Healthy joints are essential for free movement, flexibility, and stability throughout life. They connect bones, absorb shock, and support daily motion. Protecting joint health prevents pain, stiffness, and mobility loss, ensuring long-term independence and an active lifestyle.
Key Takeaways
- Joints are categorized as fibrous (immovable), cartilaginous (slightly movable), and synovial (freely movable).
- Core functions include movement, stability, weight-bearing, and cushioning of bones.
- Aging, obesity, genetics, inactivity, and poor nutrition negatively impact joint health.
- Common disorders include osteoarthritis, rheumatoid arthritis, gout, and bursitis.
- Prevention involves healthy weight, low-impact exercise, proper posture, hydration, and an anti-inflammatory diet.
- Treatment options range from medication and physiotherapy to joint injections and surgical interventions.
- Emerging trends like regenerative medicine, PRP, and advanced implants show promise for future joint repair and recovery.
Introduction to Joint Health
Healthy joints help you stay active and independent throughout your life. They allow your body to move freely and support daily activities.
- Joints are the connections between bones that give your body flexibility and stability.
Good joint health supports mobility, reduces pain risk, and protects against disability. - Problems with joints are a leading cause of pain and limited movement, especially as people age.
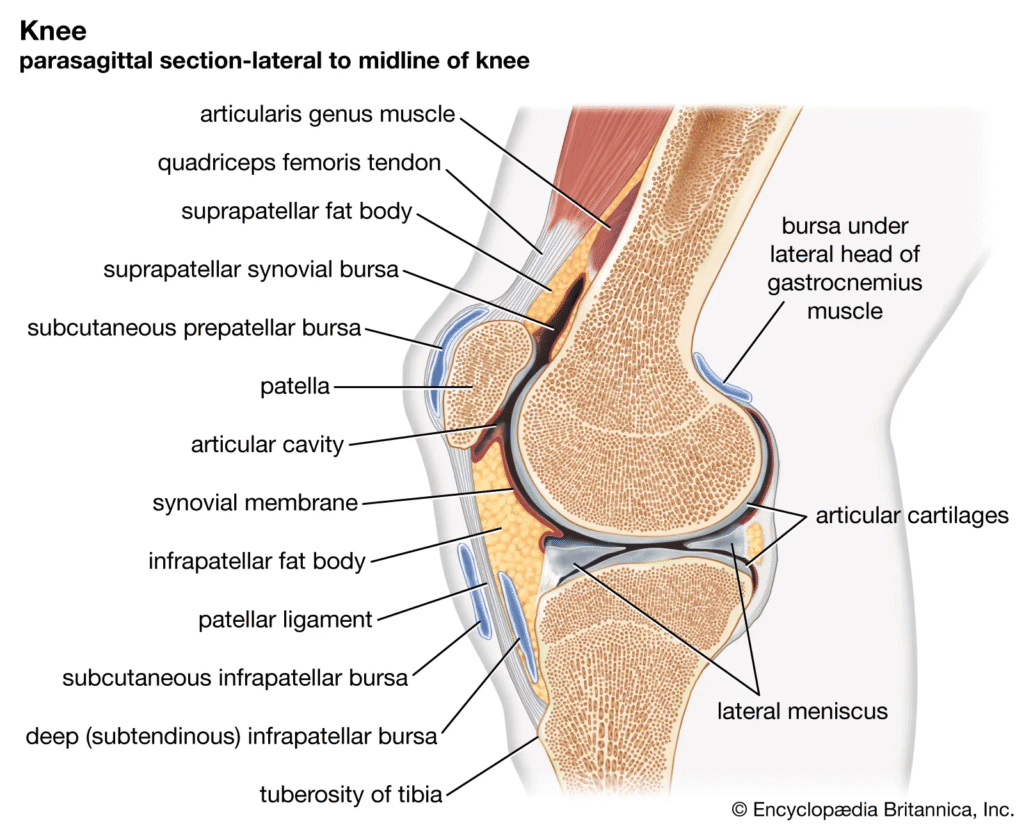
Anatomy of Joints
A joint is the point where two or more bones meet in the body, allowing for movement and providing structural support. There are three main types of joints based on their structure: fibrous joints (immovable), cartilaginous joints (slightly movable), and synovial joints (freely movable).
