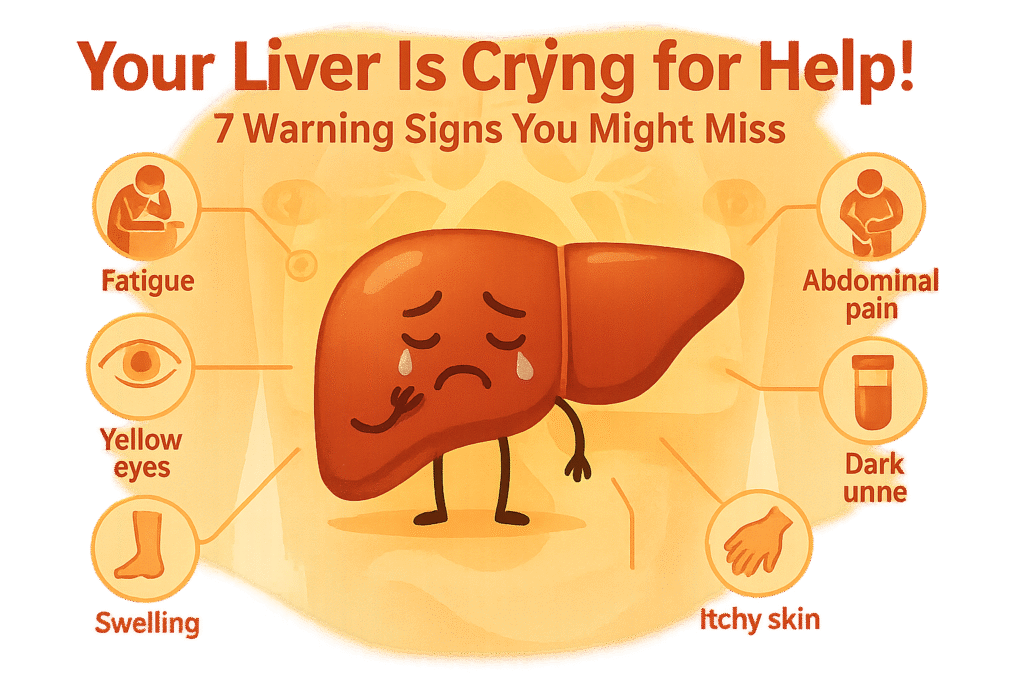
Below are some common warning signals that your liver may be under stress. Not all appear in every case, and many develop gradually over time. It’s important to watch for patterns or persistent combinations of symptoms rather than isolated mild complaints.
- Jaundice (Yellowing of Skin or Eyes): Jaundice occurs when bilirubin, a yellow pigment produced from the breakdown of red blood cells, builds up in the blood because the liver cannot process or excrete it properly. The excess bilirubin deposits in the skin and the sclera (whites of the eyes), causing the characteristic yellow color. This is often a key “red-flag” symptom indicating significant liver dysfunction or bile flow obstruction.
- Itching Without Rash (Pruritus): Persistent itching, especially on the palms and soles, often worse at night, can occur even without any visible skin changes. This happens due to cholestasis, a condition in which bile flow is reduced or blocked. Bile acids accumulate in the skin, triggering nerve endings and causing itching.
- Dark Urine and Pale or Clay-Colored Stools: When the liver fails to properly process bilirubin, it can be excreted in the urine instead of the intestine. This makes the urine dark, like tea or cola. At the same time, a lack of bile in the intestines leads to pale, gray, or clay-colored stools, since bile gives stool its normal brown color.
- Upper Right Abdominal Discomfort or Bloating: A dull ache or pressure under the right rib cage may indicate liver enlargement or stretching of the liver capsule. Swelling of the liver due to inflammation, fatty buildup, or congestion can produce this discomfort or a sense of fullness.
- Severe Fatigue and Weakness: The liver is central to energy metabolism. When it’s not functioning properly, the body’s energy production is impaired, leading to persistent fatigue and weakness, even after adequate rest.
- Nausea, Poor Appetite, Early Satiety, or Unintentional Weight Loss: Liver inflammation or dysfunction can affect digestion and metabolism. Nausea, loss of appetite, early fullness, and unexplained weight loss are often early systemic signs of liver stress or disease.
