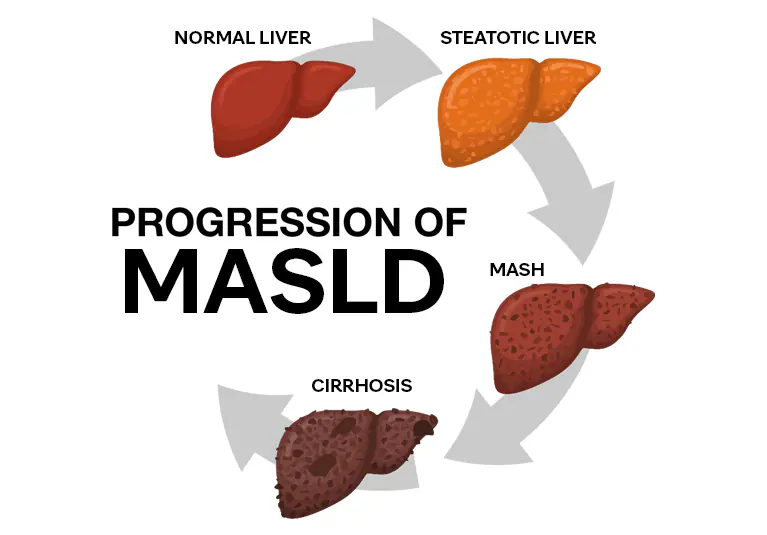
Metabolic dysfunction-Associated Steatotic Liver Disease (MASLD), formerly known as Non-Alcoholic Fatty Liver Disease (NAFLD), is a condition where excess fat accumulates in the liver due to metabolic dysfunction rather than alcohol use. It’s closely linked to obesity, diabetes, high cholesterol, and heart disease, reflecting broader metabolic imbalances in the body. Many people with MASLD show no symptoms and may have normal liver tests, making early detection crucial.
The disease spans a spectrum from simple fat buildup to inflammation, fibrosis, and even cirrhosis or liver cancer. While weight loss and lifestyle change remain the most effective treatments, new noninvasive diagnostic tools and emerging therapies like resmetirom and GLP-1 agonists offer hope for those with advanced disease. Early recognition and management not only protect the liver but also improve overall metabolic and cardiovascular health.
Key Takeaways
- MASLD is driven by metabolic problems, not alcohol.
- Many patients have normal liver enzyme levels despite disease.
- Fibrosis (scarring), not fat, predicts serious liver complications.
- Simple blood tests and scans can diagnose it without biopsy.
- Lifestyle change with weight loss remains the best treatment.
- New drugs like resmetirom offer targeted therapy for advanced cases.
What Is MASLD
MASLD (Metabolic Dysfunction-Associated Steatosis Liver Disease) is a condition where fat builds up in your liver mainly due to metabolic issues like obesity, diabetes, or high cholesterol. It often shows no symptoms at first but can harm the liver over time. Eating healthy, staying active, and managing blood sugar and cholesterol can prevent or even reverse it. See our detailed guide on Foods That Boost Liver Health to learn which nutrients best support liver recovery
The Scope of MASLD
The Scope of MASLD (Metabolic Dysfunction-Associated Steatotic Liver Disease) highlights how widespread the condition is and why it matters for public health and individual well-being. Its impact extends beyond the liver. Liver Cancer Prevention strategies often begin by addressing MASLD early.
Global Prevalence
- MASLD is one of the most common liver diseases worldwide.
- Estimates suggest that 25–30% of adults globally have MASLD, with higher rates in people with obesity or type 2 diabetes.
Who Is Affected
- Adults with metabolic risk factors: obesity, insulin resistance, high cholesterol, hypertension.
- Children and teens: Rising rates due to childhood obesity and poor diets.
- Older adults: Slower metabolism and multiple medications increase risk.
Health Impact
- Most cases are silent in the early stages.
- If untreated, MASLD can progress to:
- NASH (Non-alcoholic Steatohepatitis): liver inflammation and cell damage
- Fibrosis and cirrhosis: irreversible scarring
- Liver failure or liver cancer in advanced cases
- MASLD also increases risk of cardiovascular disease, diabetes complications, and kidney disease.
Economic and Social Burden
- The widespread prevalence leads to high healthcare costs due to screening, treatment, and complications.
- Impacts quality of life, productivity, and long-term health outcomes.
How Common Is It and Why It Matters
Prevalence is rising in parallel with obesity and diabetes. Up to 25–30 % of adults globally may have fatty liver changes. Many remain undiagnosed, raising long-term risks of cirrhosis, liver cancer, and cardiovascular disease. The health system burden is substantial due to overlapping metabolic complications.
What Happens in the Liver: The Underlying Mechanism
To understand how MASLD develops and progresses, it’s important to look inside the liver at the chain of biological events that transform simple fat accumulation into inflammation and scarring. The disease begins silently, often over years, as metabolic stress overwhelms the liver’s ability to process fats and toxins.
