Joint pain, or arthralgia, is discomfort, soreness, or stiffness in one or more joints caused by conditions like osteoarthritis, autoimmune diseases, gout, infections, or injuries. It may be short-term or chronic, requiring accurate diagnosis and tailored treatment for relief and mobility preservation.
Key Takeaways
- Common causes include osteoarthritis, rheumatoid arthritis, gout, infections, and overuse injuries.
- Diagnosis uses medical history, physical exams, imaging (X-ray/MRI), and lab tests (inflammatory or crystal markers).
- Treatment involves NSAIDs, corticosteroids, DMARDs, biologics, physical therapy, and surgery in severe cases.
- Lifestyle habits like weight control, low-impact exercise, and anti-inflammatory diets reduce pain and protect joints.
- Early medical evaluation prevents irreversible damage and maintains long-term joint function.
- Home measures: rest, heat/ice, posture correction support pain control and recovery.
What Is Joint Pain?
Joint pain, medically known as arthralgia, refers to discomfort, aches, or soreness in any joint of the body. It can occur due to various reasons such as injury, strain, inflammation, or infection. Unlike arthritis, which is a group of diseases characterized by joint inflammation and damage, joint pain is a symptom that may be temporary or chronic depending on the underlying cause.
Causes of Joint Pain
Joint pain can arise from different sources ranging from degenerative changes in cartilage to autoimmune reactions and infections. Each cause requires a distinct approach to treatment.
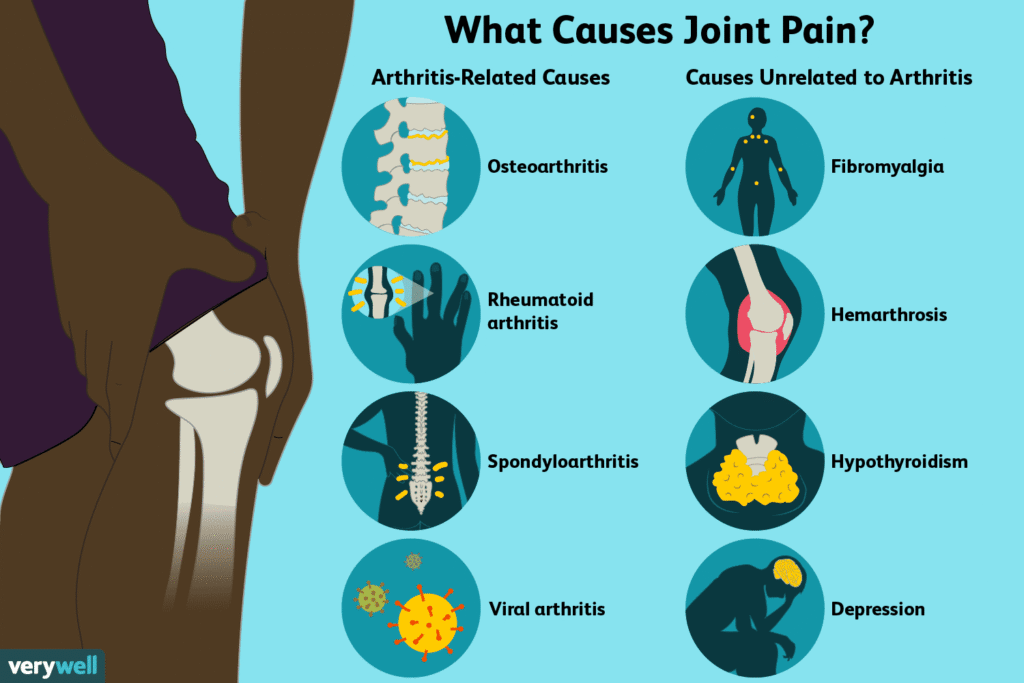
Degenerative Changes and Osteoarthritis
Osteoarthritis is the most common arthritis. It results from the gradual breakdown of cartilage, which cushions bones at joint surfaces. As cartilage wears down, bones rub against each other causing pain, swelling, stiffness, and loss of movement. Key risk factors are:
- Aging, which reduces cartilage repair ability
- Excess body weight, stressing weight-bearing joints
- Past joint injuries or repetitive stress from certain jobs or sports
- Family history affecting cartilage health
Autoimmune and Inflammatory Conditions
Some arthritis types occur when the immune system mistakenly attacks joint tissues, causing inflammation beyond the joint itself.