- Easy Bruising or Bleeding: The liver produces most clotting factors. If liver function is compromised, clotting is impaired, leading to easy bruising, frequent nosebleeds, or prolonged bleeding from minor injuries.
- Swelling in Legs, Ankles, or Abdomen (Ascites): When the liver cannot manage fluid balance properly, fluid accumulates in the abdominal cavity (ascites) or in the lower limbs. This is a sign of serious liver impairment, often seen in advanced disease such as cirrhosis.
- Spider Angiomas and Palmar Erythema: Hormonal imbalances caused by liver dysfunction can lead to vascular changes. Spider angiomas are small, spider-like blood vessels visible on the skin, and palmar erythema is redness of the palms. Both are common physical signs of liver disease.
- Cognitive Changes, Brain Fog, or Sleep Disturbances: Toxins that are normally cleared by the liver, such as ammonia, can build up in the blood when the liver fails. This can affect brain function, causing confusion, forgetfulness, poor concentration, and disrupted sleep patterns a condition called hepatic encephalopathy.
- Changes in Skin, Nails, or Hair: Chronic liver disease can cause hyperpigmentation (dark patches on skin), Terry’s nails (white, glassy nails), brittle hair, or acanthosis nigricans (dark, velvety patches of skin). These changes reflect systemic metabolic disturbances and prolonged liver dysfunction.
The Silent Challenge: Fatty Liver (MASLD / NAFLD)
Fatty liver disease is among the most common liver conditions globally, yet it often progresses quietly without obvious symptoms. Many people remain unaware they have it until routine blood tests or imaging studies reveal early liver changes. Because the disease can advance silently, individuals with metabolic risk factors such as obesity, insulin resistance, type 2 diabetes, or high cholesterol should consider regular liver screening. Early detection allows timely lifestyle or medical interventions, preventing progression to inflammation, fibrosis, or more severe liver complications.
Medications, Alcohol & Supplement Triggers
Certain substances can put extra strain on your liver. Some medications and supplements that seem harmless can cause liver inflammation or injury over time. Always read warning labels and follow dosage instructions carefully.
- Acetaminophen (especially in high doses)
- Certain over-the-counter pain relievers (NSAIDs)
- Herbal supplements such as kava, comfrey, or green tea extract (in excess)
- Anabolic steroids and performance-enhancing drugs
- High-dose vitamins or detox supplements taken without medical supervision
When to Seek Urgent Care
Some symptom combinations require same-day medical attention. Seek urgent evaluation if you experience:
- Jaundice accompanied by fever or chills
- Confusion, disorientation, or altered mental state
- Vomiting blood or passing black, tarry stools
- Rapidly worsening swelling or abdominal pain
- Bleeding that won’t stop or easy bruising
What Happens When You See a Doctor