From Fat Storage to Injury
- Excess free fatty acids and triglycerides accumulate in liver cells (hepatocytes).
- Overload triggers oxidative stress and mitochondrial dysfunction.
- Cellular stress leads to inflammation, immune cell activation, and gradual fibrotic changes.
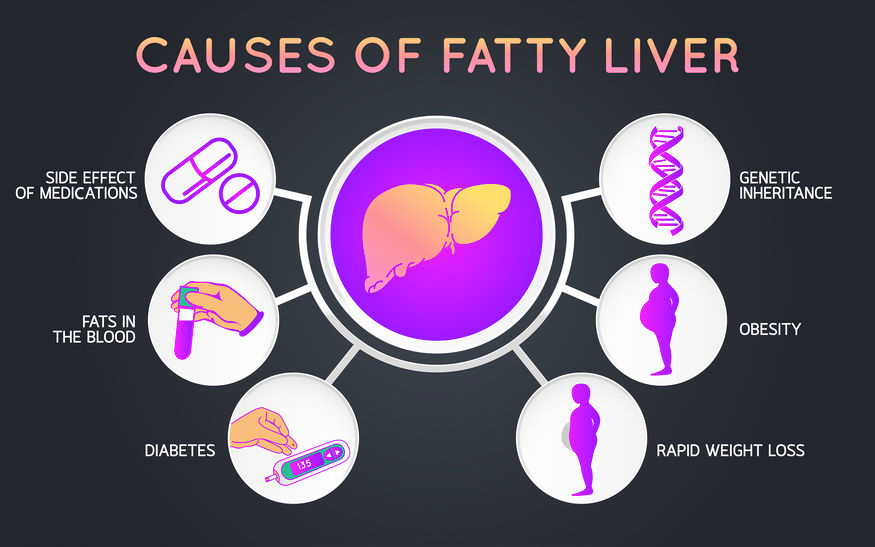
Drivers of the Process
- Insulin resistance: reduced ability to regulate glucose and fat metabolism.
- Adipose-liver cross-talk: inflamed fat tissue releases cytokines and free fatty acids.
- Genetic factors: PNPLA3 and TM6SF2 variants influence fat storage and fibrosis risk.
- Gut microbiome changes: leaky gut and endotoxins can aggravate liver inflammation.
Addressing Comorbidities
Managing MASLD effectively means treating the whole person, not just the liver. Since the disease is tightly linked to metabolic syndrome, cardiovascular issues, and diabetes, addressing these comorbidities is essential to prevent complications and improve long-term outcomes.
- Control blood pressure, cholesterol, and diabetes through medication and lifestyle changes
- Use GLP-1 or SGLT2 inhibitors when appropriate to improve both liver and metabolic health
- Vaccinate for hepatitis A and B to prevent additional liver injury
- Advise minimal alcohol use, as even small amounts can worsen liver inflammation and fibrosis
When Surgery Is an Option
In severe cases where lifestyle and medications fail, bariatric or metabolic surgery may be considered. Alongside this, a Liver-Friendly Lifestyle remains the cornerstone of ongoing recovery.
Bariatric/Metabolic Surgery
Surgical intervention is reserved for patients with severe obesity or obesity-related complications, offering long-term benefits beyond weight loss.
- Recommended for BMI ≥ 35 kg/m², or ≥ 30 kg/m² with comorbidities
- Improves liver steatosis and can partially reverse fibrosis in some patients
- Requires careful pre- and post-operative evaluation and follow-up to ensure safety and sustained benefits
Follow-Up and Monitoring
Regular follow-up is essential to track disease progression and detect complications early, especially since MASLD can remain silent for years. The frequency and intensity of monitoring depend on the stage of liver disease and individual risk factors. Consistent evaluation helps guide timely treatment adjustments and prevent irreversible damage.
- Non-cirrhotic: labs every 6–12 months, imaging every 2–5 years
- Cirrhotic: ultrasound ± AFP every 6 months, endoscopy as indicated
Action Plan for Patients
Living with MASLD requires a proactive, long-term approach focused on healthy habits and regular medical follow-up. Small, consistent lifestyle adjustments can make a major difference in reversing early liver changes and preventing complications. Patients should take an active role in their care and stay alert to warning signs of disease progression.
- Eat balanced meals and cut added sugar
- Exercise 30 min a day most days
- Sleep 7–8 hours, treat sleep apnea
- Track labs regularly
- Seek help for swelling, jaundice, or fatigue
Clinician Quick Reference
A structured and consistent approach helps clinicians quickly identify, assess, and manage MASLD in everyday practice. Early recognition and intervention can prevent progression to advanced fibrosis or cirrhosis. This simplified workflow ensures efficient risk stratification and timely referral when needed.