- Rheumatoid Arthritis (RA): The immune system targets the joint lining causing pain, swelling, stiffness, and symmetrical joint involvement such as both hands or knees. RA can also affect lungs, heart, and blood vessels. Women and smokers are at higher risk.
- Psoriatic Arthritis: Linked with the skin condition psoriasis, it causes joint and tendon inflammation including “sausage-like” swollen fingers or toes.
- Lupus Arthritis: Part of systemic lupus erythematosus, it causes joint pain alongside other systemic signs like fatigue and skin rash.
Crystal-Induced and Metabolic Arthropathies
Some types of joint pain occur when tiny crystals build up in the joint, irritating the tissues and triggering sudden, intense inflammation.
- Gout: Uric acid crystals deposit in the joints causing sudden, intense pain and swelling. It often affects the big toe. Triggers include high-purine foods (red meat, shellfish), alcohol, obesity, and genetics.
- Pseudogout: Calcium crystal deposits inflame joints presenting with symptoms similar to gout.
Infections and Post-Infectious Causes
Joint pain can sometimes be the result of an infection inside the joint or a reaction that develops after an infection elsewhere in the body.
- Septic Arthritis: A serious joint infection usually caused by bacteria, leading to severe pain, swelling, warmth, and fever. Immediate treatment is crucial to prevent joint damage.
- Lyme Disease: Tick-borne bacteria can cause joint inflammation and pain.
- Reactive Arthritis: Arthritis developing after infections elsewhere in the body such as urinary or gastrointestinal tracts.
Trauma, Overuse, and Mechanical Strain
Joint pain can result from:
- Acute injuries like sprains, strains, or fractures
- Overuse issues including tendonitis or bursitis
- Repetitive strain causing cartilage wear or ligament damage.
Diagnosis and Evaluation of Joint Pain
Accurate diagnosis is key to effective treatment. It involves:
- Clinical History and Physical Examination: Understanding pain location, duration, swelling, symmetry, stiffness duration, and other symptoms guides diagnosis.
- Imaging Tests: X-rays show bone and cartilage changes common in osteoarthritis. MRI and ultrasound better detect inflammation and soft tissue changes important in rheumatoid arthritis.
- Laboratory Tests: Blood tests include markers of inflammation like ESR and CRP, presence of autoimmune antibodies (rheumatoid factor, anti-CCP), uric acid levels for gout, and analysis of joint fluid to detect infection or crystals.
- Differential Diagnosis: Distinguishes osteoarthritis, rheumatoid arthritis, gout, infections, and other causes based on combined clinical, imaging, and lab findings.
Treatment Strategies for Joint Pain and Arthritis
Treatment depends on the cause but aims generally to relieve pain, improve function, and limit joint damage.