A thorough medical evaluation helps identify the cause, severity, and treatment plan for liver issues. Typical steps include:
- Review of medical history: including medication, alcohol, and supplement use
- Physical examination: checking for abdominal tenderness, swelling, or skin changes
- Blood tests: liver enzymes (AST, ALT, ALP, GGT), bilirubin, albumin, and clotting factors
- Imaging: ultrasound, FibroScan, or elastography to assess fat buildup and fibrosis
- Advanced diagnostics: CT/MRI scans or a liver biopsy if the diagnosis remains unclear
Tracking & Self-Monitoring Cues
Keeping an eye on small daily changes can help detect liver stress early and assist your doctor in managing your health. You can monitor:
- Daily or weekly weight and waist measurements
- Color changes in stool and urine
- Severity and timing of itching episodes
- Introduction of new medications or supplements
- Patterns of fatigue, concentration, or mood changes
Prevention Strategies That Work
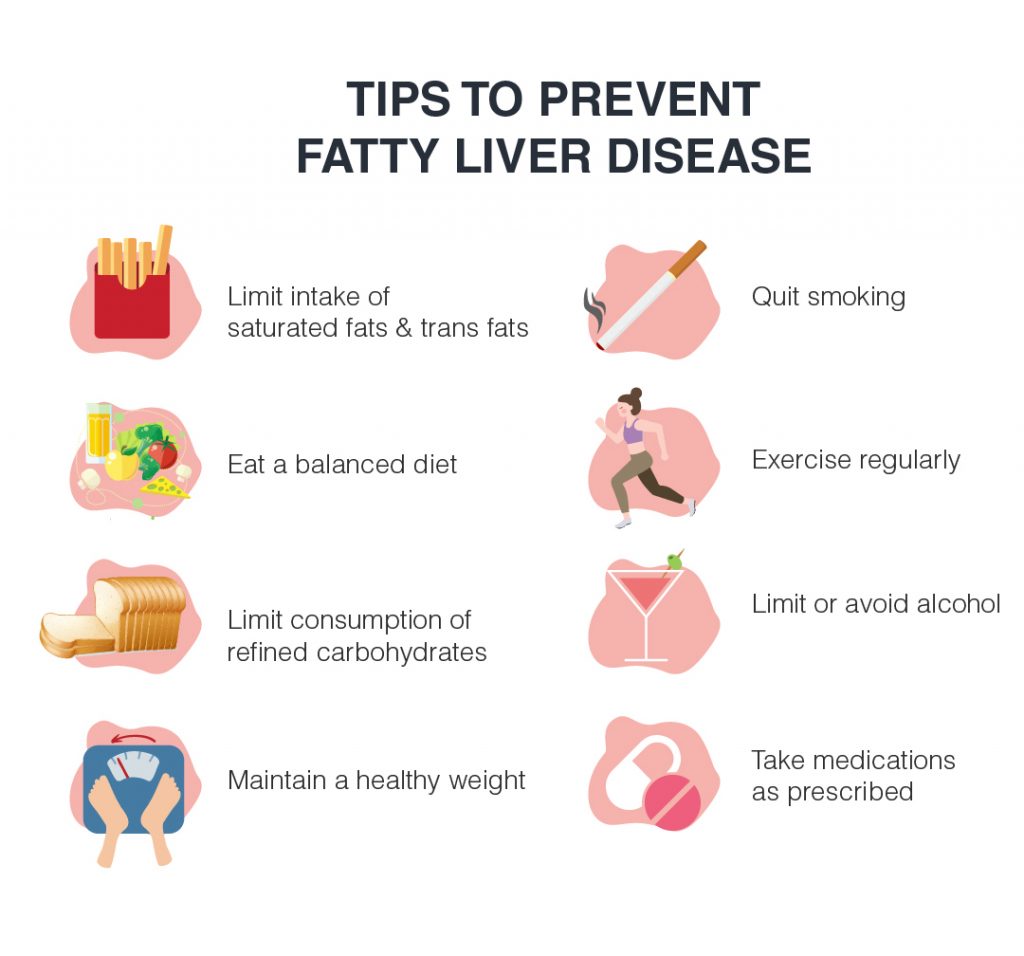
Not all liver diseases can be entirely prevented, but many risk factors are manageable through conscious lifestyle choices and regular medical check-ups. Protecting your liver involves a combination of healthy habits, vaccinations, and proactive monitoring. Key strategies include:
- Limit or avoid alcohol based on medical guidance to reduce liver strain.
- Maintain a healthy weight and manage conditions like diabetes, high cholesterol, and high blood pressure.
- Get vaccinated against hepatitis A and B to prevent viral liver infections.
- Review medications and supplements with your doctor regularly, as some can affect liver function.
- Undergo regular liver screening if you have metabolic risks, viral infections, or a family history of liver disease.
Adopting these measures can significantly reduce the risk of liver damage and support long-term liver health.
Myths Versus Facts
Below are common misunderstandings clarified with evidence:
| Myth | Fact |
| The liver always hurts when it’s diseased. | Most liver conditions cause no pain until very late stages. |
| Detox teas or cleanses can repair the liver. | There’s no scientific proof they help; some may even damage the liver. |
| Only people who drink alcohol get liver disease. | Many cases occur in non-drinkers due to obesity, diabetes, or viral infections. |
| Normal liver enzymes mean your liver is healthy. | Liver tests can appear normal even when silent damage exists. |
| Once the liver is damaged, nothing can be done. | Early treatment and lifestyle changes can slow, stop, or reverse damage. |
| Liver problems are always easy to spot. | Early symptoms are often subtle, such as fatigue, itching, or mild nausea. |
Special Situations to Watch
While liver issues can affect anyone, certain groups of people need to be extra cautious. In these situations, symptoms may appear differently or progress faster, making regular check-ups and early testing even more important. Recognizing the signs early can prevent complications for both short- and long-term health.
