Testosterone levels naturally decrease with age in both men and women, affecting energy, strength, mood, and sexual health. This gradual hormonal decline begins around age 30 and can influence physical and emotional well-being, making early recognition and proactive management crucial for healthy aging.
Key Takeaways
- Average testosterone drops about 1% yearly after age 30 in men; women see a faster decline after menopause.
- Symptoms include fatigue, low libido, mood shifts, muscle loss, and reduced bone density.
- Accelerated by obesity, chronic illness, poor sleep, stress, smoking, and alcohol use.
- Diagnosis confirmed through blood testing of total and free testosterone levels.
- Managed with lifestyle changes, resistance exercise, weight control, and good sleep.
- Medical options like TRT or supplements require medical supervision due to potential risks.
- Early detection and consistent monitoring help preserve vitality and hormonal balance with age.
Testosterone: Roles and Regulation
Testosterone is a vital hormone produced mainly in the testes in men and the ovaries and adrenal glands in women. It plays a central role in building muscle mass, maintaining bone density, supporting libido, and influencing mood and cognitive function. The brain and pituitary gland regulate testosterone production through a feedback system, adjusting levels based on the body’s needs.
Research published in the Journal of Clinical Endocrinology & Metabolism highlights that testosterone is essential not only for physical health but also for emotional well-being. Both high and low levels can have wide-ranging effects, making balanced regulation crucial for day-to-day life.
How Testosterone Levels Change with Age in Men
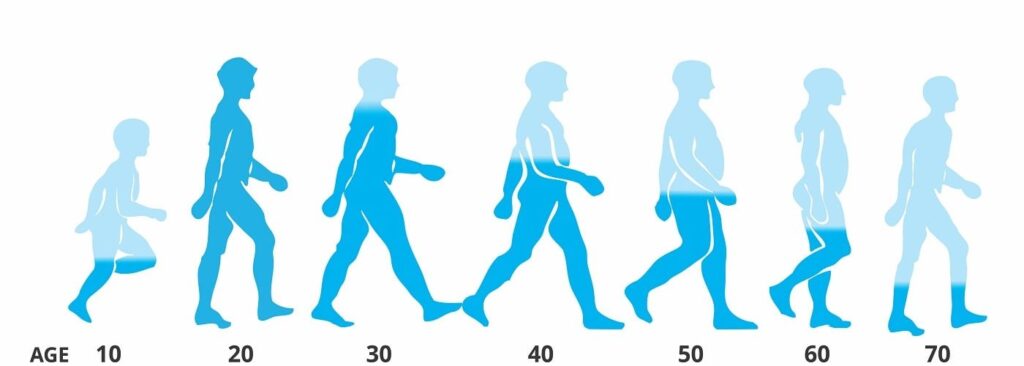
As men age, testosterone levels naturally decrease. This decline usually begins around age 30 and drops by about 1% each year after that. According to a study by the Massachusetts Male Aging Study, roughly 30% of men over age 60 have low testosterone, also called hypogonadism.
While the decline is gradual, some men notice changes earlier. Symptoms may include reduced energy, muscle weakness, or mood changes. Clinical trials have found that by age 70, most men will have testosterone levels far lower than in their younger years, which can impact overall health and vitality.
Age-Related Testosterone Changes in Women
Although testosterone is often linked to men, women also produce this hormone, though in smaller amounts. Testosterone supports bone health, muscle strength, and sexual well-being in women. As women age, particularly during and after menopause, testosterone levels decline. Below is a table that shows average testosterone levels at different stages of life in women.
| Age Group | Average Total Testosterone (ng/dL) | Key Changes |
| 20-29 years | 15–70 | Peak reproductive years |
| 30-39 years | 13–65 | Gradual decrease starts |
| 40-49 years | 10–60 | Noticeable decline |
| 50-59 years | 7–53 | Menopause, faster drop |
| 60+ years | 6–45 | Post menopause, lowest |
Symptoms of Low Testosterone at Different Ages
Recognizing low testosterone can be difficult because many symptoms resemble typical aging. Still, certain signs at each stage of life can suggest a hormonal imbalance that should not be ignored. Here is what to watch for at different ages:
- In Men (30s-40s): Men may begin to notice ongoing fatigue even after a full night’s sleep, difficulty building or maintaining muscle, and a gradual decline in sexual interest or performance. These changes may be subtle but can affect daily life and well-being.
- In Men (50s-60s): Symptoms can become more pronounced with age. Erectile dysfunction becomes more common, along with a loss of motivation and drive. Many men also experience increased abdominal fat, even if their lifestyle has not changed. These issues may be mistaken for other health concerns but often relate to testosterone decline.
- In Women (Post-menopause): Women may experience mood swings, irritability, and decreased bone density, making them more prone to fractures. A noticeable reduction in sexual interest is also common. These symptoms can impact self-esteem and daily comfort.