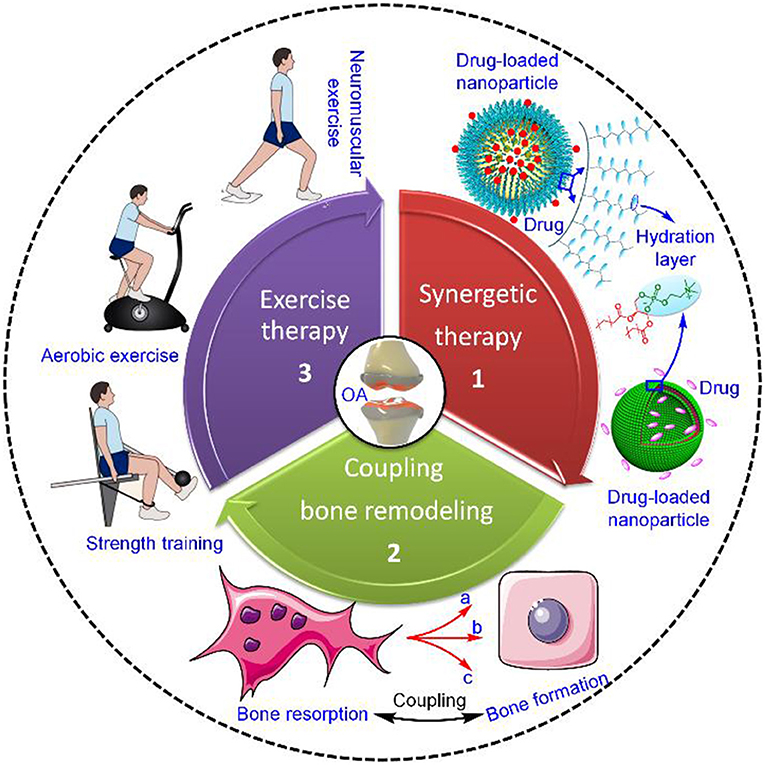
Conservative and At-Home Management
Simple steps can significantly ease symptoms and improve joint health:
- Rest painful joints but avoid prolonged inactivity
- Apply ice for swelling or heat to loosen stiff joints
- Use over-the-counter pain relievers such as acetaminophen or NSAIDs
- Engage in physical therapy and low-impact exercises like walking, swimming, or cycling to strengthen muscles and improve mobility
- Manage body weight to reduce stress on joints
- Improve ergonomics at work and home and maintain good posture
Medical and Pharmacologic Interventions
Medications for joint pain and arthritis include:
- NSAIDs and corticosteroids to reduce inflammation and relieve pain
- Disease-modifying antirheumatic drugs (DMARDs) used in autoimmune arthritis like RA to slow immune attack and joint damage
- Biologic therapies target specific parts of the immune system for moderate to severe RA
- Emerging treatments such as gene therapy and delivery of cartilage regenerating factors are under research
- Supplements like omega-3 fatty acids may help reduce inflammation, while glucosamine and chondroitin have mixed evidence
Surgical and Advanced Procedures
Surgery may be necessary if other treatments fail or joints are severely damaged:
- Joint replacement surgery for hips, knees, or shoulders can relieve pain and restore movement. Implants typically last 10 to 15 years.
- Ablative surgeries, like nerve radiofrequency ablation, reduce pain by interrupting pain signals.
- Surgery decisions are made carefully considering risks and benefits.
Prevention and Lifestyle Strategies
Preventing joint pain and arthritis breakthrough or worsening involves:
- Maintaining optimal body weight to avoid excess joint loading
- Avoiding repetitive high-stress activities that accelerate joint damage
- Staying active with regular low-impact exercises such as walking, swimming, and cycling
- Eating an anti-inflammatory diet, such as Mediterranean style rich in fruits, vegetables, whole grains, and omega-3 fatty acids
- Seeking early treatment at the first signs of joint pain
- Practicing good posture, ergonomic adjustments, and simple joint movements or fidgeting to keep joints lubricated
Conclusion
Joint pain, or arthralgia, is discomfort in any joint and can be temporary or chronic. It arises from causes such as osteoarthritis, where cartilage wears down, autoimmune diseases like rheumatoid arthritis and lupus, crystal deposits as in gout or pseudogout, infections including septic arthritis and Lyme disease, or injuries and overuse. Diagnosis involves medical history, physical examination, imaging such as X-rays or MRI, and lab tests to detect inflammation, crystals, or infection.
Treatment depends on the cause and may include rest, ice or heat, over-the-counter pain relievers, physical therapy, prescription medications like NSAIDs, corticosteroids, DMARDs, biologics, or, in severe cases, surgery such as joint replacement. Prevention focuses on maintaining a healthy weight, staying active with low-impact exercise, eating an anti-inflammatory diet, avoiding repetitive strain, and seeking early medical advice. Timely care can relieve pain, protect joint function, and improve quality of life.