Groups that require special attention include:
- Pregnancy: During pregnancy, a condition called intrahepatic cholestasis of pregnancy can develop. It often presents as intense itching (especially on the palms and soles), usually worse at night, along with dark urine and pale stools. These symptoms should never be ignored early detection is essential to protect both mother and baby.
- Children and Teens: Fatty liver disease is becoming increasingly common among young people, largely due to rising rates of obesity and poor diet habits. Because symptoms are often subtle or absent, routine check-ups and blood tests are key for early diagnosis and prevention.
- Older Adults: In older adults, multiple medications and slower metabolism can put extra strain on the liver. Symptoms like fatigue, loss of appetite, or mild confusion may be mistaken for aging, but they can indicate liver stress. Regular monitoring and medication review can make a big difference.
Conclusion
Your liver is vital for keeping your body clean, nourished, and balanced, yet it rarely signals trouble until damage has advanced. Learning to spot early warning signs such as fatigue, dark urine, itching, or jaundice can help detect issues before they become life-threatening. Liver problems aren’t limited to alcohol use; conditions like fatty liver, viral infections, or medication side effects are now common causes. Regular check-ups, balanced nutrition, and responsible medication use can protect your liver and even reverse early damage. If symptoms appear, seek medical advice promptly rather than waiting for pain or obvious illness. Awareness and prevention are your best protection against liver disease.
Frequently Asked Questions
What is the earliest symptom I should pay attention to?
Itching (without visible rash), dark urine, and pale stools are often among the earliest changes before more dramatic symptoms.
Can liver disease exist even if my liver enzymes are normal?
Yes. Some people, especially early in disease, can show normal enzyme levels yet have damage visible on imaging or biopsy.
What is the difference between fatty liver and NASH (nonalcoholic steatohepatitis)?
Fatty liver (MASLD/NAFLD) involves fat accumulation without significant injury. NASH includes inflammation and cell damage, which can progress to fibrosis.
Which over-the-counter medications or supplements commonly harm the liver?
High doses of acetaminophen, some herbal remedies (kava, green tea extract in excess), anabolic steroids, and large doses of vitamins can stress the liver.
When should I go to the emergency department rather than wait for an appointment?
Go urgently if you have jaundice plus fever, mental confusion, vomiting blood or black stools, rapidly worsening swelling or bleeding.
Should I get screened if I have risk factors but no symptoms?
Yes. With obesity, diabetes, metabolic syndrome, or family history, screening (lab tests, imaging) can catch disease early before symptoms begin.
How is liver-related itching different from common dry skin itch?
Liver-itch tends to worsen at night, occurs on palms/soles, lacks rash, resists moisturizing, and is linked to lab abnormalities.
What tests confirm liver trouble?
Doctors use panels of liver enzymes, bilirubin levels, albumin, clotting tests, viral markers, then imaging (ultrasound, FibroScan) or biopsy when needed.
Do only people who drink alcohol get cirrhosis?
No. Metabolic causes (obesity, diabetes), viral hepatitis, autoimmune and cholestatic diseases also lead to cirrhosis.
Can symptoms reverse if I intervene early?
Yes, In many cases lifestyle changes, controlling risk factors, and managing disease early can halt progression or even partially reverse damage.
Aubrey Carson is an RDN with 9 years across hospital, outpatient, and private practice settings. They earned an MS in Clinical Nutrition from Tufts University – Friedman School (2016) and completed a Dietetic Internship at Mayo Clinic. Aubrey specializes in micronutrient assessment, evidence-based supplementation, and patient education. Their work includes CE presentations for the Academy of Nutrition and Dietetics and collaborations with Mass General Brigham on nutrition education resources.

