Oral health is essential for overall well-being, enabling vital functions like chewing, speaking, and smiling while preventing infections and systemic diseases. It involves healthy teeth, gums, and oral tissues maintained through daily hygiene, balanced nutrition, and regular dental care. Modern dentistry combines prevention, restoration, and digital technology to preserve lifelong oral wellness across all age groups.
Key Takeaways
- Oral health prevents tooth decay, gum disease, and oral cancer.
- Key structures: teeth, gums, saliva, and oral microbiome maintain balance.
- Core practices: brushing twice daily, flossing, tongue cleaning, and fluoride use.
- Nutrition rich in calcium, vitamins C and D supports strong teeth and gums.
- Risk factors: poor hygiene, sugar intake, smoking, alcohol, and dry mouth.
- Professional dental visits enable cleaning, early detection, and oral cancer screening.
- Advanced care includes fillings, crowns, implants, laser, and digital dentistry innovations.
Understanding about Oral Health
Oral health is the state of being free from mouth and facial pain, oral infections, gum disease, tooth decay, and other diseases that limit an individual’s ability to bite, chew, smile, and speak. Beyond aesthetics, it plays a vital role in nutrition and social interaction. Poor oral health can result in chronic pain, tooth loss, and impact self-esteem and communication abilities.
Anatomy and Physiology of the Oral Cavity
The mouth is a complex system composed of multiple structures working together for oral functions and protection.

Teeth Structure and Function
Teeth are specialized structures designed to perform specific functions essential for chewing, speaking, and maintaining overall oral health. Their unique shapes and internal composition enable them to efficiently break down food while protecting the sensitive inner tissues from damage.
- Types: incisors, canines, premolars, molars
- Layers: enamel (strongest substance), dentin (protects pulp), pulp (nerve and blood supply)
- Tooth eruption stages: primary (baby teeth) and permanent teeth timeline
Gums and Supporting Tissue
The gums and supporting tissues form the foundation that holds teeth securely in place, protecting them from harmful bacteria and mechanical forces while maintaining overall oral stability and health.
- Gingiva: protective tissue around teeth
- Periodontal ligament: anchors teeth in jawbone
- Alveolar bone: supports teeth roots
Saliva and its Role
Saliva is a vital fluid produced continuously by the salivary glands, playing a key role in maintaining oral health and supporting digestion.
- Lubrication and digestion aid
- Antimicrobial properties
- Buffering acids to protect enamel
Oral Microbiome
The oral microbiome is the complex community of microorganisms that naturally reside in the mouth, playing a crucial role in maintaining oral health and preventing disease.
- Composition of bacteria
- Balance between beneficial and harmful microbes
- Impact on oral and systemic health
Common Oral Diseases and Their Causes
Understanding common oral diseases and their causes is essential for effective prevention and early treatment. Awareness helps in recognizing symptoms early and seeking timely dental care, which can prevent complications and preserve oral health.
Dental Caries (Tooth Decay)
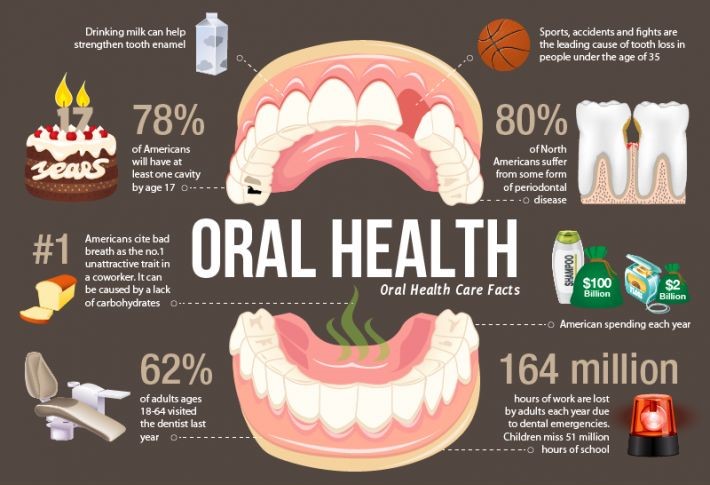
Dental caries, commonly known as tooth decay or cavities, is one of the most widespread oral diseases worldwide. It occurs when acid-producing bacteria in the mouth metabolize sugars from food and drinks, generating acids that gradually erode the tooth’s enamel, the hard protective outer layer.