- Fibrous joints: Bones are joined by dense fibrous connective tissue; these joints are usually immovable, like the sutures in the skull.
- Cartilaginous joints: Bones are connected by cartilage, allowing limited movement; examples include the joints between vertebrae.
- Synovial joints: Most common and movable joint type, characterized by a joint cavity containing synovial fluid for lubrication; examples are the knee, shoulder, and hip.
Key Functions of Joints
The key functions of joints are to enable movement, provide structural support and stability, bear weight, cushion and protect bones, and maintain posture and flexibility in the skeleton.
- Enable Movement: Joints allow bones to move relative to one another, making walking, running, bending, and other motions possible.
- Provide Structural Support and Stability: Joints help stabilize parts of the skeleton, like the skull and pelvis, protecting vital organs and supporting the body’s weight.
- Bear Weight: Many joints, especially those in the legs and spine, are designed to support the body’s weight during standing and movement.
- Cushion and Protect Bones: Synovial joints include cartilage and fluid that reduce friction, cushion bone ends, and absorb shock during movement.
- Maintain Posture and Flexibility: Joints help maintain body posture, balance, and allow for flexibility in activities and sports.
Factors Influencing Joint Health
Several factors influence how well your joints function and how long they stay healthy.
- Age and genetics: Joint problems often become more common with age, and family history can play a role
- Body weight: Extra weight puts added pressure on weight-bearing joints, like knees and hips
- Physical activity: Regular movement strengthens muscles around joints but too much or too little can be harmful
- Nutrition and hydration: Proper nutrients and enough water keep joints lubricated and strong
- Hormonal changes: Hormones, especially in women during menopause, can affect joint health
Common Joint Disorders and Diseases
Common joint disorders and diseases include osteoarthritis, rheumatoid arthritis, gout, bursitis, and ankylosing spondylitis. Less common but important conditions are infectious arthritis, psoriatic arthritis, systemic diseases like lupus, and joint problems from trauma or overuse.
- Osteoarthritis: The most common joint disorder, caused by the gradual breakdown of cartilage, leading to pain, stiffness, and swelling.
- Rheumatoid arthritis: An autoimmune disease where the immune system attacks the joint lining, causing inflammation, pain, swelling, and eventual joint deformity.
- Gout: Characterized by sudden, severe attacks of pain and swelling, often in the big toe, due to uric acid crystal buildup in the joint.
- Bursitis: Inflammation of bursae (fluid-filled sacs) that cushion joints, commonly resulting from overuse or trauma, causing pain and swelling.
- Ankylosing spondylitis: A type of inflammatory arthritis primarily affecting the spine and sacroiliac joints, leading to stiffness and reduced mobility.
- Psoriatic arthritis: An inflammatory joint condition occurring in people with psoriasis, affecting peripheral joints and sometimes causing significant bone damage.
- Infectious arthritis: Caused by bacterial, viral, or fungal infections, leading to rapid joint damage if untreated.
- Lupus and other systemic diseases: Autoimmune conditions, such as lupus and scleroderma, often affect multiple joints, sometimes in combination with skin or organ problems.
Early Signs and Symptoms of Joint Problems

Recognizing symptoms early helps prevent long-term joint damage. Even mild discomfort can signal the start of a problem.
- Persistent Joint Pain: Pain lasting weeks, often worsening with movement or after rest, can indicate arthritis or joint damage. It may feel like a dull ache or burning sensation.
- Joint Stiffness: Especially noticeable after inactivity or in the morning, stiffness may limit joint movement and flexibility. In rheumatoid arthritis, morning stiffness can last over 45 minutes.