- In Both: Both men and women may have trouble focusing, poor sleep quality, and a decrease in overall physical strength. If these issues persist, it is important to seek medical evaluation, as addressing low testosterone can improve quality of life.
Factors Accelerating Testosterone Decline
Some lifestyle and health factors can speed up the natural decline of testosterone as we age. Paying attention to these can help maintain healthier levels for longer.
- Chronic illnesses such as diabetes or obesity: These conditions can disrupt hormone levels and increase inflammation, worsening overall health.
- High stress levels and poor sleep: Both can negatively affect hormone production and immune function, leading to increased disease risk.
- Use of certain medications, including steroids: Some drugs alter hormone balance or increase the risk of side effects like fluid retention or blood clots.
- Excess alcohol use and smoking: These habits damage organs, impair hormone regulation, and elevate cardiovascular and metabolic risks.
- Lack of regular physical activity: Insufficient exercise contributes to obesity, poor circulation, and worsened metabolic and hormonal health.
Measuring Testosterone Levels by Age Group
Doctors measure testosterone using blood tests, often taken in the morning when levels are highest. Here is an overview of typical ranges:
| Age Group | Average Testosterone in Men (ng/dL) | Clinical Reference Range |
| 20-29 years | 280–1100 | 300–1000 |
| 30-39 years | 220–980 | 270–950 |
| 40-49 years | 200–900 | 250–900 |
| 50-59 years | 170–820 | 200–850 |
| 60+ years | 130–700 | 170–720 |
Levels below the lower end of the range may suggest low testosterone and prompt further evaluation.
Effects of Low Testosterone on Health
Low testosterone can affect many areas of health. Here are some of the key impacts:
- Muscle Loss: Reduced muscle mass and strength, leading to decreased mobility
- Bone Density: Higher risk of osteoporosis and fractures
- Heart Health: Increased risk of cardiovascular problems, including heart disease
- Mood Changes: Higher rates of depression, irritability, and anxiet
- Cognitive Decline: Difficulty with memory, focus, and decision-making
- Fatigue: Persistent tiredness that does not improve with rest
- Sexual Health: Lower libido, erectile dysfunction in men, and reduced arousal in women.
- Body Composition: Increase in body fat, particularly around the abdomen
Managing Age-Related Testosterone Decline
There are several steps older adults can take to manage the effects of declining testosterone. Early recognition and a tailored plan can improve quality of life.
- Schedule regular health check-ups and hormone tests
- Address underlying conditions like obesity, diabetes, or sleep apnea
- Maintain a balanced diet rich in lean protein, healthy fats, and vegetables
- Engage in resistance training and regular physical activity
- Manage stress through relaxation techniques and mindfulness
- Discuss symptoms openly with healthcare providers for individualized advice.
Medical Interventions for Age-Related Decline
For some, medical treatment may be recommended. This is typically decided after thorough evaluation and consideration of symptoms and lab results.
- Testosterone Replacement Therapy (TRT): Delivered by injection, gel, patch, or pellet under medical supervision
- Medications: Some drugs can boost the body’s own production or address specific symptoms
- Treatment of Underlying Diseases: Managing diabetes or thyroid problems can improve testosterone levels
- Monitoring: Ongoing blood tests to ensure safety and effectiveness
Recent clinical trials, including those reviewed in the New England Journal of Medicine, show that TRT can improve energy and mood in select older adults, but is not suitable for everyone.
Natural Ways to Support Healthy Testosterone as You Age
Supporting hormone health naturally can make a big difference. Here are evidence-backed ways to help maintain healthy testosterone levels:
- Regular Exercise: Engaging in strength training a few times a week helps stimulate testosterone production and supports muscle and bone health, making it especially beneficial for older adults aiming to maintain healthy hormone levels and physical strength.
- Healthy Weight: Maintaining a healthy body weight reduces the risk of hormone imbalances, as excess body fat can convert testosterone to estrogen and accelerate decline, which is especially important with age.
- Balanced Nutrition: Eating foods rich in zinc, vitamin D, and omega-3 fatty acids supports hormone production and balance. These nutrients are linked to healthier testosterone levels and should be included in daily meals.
- Good Sleep: Getting 7–8 hours of restful sleep each night helps the body regulate hormones. Poor sleep lowers testosterone, so keeping a regular sleep schedule is important for supporting healthy aging.
- Limit Alcohol: Excessive alcohol intake can lower testosterone levels and harm overall health. Moderate drinking or abstaining altogether is best for hormone balance and long-term wellness.
- Reduce Stress: Chronic stress raises cortisol, a hormone that suppresses testosterone production. Managing stress through relaxation, meditation, or enjoyable activities helps maintain healthy hormone levels as you age.
- Quit Smoking: Smoking is associated with faster testosterone decline and other health risks. Quitting can help protect your hormones and improve overall well-being, especially in later life.