The process begins with enamel demineralization, where acids dissolve minerals like calcium and phosphate from enamel. If this acid attack continues unmitigated without proper oral hygiene or fluoride protection, it leads to the formation of cavities holes in the tooth structure.
Risk factors for dental caries include:
- Poor oral hygiene that allows plaque buildup
- Frequent consumption of sugary or acidic foods and beverages
- Reduced saliva flow or dry mouth, which lowers natural protection
- Deep pits or grooves in teeth that trap food particles
- Certain medical conditions and medications that affect saliva
Periodontal Diseases
Periodontal diseases affect the gums and other structures supporting the teeth. They range from mild inflammation to severe tissue destruction.
- Gingivitis is the initial stage characterized by red, swollen, and bleeding gums caused by plaque-induced inflammation. It is reversible with thorough cleaning and improved oral hygiene.
- If untreated, gingivitis can progress to periodontitis, a more severe condition where the inflammation spreads deeper causing destruction of the connective tissue and bone that anchor the teeth. This leads to gum recession, tooth mobility, and eventually tooth loss.
Oral Cancer
Oral cancer is a serious condition most frequently found on the tongue, floor of the mouth, lips, and other oral surfaces. It often appears as persistent ulcers, lumps, or white/red patches that do not heal.
Risk factors include:
- Tobacco use (smoking or chewing)
- Excessive alcohol consumption
- Human papillomavirus (HPV) infection
- Prolonged sun exposure to the lips
Other Oral Conditions
Several additional conditions affect oral health:
- Aphthous ulcers (canker sores) are small, painful, shallow lesions inside the mouth. Though their exact cause is unknown, factors like stress, minor injuries, or immune responses are involved. They typically heal within 1-2 weeks without scarring.
- Oral thrush is a fungal infection caused by an overgrowth of Candida yeast, appearing as creamy white patches on the tongue or inner cheeks. It commonly affects individuals with weakened immunity, those using inhaled steroids, or after antibiotic use.
- Dental trauma refers to physical injuries to the teeth or surrounding tissues, often from accidents or sports injuries. It can cause tooth fracture, displacement, or loss.
- Dental erosion results from acid exposure not caused by bacteria but from external sources like acid reflux, frequent vomiting (eating disorders), or excessive acidic food and drink intake. It leads to enamel thinning and increased sensitivity.
Essential Daily Oral Hygiene Practices

Routine oral care is the cornerstone of preventing dental diseases and maintaining a fresh, healthy mouth. Consistently following proper Dental habits, cleaning helps control plaque, reduce harmful bacteria, and protect teeth and gums.
Tooth Brushing Best Practices
Effective tooth brushing involves more than just frequency; technique and tools matter significantly.
- Proper brushing technique and timing: Brush for at least two minutes twice daily, using gentle circular or short back-and-forth motions. Hold the toothbrush at a 45-degree angle to the gum line to clean both teeth and gums without causing damage.
- Choosing toothbrushes for different needs: Soft-bristled brushes are ideal for most people, especially those with sensitive gums. Special brushes are designed for people with braces or dental implants to reach difficult areas.
- Use of electric versus manual toothbrushes: Electric toothbrushes can offer better plaque removal, especially for those with limited manual dexterity. However, a well-used manual brush can also be effective.
Flossing and Interdental Cleaning
Cleaning between teeth is essential since toothbrushes cannot reach tight spaces adequately.
- Why flossing is critical: Flossing removes plaque and food particles between teeth, preventing cavities and gum disease.
- How to floss correctly: Use about 18 inches of floss, gently curve it against each tooth in a C shape, sliding beneath the gum line without snapping.