- Swelling and Warmth: Inflammation can cause the joint to swell, feel warm, tender, or look red. This often signals underlying joint inflammation or infection.
- Limited Range of Motion: Difficulty fully bending or moving the joint can occur early, often accompanied by the sensation of the joint being “stuck”.
- Clicking, Popping, or Grinding Noises: These joint sounds, especially if frequent or painful, may suggest cartilage wear or mechanical joint problems.
- Weakness or Instability: A feeling that the joint might give out implies ligament or tendon issues affecting joint stability.
- Other Symptoms: Depending on the cause, additional signs might include redness, tenderness, or systemic symptoms like fatigue and fever in autoimmune conditions like rheumatoid arthritis.
Diagnosing Joint Issues
Diagnosing joint issues involves a combination of clinical evaluation, laboratory testing, and imaging studies.
Clinical Examination
Doctors begin with a physical exam to check for joint swelling, redness, warmth, tenderness, deformity, and range of motion. They may also assess joint stability and listen for joint sounds like clicking or grinding. Comparing affected joints with unaffected ones helps detect abnormalities.
Imaging Tests
The initial imaging test for evaluating joint disorders is typically radiography (X-rays). X-rays are preferred first because they are widely available, low cost, and provide a clear view of bone structure, including joint space narrowing, bone spurs (osteophytes), and other bony abnormalities relevant in many joint diseases like osteoarthritis.
If X-rays are inconclusive or more detailed evaluation is needed, especially for detecting early or subtle joint problems, other imaging modalities are used:
- MRI (Magnetic Resonance Imaging): Offers detailed images of soft tissues such as cartilage, ligaments, and tendons, and can detect early signs of joint inflammation, cartilage degeneration, and bone marrow edema. MRI is especially useful for early diagnosis in conditions like osteoarthritis and rheumatoid arthritis.
- Ultrasound: Used to evaluate soft tissues around joints, detect synovial inflammation, cysts, and guide joint fluid aspiration. It is sensitive in identifying early inflammatory changes not visible on X-rays.
- CT (Computed Tomography) scans: Useful for detailed bone imaging, detecting small fractures, bone fragments, and periarticular calcifications. CT is considered when MRI is contraindicated or unavailable.
Laboratory Tests
Laboratory tests are crucial in diagnosing joint issues by detecting inflammation, autoimmune markers, infections, and other conditions affecting joints.
Key laboratory tests include:
- Blood Tests for Inflammation: Erythrocyte Sedimentation Rate (ESR) and C-Reactive Protein (CRP) measure inflammation levels but are nonspecific markers to indicate the presence of inflammatory processes in the body.
- Autoimmune Markers: Tests such as Rheumatoid Factor (RF) and Anti-Cyclic Citrullinated Peptide (anti-CCP) antibodies help diagnose rheumatoid arthritis. Antinuclear Antibodies (ANA) detect autoimmune diseases like systemic lupus erythematosus (SLE). Other disease-specific antibodies such as anti-dsDNA, anti-Sm, anti-Ro/SS-A, anti-La/SS-B may be tested for lupus, Sjogren’s syndrome, or scleroderma.
- Genetic Marker: HLA-B27 antigen is tested as it is associated with spondyloarthropathies such as ankylosing spondylitis.
- Joint Fluid Analysis (Arthrocentesis): Fluid withdrawn from the joint is examined for infection, crystals (gout or pseudogout), inflammation, and blood cells, aiding in differential diagnosis.
- Other Blood Tests: Complete Blood Count (CBC) to evaluate for infection or anemia, uric acid levels for gout, creatine kinase levels for muscle damage, and Lyme disease serology if tick-borne infection is suspected.