- Stay Socially Engaged: Regular social interaction boosts mental and emotional health and supports hormonal balance. Staying connected with family, friends, or community can have a positive impact on aging.
- Herbal Supplements: Certain herbs like ashwagandha and fenugreek may help support testosterone, but they should only be used after consulting your doctor to avoid interactions and ensure safety.
Risks of Testosterone Supplementation in Older Adults
While testosterone therapy may help some, it is not without risks. Understanding potential side effects is important before starting any treatment.
- Increased risk of blood clots and stroke: Testosterone can increase the likelihood of forming harmful blood clots, which may travel to the brain and cause a stroke.
- Possible worsening of existing prostate issues: Testosterone might exacerbate benign prostatic hyperplasia or contribute to prostate cancer growth.
- Fluid retention, which can worsen heart failure: Retained fluid increases blood volume and pressure, putting additional strain on an already weakened heart.
- Sleep apnea can become worse: Testosterone may worsen obstructive sleep apnea by relaxing airway muscles during sleep.
- Higher red blood cell count, increasing heart risks: Elevated hematocrit thickens the blood, increasing the risk of cardiovascular complications.
- Acne and skin changes: Hormonal effects can stimulate oil glands, resulting in acne or other skin alterations.
- Breast enlargement in men: Hormone imbalances may cause gynecomastia, or male breast tissue growth.
- Fertility reduction: Testosterone therapy can decrease sperm production, impairing fertility.
Prevention and Early Detection
Preventing low testosterone and detecting issues early can lead to better long-term health outcomes. Here’s what you can do:
- Get regular check-ups with your healthcare provider
- Ask for hormone testing if you notice symptoms like fatigue or mood changes
- Maintain a healthy lifestyle with exercise and balanced nutrition
- Address chronic diseases early, such as diabetes and hypertension
- Avoid unnecessary use of steroids or hormone supplements
- Learn your family history, as genetics can play a role
- Stay informed about the signs and risk factors
Conclusion
Testosterone levels naturally decline as part of the aging process for both men and women. This change can bring a variety of symptoms, including low energy, mood shifts, and reduced muscle or bone strength, which may affect daily life and independence. Recognizing these changes early allows you to take steps to support your health and well-being. Regular medical check-ups, an active lifestyle, balanced nutrition, and good sleep habits are crucial for maintaining healthy hormone levels as you get older.
It’s important to stay informed about potential risks and treatment options, including when to seek help from a healthcare provider. With the right knowledge and proactive care, most adults can manage the effects of age-related testosterone decline and maintain a good quality of life. Remember, a healthy approach to aging involves both prevention and early detection.
Frequently Asked Questions
1. At what age does testosterone start to decline in men?
Testosterone usually begins to decline around age 30, dropping by about 1% each year. The process is gradual and often goes unnoticed at first.
2. Can women experience symptoms from low testosterone?
Yes, women can have symptoms such as reduced energy, low mood, and decreased sexual desire, especially after menopause as hormone levels drop further.
3. What are normal testosterone levels for older adults?
Normal levels vary, but in men over 60, typical ranges are between 130 and 700 ng/dL. Values below this range may suggest low testosterone.
4. Is testosterone therapy safe for seniors?
Testosterone therapy can be safe for some, but carries risks like blood clots and heart issues. It requires careful monitoring by a healthcare provider.
5. Can lifestyle changes help maintain testosterone levels?
Yes, regular exercise, healthy diet, good sleep, and managing stress can help maintain healthier testosterone levels as you age.
6. Are there natural supplements for boosting testosterone?
Some supplements like ashwagandha and fenugreek may support healthy testosterone, but always consult a doctor before starting any supplement.
7. What are common symptoms of low testosterone in men?
Common symptoms include fatigue, loss of muscle strength, low sex drive, mood changes, and increased body fat.
8. How is testosterone tested?
Testosterone is measured with a simple blood test, usually done in the morning when hormone levels are highest.
9. Can chronic illness affect testosterone levels?
Yes, illnesses such as diabetes, obesity, and chronic stress can speed up the decline of testosterone levels.
10. What should I do if I think I have low testosterone?
See your healthcare provider for a proper evaluation, including blood tests and a discussion about your symptoms and possible treatment options.
Reference
- The Journal of Clinical Endocrinology & Metabolism (JCEM)
- The New England Journal of Medicine (NEJM)
- Endocrine Society NCBI
- Menopause Review (Przegląd Menopauzalny)
- Hormones and Behavior (journal)
Dr. Ethan Ward, MD, is a board-certified urologist with over 12 years of clinical experience specializing in men’s health, hormone optimization, and sexual wellness. He earned his MD from Johns Hopkins University School of Medicine and completed his urology residency at Cleveland Clinic. Dr. Ward focuses on testosterone therapy, erectile function, and metabolic contributors to hormonal imbalance. His work includes peer-reviewed research on andropause management and patient-centered approaches to male vitality.