- Abnormal ALT or metabolic risk – calculate FIB-4
- Low risk – monitor; Indeterminate – elastography; High risk – refer
- Start lifestyle modification immediately
Common Myths vs Facts
Understanding MASLD can be confusing because many long-held beliefs are outdated. The table below clears common misconceptions.
| Myth | Fact |
| Normal ALT means no disease | Many patients with MASLD have normal enzymes, yet may have advanced fibrosis. |
| Statins harm the liver | Statins are safe and reduce heart risk in MASLD. |
| Biopsy is always needed | Noninvasive tools like FibroScan or MRI often replace biopsy. |
| Weight loss cures everything | Fat loss helps, but fibrosis may need longer management. |
| Only obese people get MASLD | Lean people with metabolic dysfunction can have MASLD. |
| MASLD rarely causes serious issues | It can progress to cirrhosis, cancer, and heart disease. |
Conclusion
Metabolic dysfunction-Associated Steatotic Liver Disease (MASLD), formerly NAFLD, is a major lifestyle-related liver condition with serious systemic effects. Early detection using simple blood tests and imaging can stop progression before cirrhosis or cancer develops. Most cases improve with weight loss, healthy eating, and regular exercise, while new drugs like resmetirom offer additional options for advanced disease. Awareness, prevention, and regular medical follow-up are key to safeguarding liver and heart health.
Frequently Asked Questions
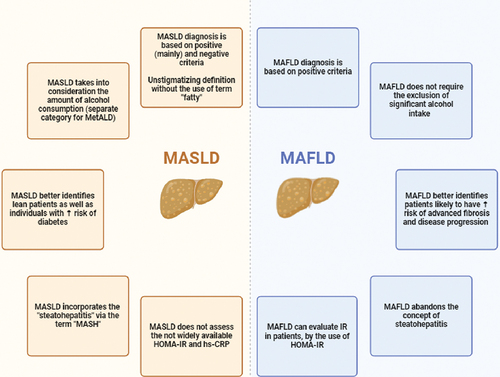
Is MASLD just a new name for NAFLD, and does it change anything clinically?
Yes, MASLD is the new name for NAFLD, emphasizing metabolic dysfunction as the primary cause. Treatment remains the same, focusing on lifestyle changes and managing underlying metabolic conditions like diabetes and obesity.
What FIB-4 cutoffs are used, and when should I order elastography?
Use 1.3 (under 65) or 2.0 (over 65) for low risk, and 2.67 for high risk requiring referral. Order elastography for intermediate scores to better assess fibrosis risk.
Can ultrasound detect MASLD or fibrosis?
Ultrasound detects moderate to severe fat but cannot assess fibrosis reliably. Elastography and specialized MRI provide more accurate evaluation of both fat content and fibrosis staging.
How much weight loss helps?
5% weight loss improves liver fat, while 7 to 10% or more significantly reduces inflammation and fibrosis. Sustained weight reduction through lifestyle changes shows the greatest liver benefit.
Do GLP-1 drugs treat MASLD?
GLP-1 agonists like semaglutide reduce liver fat and improve metabolic health but aren’t yet FDA-approved specifically for MASLD. They’re still under clinical evaluation for direct liver disease treatment.
Who qualifies for resmetirom, and how is it monitored?
Adults with non-cirrhotic MASH and F2-F3 fibrosis qualify for resmetirom. Regular monitoring includes thyroid function, liver enzymes, and lipids due to its thyroid receptor mechanism.
Are statins safe?
Yes, statins are safe and recommended for cardiovascular risk management in MASLD patients. They rarely cause liver harm and the cardiovascular benefits outweigh minimal hepatotoxicity risk.
When is a biopsy still required?
Biopsy is needed when noninvasive tests conflict, precise staging is essential for treatment decisions, or when evaluating for concurrent liver diseases. It’s also required before certain drug therapies.
How often should non-cirrhotic patients be followed up?
Follow non-cirrhotic patients every 6 to 12 months with labs and metabolic assessment. Increase frequency if disease progresses or metabolic control worsens.
What additional checks are needed after cirrhosis?
Cirrhotic patients need ultrasound ± AFP every 6 months for cancer screening and upper endoscopy every 1 to 3 years for varices. Regular monitoring for decompensation signs is also essential.
Dr. Amiah Rainey researches diet–disease relationships with expertise in vitamins, minerals, and biomarker methods. She earned a PhD from Harvard T.H. Chan School of Public Health (2019) and completed a postdoctoral fellowship at the NIH/NIDDK. With ~20 peer-reviewed publications (example) and experience on NIH-funded cohort studies, Amiah translates complex evidence into practical guidance. She advises on study design, evidence grading, and data transparency. Profiles: ORCID, Google Scholar; list affiliations and any disclosures.