Preventive Strategies for Optimal Joint Health
Preventive strategies for maintaining optimal joint health focus on lifestyle habits, diet, exercise, and injury prevention to reduce joint stress, inflammation, and risk of diseases like arthritis. Key strategies include:
- Maintain a Healthy Weight: Excess weight increases stress on weight-bearing joints (knees, hips, spine), accelerating cartilage wear and risk of osteoarthritis. Even modest weight loss can significantly reduce joint load and disease risk.
- Engage in Regular Low-Impact Exercise: Activities like walking, cycling, swimming, and strength training improve joint flexibility, strengthen muscles supporting joints, and reduce stiffness without excessive joint stress.
- Adopt Proper Posture: Correct posture reduces unnecessary strain on spine and joints, preventing long-term damage. This includes sitting and standing with spine aligned, bending knees instead of waist when lifting, and engaging core muscles.
- Eat a Balanced, Anti-Inflammatory Diet: Diet rich in fruits, vegetables, whole grains, lean protein, calcium, vitamin D, omega-3 fatty acids (found in fish, flaxseeds), and antioxidants supports joint health and reduces inflammation. Avoid processed foods, excess sugar, and unhealthy fats that can exacerbate inflammation.
- Stay Hydrated: Adequate water intake helps maintain lubrication in joints and reduces stiffness.
- Protect Joints from Injury and Overuse: Use proper techniques during physical activity, wear protective gear for sports, avoid repetitive strain by taking breaks and diversifying joint use, and warm up adequately before exercise to prevent injury.
- Avoid Smoking and Limit Excessive Caffeine/Alcohol: Smoking reduces bone mass increasing fracture risk, and excess caffeine and alcohol can weaken bones and increase inflammation.
- Regular Medical Checkups: Routine visits to healthcare providers or orthopedic specialists help detect early joint issues, allowing timely intervention to prevent progression.
Nutrition and Supplements for Joint Health
Nutrition and supplements play a vital role in supporting joint health by reducing inflammation, maintaining cartilage integrity, and strengthening bones. Key nutritional components and supplements beneficial for optimal joint function include.
Nutrition for Joint Health
The starting point for nutrition supporting joint health involves focusing on key essential nutrients that help protect bones, maintain cartilage, reduce inflammation, and support overall joint function.
- Omega-3 Fatty Acids: Found in fatty fish (salmon, mackerel, sardines) and flaxseeds, omega-3s have strong anti-inflammatory properties that help reduce joint pain, swelling, and stiffness. Regular intake of omega-3-rich foods or supplements can improve symptoms of arthritis and support overall joint health.
- Antioxidants (Vitamins C and E): Vitamin C, abundant in fruits like berries and citrus, is critical for collagen production, which maintains cartilage strength and flexibility. Antioxidants fight oxidative stress that contributes to joint damage.
- Calcium and Vitamin D: Calcium is essential for bone density, while vitamin D enhances calcium absorption. Dairy products, fortified foods, leafy greens, eggs, and sunlight are good sources. Adequate levels help prevent bone loss and joint degeneration.
- Collagen: Collagen supports cartilage structure. Bone broth and collagen supplements can aid in reducing joint pain and improving mobility by maintaining connective tissue health.
- Anti-Inflammatory Foods: Incorporating fruits, vegetables (especially leafy greens and cruciferous vegetables), nuts, seeds, whole grains, olive oil, and herbs/spices like turmeric and ginger helps reduce inflammation and protect joints.
Popular Supplements for Joint Health
Popular supplements for joint health, supported by scientific evidence and commonly used to reduce joint pain, inflammation, and support cartilage and bone integrity, include the following.
- Glucosamine and Chondroitin: These compounds are components of cartilage and may help reduce joint pain and stiffness by supporting cartilage repair. Evidence is mixed, but some people experience relief with these supplements.
- Turmeric/Curcumin: Known for its anti-inflammatory effects, curcumin in turmeric can lessen joint pain and inflammation, particularly in osteoarthritis and rheumatoid arthritis.
- Fish Oil: Concentrated omega-3 supplements help reduce inflammation and improve joint symptoms.