FAQs
1. What is joint pain and how is it different from arthritis?
Joint pain, also called arthralgia, refers to discomfort, soreness, or stiffness in one or more joints. Arthritis, on the other hand, is a group of diseases that cause inflammation, swelling, and sometimes permanent damage to the joints. Joint pain may be temporary or long-term, depending on the underlying cause.
2. What are the most common causes of joint pain?
The leading causes include osteoarthritis (wear and tear of cartilage), rheumatoid arthritis and lupus (autoimmune diseases), gout or pseudogout (crystal deposits), infections like Lyme disease or septic arthritis, and injuries such as sprains, strains, or overuse.
3. When should I see a doctor for joint pain?
You should seek medical advice if the pain is persistent, sudden, or severe, or if it’s accompanied by swelling, redness, warmth, fever, or an inability to move the joint normally. Early diagnosis prevents complications and permanent damage.
4. How is joint pain diagnosed?
Doctors use a combination of physical exams, medical history, imaging tests (X-rays, MRI, ultrasound), and lab tests (blood tests for inflammation, antibodies, uric acid levels, or joint fluid analysis) to identify the exact cause.
5. Can exercise help reduce joint pain?
Yes. Regular low-impact exercise like swimming, cycling, and walking strengthens muscles, reduces stiffness, and protects joint mobility. High-impact or repetitive activities may worsen symptoms, so exercise should be tailored with guidance from a physical therapist.
6. What lifestyle changes help prevent or manage joint pain?
Maintaining a healthy weight, staying physically active, eating an anti-inflammatory diet, practicing good posture, and avoiding repetitive stress on joints are all effective in protecting joint health.
7. What are the best foods for joint pain relief?
Diets rich in omega-3 fatty acids (fish, flaxseeds, walnuts), fruits, vegetables, whole grains, olive oil, and nuts can reduce inflammation. Limiting processed foods, sugary snacks, and red meats may also help.
8. Are there home remedies that work for joint pain?
Yes. Rest, applying ice to reduce swelling, heat to ease stiffness, gentle stretching, massage, and over-the-counter pain relievers like acetaminophen or NSAIDs can provide short-term relief.
9. What medications are used for joint pain?
Common options include NSAIDs, corticosteroids, disease-modifying antirheumatic drugs (DMARDs) for autoimmune arthritis, and biologics for more advanced cases. Supplements such as omega-3 fatty acids may support overall joint health, though results vary.
10. Can joint pain be caused by infections?
Yes. Conditions like septic arthritis, Lyme disease, or reactive arthritis can trigger joint inflammation. These infections require urgent medical attention to avoid serious complications.
11. Is joint pain always age-related?
No. While osteoarthritis is more common with age, younger people can also develop joint pain due to injuries, autoimmune conditions, obesity, or infections.
12. Is surgery the only option for severe joint pain?
Not always. Surgery, including joint replacement, is usually a last resort when medications, therapy, and lifestyle changes fail. Many people manage pain effectively without surgery.
Reference
- Cleveland Clinic – Arthritis Overview https://my.clevelandclinic.org/health/diseases/12061-arthritis
- CDC – Osteoarthritis Overview https://www.cdc.gov/arthritis/osteoarthritis/index.html CDC
- Mayo Clinic – Arthritis Diagnosis &Treatment https://www.mayoclinic.org/diseases-conditions/arthritis/diagnosis-treatment/drc-20350777 Mayo Clinic
- CDC – Physical Activity & Arthritis https://www.cdc.gov/arthritis/prevention/index.html CDC
Dr. Carlos Mendoza, MD, PhD, is a rheumatologist and clinical researcher with 15 years of experience in musculoskeletal health, joint preservation, and inflammation management. He earned his PhD in Immunology from University of Toronto and completed his medical residency at Mayo Clinic. Dr. Mendoza’s practice bridges traditional rheumatology with emerging nutraceutical and anti-inflammatory interventions. He has published extensively on cartilage repair and omega-3 supplementation for joint function.