- Alternatives: Interdental brushes work well for people with wider gaps or braces, and water flossers are a good option for those seeking easier or more comfortable cleaning.
Tongue Cleaning
Bacteria and debris accumulate on the tongue’s surface, contributing to bad breath and plaque formation.
- Reducing bacteria that cause bad breath: Cleaning the tongue removes odor-causing microorganisms.
- Correct methods and tools: Use a tongue scraper or the bristles of a toothbrush to gently clean from the back toward the front of the tongue daily.
Mouthwash Use
Mouthwashes complement mechanical cleaning by reaching areas brushes and floss can’t.
- Cosmetic mouthwashes temporarily freshen breath.
- Antibacterial rinses reduce plaque and gum inflammation.
- Fluoride mouthwashes help strengthen enamel and prevent cavities.
- How to select appropriate mouthwash: Choose based on your oral health needs and consult a dentist if unsure.
- Limitations and potential side effects: Mouthwash is no substitute for brushing and flossing; some contain alcohol that may cause dryness or irritation.
Selecting Toothpaste
Toothpaste formulations are designed to address various oral health needs.
- Role of fluoride: Fluoride strengthens enamel and helps reverse early decay.
- Toothpaste formulations: Options include those for sensitive teeth, tartar control, whitening, or anti-cavity effects. Pick toothpaste suitable for your issues and preferences.
Managing Special Conditions
Certain conditions require adjusted oral hygiene practices.
- Braces and orthodontic care: Use special brushes and interdental cleaners to remove plaque around brackets and wires.
- Handling sensitive teeth: Use desensitizing toothpaste and avoid overly aggressive brushing.
- Tips for dry mouth sufferers: Sip water regularly, use saliva substitutes, avoid alcohol-containing mouthwashes, and maintain hydration to prevent decay and discomfort.
Nutrition and Lifestyle Factors Affecting Oral Health
What you eat and how you live play a crucial role in the health of your teeth and gums. Proper nutrition and healthy habits can strengthen oral tissues, while poor choices may contribute to disease.
Nutrients Supporting Oral Health
Certain vitamins and minerals are essential for maintaining strong teeth and healthy gums.
- Calcium and Vitamin D: Calcium is vital for building and maintaining strong tooth enamel and jawbone density. Vitamin D helps the body absorb calcium effectively, supporting bone and teeth strength.
- Vitamin C: This vitamin is critical for healthy gums as it supports collagen production, maintaining gum tissue integrity and accelerating healing.
- Antioxidants: Found in fruits and vegetables, antioxidants help combat inflammation and oxidative stress, reducing the risk of gum disease.
Foods to Avoid or Limit
Some foods and beverages increase the risk of tooth decay and enamel damage.
- Sugary snacks and beverages: Sugar fuels harmful bacteria that produce acids, leading to tooth decay. Frequent consumption of candies, sodas, and sweetened drinks raises cavity risk.
- Acidic foods: Citrus fruits, vinegars, and soft drinks can erode the enamel, making teeth more sensitive and prone to decay.
- Sticky foods: Items like dried fruits or caramel can cling to teeth longer, providing a breeding ground for bacteria.
Effects of Hydration and Saliva
Saliva is a natural defense against tooth decay and infection.
- Importance of water intake: Drinking adequate water helps wash away food particles and neutralizes acids, assisting saliva in protecting teeth.
- Factors that reduce saliva flow: Certain medications, dehydration, mouth breathing, and medical conditions can decrease saliva, increasing cavity and gum disease risk.
Tobacco and Alcohol Impact
Habits like smoking and drinking affect oral health deeply.
- How smoking harms gums and teeth: Tobacco use reduces blood flow to gums, impairing healing and encouraging bacterial growth. It also stains teeth and increases oral cancer risk.
- Alcohol’s drying effect and cancer risk: Alcohol dehydrates the mouth, lowering saliva production. Combined with tobacco, it significantly elevates the risk of oral cancers.
Stress and Hormonal Effects
Body stress and hormonal changes influence gum health.