- Collagen Peptides: Collagen supplements support the repair of ligaments, tendons, and cartilage.
- Rose Hip: Rich in vitamin C, it supports collagen formation and reduces inflammation.
- Other Natural Supplements: Boswellia (Indian frankincense), SAMe, green tea extract, and methylsulfonylmethane (MSM) have varying degrees of evidence for joint support.
Dietary and Lifestyle Tips for healthy joints
Here are important dietary and lifestyle tips to support optimal joint health.
- Follow an Anti-Inflammatory Diet: Emphasize whole, unprocessed foods such as fruits, vegetables, whole grains, nuts, seeds, olive oil, and fatty fish rich in omega-3 fatty acids. These foods help reduce inflammation and protect joint tissues.
- Maintain a Healthy Weight: Excess body weight puts extra stress on weight-bearing joints like knees and hips, accelerating wear and increasing risk of osteoarthritis. Even modest weight loss can significantly reduce joint load.
- Stay Hydrated: Drinking adequate water helps keep joints lubricated and reduces stiffness.
- Engage in Regular Low-Impact Exercise: Activities such as walking, swimming, cycling, and strength training improve joint flexibility, build supportive muscle strength, and reduce stiffness while avoiding excessive joint stress.
- Use Proper Posture and Body Mechanics: Good posture reduces unnecessary strain on joints, especially the spine. When lifting, bend knees instead of the waist and engage core muscles.
- Protect Joints from Injury: Use proper techniques during activities and sports, wear protective gear, and avoid repetitive strain by taking breaks and varying joint use.
- Avoid Smoking and Limit Excessive Caffeine or Alcohol: Smoking reduces bone density and healing capacity, while excess caffeine and alcohol can adversely affect bone and joint health.
- Consult Healthcare Providers for Supplements and Early Joint Concerns: Medical guidance ensures appropriate use of supplements like omega-3s, glucosamine, or turmeric, and timely intervention if joint symptoms arise.
Treatment Options for Joint Disorders
Treatment options for joint disorders vary depending on the specific condition, its severity, and the affected joint, but generally include a combination of medication, physical therapy, lifestyle modifications, injections, and surgery.
Medications
Medications are often the first line of treatment for joint disorders and are used to relieve pain, reduce inflammation, and address the underlying causes of joint problems.
- Pain relievers and anti-inflammatory drugs (NSAIDs): Commonly prescribed to reduce pain and inflammation (e.g., ibuprofen, naproxen).
- Acetaminophen: For mild to moderate joint pain.
- Disease-modifying antirheumatic drugs (DMARDs): Used in autoimmune joint diseases like rheumatoid arthritis to slow disease progression.
- Corticosteroids: Either oral or injected into the joint to reduce severe inflammation.
- Uric acid-lowering drugs: Used for gout management.
Physical therapy and lifestyle changes
Physical therapy and lifestyle modifications play a crucial role in managing joint disorders by improving joint function, increasing strength and flexibility, and reducing stress on affected joints.
- Exercises to improve joint flexibility, strengthen muscles supporting the joint, and reduce stiffness.
- Weight management to decrease stress on weight-bearing joints.
- Joint protection techniques and avoiding injury.
Joint injections
Joint injections are used to deliver medications directly into the affected joint, providing targeted relief from pain and inflammation and, in some cases, promoting healing.
- Corticosteroid injections: Provide temporary relief by reducing inflammation.
- Hyaluronic acid injections: Aim to lubricate the joint, especially in osteoarthritis, though evidence is mixed.
- Regenerative medicine approaches: Such as platelet-rich plasma (PRP) to promote healing.
Surgical options: Considered when conservative treatments
Surgical interventions are considered when conservative treatments are ineffective, and may include various procedures aimed at repairing, replacing, or stabilizing the affected joint.
- Arthroscopy: Minimally invasive surgery to repair or clean damaged joint tissues.
- Joint replacement surgery: Replacing damaged joints (hip, knee, shoulder) with artificial implants for severe degeneration.
- Joint fusion: Fusing bones to eliminate painful joint movement.
- Osteotomy: Bone realignment to redistribute weight away from damaged joint areas.
Lifestyle Modifications for Lifelong Joint Health
For lifelong joint health, key lifestyle modifications include maintaining a healthy weight, engaging in regular low-impact exercise, adopting proper posture, eating an anti-inflammatory balanced diet, protecting joints from injury, staying hydrated, and ensuring regular medical check-ups.
- Maintain a Healthy Weight: Excess weight increases stress on joints, especially weight-bearing ones like knees and hips, accelerating cartilage wear and risk of arthritis. Even a modest weight loss reduces joint load significantly.
- Regular Low-Impact Exercise: Activities such as walking, swimming, cycling, yoga, tai chi, and strength training enhance joint flexibility, strengthen muscles supporting joints, reduce stiffness, and improve balance without undue stress on joints.
- Proper Posture and Body Mechanics: Maintaining good posture while sitting, standing, and lifting reduces unnecessary joint strain. Ergonomic adjustments at work (chair, desk, screen setup) and correct lifting techniques (bend knees, not waist) distribute weight evenly and protect joints.
- Balanced Anti-Inflammatory Diet: A diet rich in fruits, vegetables, whole grains, nuts, lean proteins, omega-3 fatty acids, and antioxidants supports joint health by reducing inflammation and providing nutrients essential for cartilage and bone.
- Protect Joints from Injury and Overuse: Avoid repetitive joint strain by taking breaks, using bracing or compression if needed, wearing supportive footwear, and warming up before physical activity to prevent injury and chronic damage.
- Stay Hydrated: Adequate water intake maintains synovial fluid concentration, keeping joints lubricated and reducing stiffness.
- Regular Medical Checkups: Routine visits to healthcare providers or orthopedic specialists help detect early joint problems and prevent progression with timely interventions.
- Adequate Rest and Sleep: Listening to your body’s signals, taking breaks when needed, and ensuring quality sleep aids joint repair and reduces discomfort.
Advanced Therapies and Future Trends
Advanced therapies and future trends in joint health and treatment are rapidly evolving, leveraging breakthroughs in biologics, regenerative medicine, and advanced technologies to transform how joint disorders are managed.
Key advanced therapies currently gaining prominence include:
- Regenerative Medicine: This encompasses stem cell therapy and platelet-rich plasma (PRP) injections. Stem cell therapies aim to repair damaged joint tissues by differentiating into required cell types, showing promise especially in osteoarthritis and tendon injuries. PRP uses concentrated growth factors from the patient’s own blood to accelerate healing and reduce inflammation. These treatments offer less invasive alternatives to surgery, with the goal of restoring joint function and delaying or avoiding joint replacement.
- Orthobiologics: Beyond stem cells and PRP, emerging orthobiologic treatments include cell secretomes and extracellular vesicles (EVs), which may provide regenerative and anti-inflammatory effects without using living cells, enhancing safety and therapeutic potential.
- Targeted Molecular Therapies: Small molecule drugs and biologics targeting specific pathways involved in joint degeneration and inflammation are under development. Growth factors like recombinant human fibroblast growth factor-18 (rhFGF-18) and bone morphogenetic proteins are explored to promote cartilage repair. Gene therapies aim to modify gene expression to sustain joint health and combat disease progression.
- Nanotechnology and Drug Delivery Systems: Advanced delivery methods using nanoparticles and hydrogels are designed to deliver medications directly to joint tissues with controlled release, maximizing efficacy while minimizing side effects.
- Advanced Imaging and Personalized Medicine: Innovations in imaging and biomarker research are enabling more precise diagnosis and individualized treatment plans. Machine learning and genomics help classify patient subtypes to tailor therapies targeting their specific disease mechanisms.
- Surgical Innovations: Techniques such as robotic-assisted joint replacement, 3D-printed custom implants, and “smart” implants that can monitor joint health are improving surgical precision, outcomes, and recovery times. Minimally invasive procedures continue to advance, allowing faster rehabilitation.
- Assistive Technologies for Rehabilitation: Wearable sensors, robotic exoskeletons, and virtual reality programs enhance physical therapy by providing real-time feedback and personalized exercise regimens to optimize joint recovery and function.
Myths and Misconceptions About Joint Health
Common myths and misconceptions about joint health often lead to misunderstanding and may hinder effective prevention and treatment. Here are some key myths debunked by experts.
- Myth: Joint discomfort is an inevitable aspect of aging.
Fact: While joint stiffness may increase with age, it is not inevitable that one must suffer joint pain. Many cases of joint pain stem from treatable issues like inflammation, muscle weakness, or poor posture. With proper care, exercise, and nutrition, pain-free mobility is possible even in older adults. - Myth: All joint pain means arthritis.
Fact: Not all joint pain is arthritis. Other causes include injuries, tendonitis, bursitis, or inflammation of soft tissues around joints. - Myth: Only older people get arthritis.
Fact: Arthritis can affect people of all ages, including children (juvenile arthritis) and young adults. Early diagnosis is important regardless of age. - Myth: Cracking your joints causes arthritis.
Fact: The cracking sound is due to gas bubbles releasing in joint fluid and is not scientifically linked to arthritis. Excessive cracking can irritate tissues but does not cause arthritis. - Myth: Nightshade vegetables (like tomatoes, potatoes, eggplants) worsen arthritis.
Fact: There is no evidence that nightshade foods aggravate arthritis symptoms. In fact, anti-inflammatory foods are recommended for joint health. - Myth: Exercise worsens arthritis or joint pain.
Fact: Proper, low-impact exercise improves joint function, strengthens muscles supporting joints, and reduces stiffness. - Myth: Bone loss is always noticeable.
Fact: Bone loss (osteoporosis) is often silent until fractures occur; symptoms may not be felt, stressing the importance of preventive care and screening. - Myth: Weather changes cause arthritis flare-ups.
Fact: While weather can affect how pain is perceived, it does not cause or worsen arthritis itself. - Myth: Surgery is the only solution for joint problems.
Fact: Many joint issues can be managed effectively with medication, physical therapy, lifestyle changes, and injections. Surgery is usually a last resort.
Red Flags When to See a Doctor.
You should see a doctor promptly if any of the following red flags for joint problems in children are present.
- Persistent joint swelling or visibly swollen joints.
- Pain at night that wakes the child or does not improve with common pain relievers such as paracetamol or ibuprofen.
- Severe bone pain is often described as deep, throbbing pain pointing to the bone rather than the joint.
- Joint redness, warmth, and tenderness, which may indicate infection (e.g., septic arthritis) requiring urgent care.
- Inability or refusal to walk or bear weight on the affected leg/joint.
- Limping or changes in movement/motor skills that are new, persistent, or worsening.
- Symptoms of systemic illness: loss of appetite, fatigue, weight loss, pallor, swollen lymph nodes, fever, or unusual rashes.
- Morning stiffness or prolonged stiffness over 45 minutes, suggesting inflammatory arthritis.
- Unexplained bone lumps or tenderness.
- Pain or swelling that lasts for several weeks or worsens over time.
- History inconsistent with injury, or pain without clear trauma.
- Weakness or regression in motor milestones or function in children.
Conclusion
Joint health is essential for mobility, independence, and overall quality of life. Joints are where bones meet, allowing movement, providing support, and absorbing shock. There are three main joint types: immovable (fibrous), slightly movable (cartilaginous), and freely movable (synovial, like knees and shoulders). Healthy joints depend on age, genetics, weight, activity, nutrition, and hormones. Common joint problems include osteoarthritis, rheumatoid arthritis, gout, and injuries, with symptoms like pain, stiffness, swelling, and reduced mobility. Early diagnosis uses exams, imaging, and lab tests.
Treatment ranges from medication and physical therapy to injections and surgery, depending on severity and cause. Preventive strategies such as maintaining a healthy weight, regular low-impact exercise, balanced diet, hydration, and injury prevention are key for lifelong joint health. New therapies, like regenerative medicine, are emerging. Addressing myths and seeking timely care for red-flag symptoms helps ensure joint health and function for all ages.
FAQs
1. What are joints and why are they important?
Joints are the connections between bones, allowing movement, flexibility, and support for the body’s daily activities.
2. What causes joint pain?
Joint pain can result from arthritis, injuries, overuse, infections, autoimmune diseases, or age-related wear and tear.
3. How can I keep my joints healthy as I age?
Maintain a healthy weight, stay active with low-impact exercises, eat a balanced diet, practice good posture, stay hydrated, and avoid injuries.
4. Are supplements like glucosamine or turmeric helpful for joint health?
Some people find relief with these supplements, but evidence varies. Consult your doctor before starting any supplement.
5. When should I see a doctor for joint pain?
See a doctor if pain is persistent, severe, associated with swelling or redness, limits movement, or follows an injury.
6. Is exercise safe if I have joint problems?
Yes, gentle, low-impact activities like swimming, walking, or cycling can help strengthen joints and reduce stiffness.
7. Does cracking your knuckles cause arthritis?
No, research shows that cracking knuckles doesn’t cause arthritis, though it might irritate tissues if done excessively.
8. What foods are good for joint health?
Foods rich in omega-3 fatty acids, antioxidants, calcium, and vitamin D—like fish, nuts, leafy greens, fruits, and dairy support joint health.
9. Can children get joint problems?
Yes, children can develop joint issues from injuries, infections, or conditions like juvenile arthritis.
10. What are the warning signs of a serious joint problem?
Red flags include persistent swelling, redness, warmth, inability to move the joint, fever, or severe, unexplained pain.
Reference
- National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) – Educational resources and research updates on joints and related diseases
https://www.niams.nih.gov/health-topics/educational-resources/health-lesson-learning-about-joints - Arthritis Foundation – Support, education, advocacy, and resources for arthritis and joint health
https://www.arthritis.org - JointHealth™ Education – An online program to help people with arthritis learn about self-management
https://education.jointhealth.org - MedlinePlus – Joint Disorders – Trusted information on joint disorders, diagnosis, and treatment
https://medlineplus.gov/jointdisorders.html - WebMD – Tips and advice for keeping joints healthy and managing joint pain
https://www.webmd.com/rheumatoid-arthritis/ss/slideshow-keep-joints-healthy - CreakyJoints – Arthritis support group finder and patient community resources
https://creakyjoints.org/support/arthritis-support-groups/ - British Society for Rheumatology – Leading UK specialist society for rheumatology and joint conditions
https://www.rheumatology.org.uk - Healthline – Information on supplements and nutrition for joint health
https://www.healthline.com/health/joint-supplements - Orthopaedic Specialty Group – Tips and resources for maintaining joint health from orthopedic experts
https://osgpc.com/top-10-orthopaedic-tips-for-maintaining-joint-health-i-osg/ - Arthritis Consumer Experts – Curated and reliable arthritis educational links and resources
https://jointhealth.org/resources-links.cfm?locale=en-CA
Dr. Carlos Mendoza, MD, PhD, is a rheumatologist and clinical researcher with 15 years of experience in musculoskeletal health, joint preservation, and inflammation management. He earned his PhD in Immunology from University of Toronto and completed his medical residency at Mayo Clinic. Dr. Mendoza’s practice bridges traditional rheumatology with emerging nutraceutical and anti-inflammatory interventions. He has published extensively on cartilage repair and omega-3 supplementation for joint function.