- How stress worsens gum disease: Chronic stress weakens immune response, increasing inflammation and susceptibility to gum infection.
- Hormonal changes: Pregnancy, menstruation, and menopause cause gum sensitivity and swelling due to fluctuating hormones, making gum care more important during these times.
Professional Dental Care and Preventive Strategies
Professional care is the “second line of defense” that strengthens what you do at home. It targets plaque and tartar you can’t remove yourself, monitors early changes, and applies treatments that harden enamel and protect gums.
- Professional care supplements daily hygiene for comprehensive protection: Daily brushing/flossing manages soft plaque; professional visits remove hardened deposits, check for decay and gum disease, and customize strategies (fluoride, sealants, hygiene coaching) so problems are prevented, not just treated.
- Frequency and Importance of Dental Visits: Regular visits keep small issues small, reduce emergency risk, and improve long-term tooth and gum health.
- Standard six-month checkups: Twice-yearly exams/cleanings suit many people: they allow early detection of cavities and gum inflammation, routine polishing, and periodic X-rays when indicated.
- Tailoring frequency for high-risk individuals: If you’re at higher risk of gum disease or cavities, dry mouth, diabetes, pregnancy, smokers/vapers, orthodontic appliances, many restorations, or reduced dexterity your dentist may suggest every 3–4 months.
- Professional Cleaning: A professional cleaning removes hardened tartar (calculus) and biofilm below the gumline that normal brushing can’t reach.
- Scaling and root planing to remove tartar: Scaling dislodges plaque/tartar above and below the gums; root planing smooths root surfaces, helping gums reattach and reducing pocket depth and bleeding.
- Polishing to smooth teeth surfaces: Polishing removes surface stains and residual plaque, leaving enamel smoother so new plaque adheres less readily and is easier to brush off.
- Fluoride Treatments and Sealants: Both strengthen vulnerable areas: fluoride hardens enamel; sealants create a physical barrier over deep grooves.
- Mechanisms and benefits: Fluoride promotes remineralization and makes enamel more acid-resistant, lowering cavity risk. Sealants flow into pits/fissures of molars to block bacteria and acids, protecting areas toothbrush bristles struggle to reach.
- Ideal candidates and usage: Fluoride varnish is useful for children, teens with braces, adults with dry mouth or exposed roots, and anyone with recent cavities often applied every 3–6 months. Sealants are ideal soon after molars erupt (kids/teens) and for adults with deep, stain-prone grooves but no decay.
- Oral Cancer Screening: Early detection saves tissue and improves outcomes; screening is fast and painless.
- Visual and tactile exams: Dentists inspect lips, cheeks, tongue, floor of mouth, palate, and throat; they gently palpate tissues and neck nodes to feel for lumps or areas that don’t heal.
- Risk assessment: Risks include tobacco (any form), heavy alcohol, persistent irritation, HPV infection, prior lesions, age over 40, and sun exposure to the lips. High-risk patients may need more frequent checks.
- Diagnostic Tools: Imaging complements the clinical exam to reveal issues not visible to the eye.
- X-rays for hidden decay and bone assessment: Bitewings detect cavities between teeth; periapicals assess roots and infections; panoramic images survey jaws and impacted teeth. Dentists follow ALARA principles to keep radiation as low as reasonably achievable.
- Digital imaging advances: Digital sensors reduce radiation and give instant images. Adjuncts like transillumination and fluorescence-based caries detection help spot early lesions; 3D cone-beam CT may be used for implants, complex roots, or impacted teeth.
- Tailored Preventive Programs: Your plan should reflect your mouth, habits, and risks, not a one-size-fits-all checklist.
- Education customized to patient needs:Coaching covers brushing technique and frequency, interdental aids (floss, picks, brushes), prescription-strength fluoride when needed, diet timing to reduce “acid attacks,” and managing dry mouth or reflux that raises cavity risk.
- Incorporation of new technologies such as laser therapy: Lasers can reduce bacteria in periodontal pockets, aid gingival procedures with minimal bleeding, desensitize roots, and help detect early decay. Your dentist will weigh benefits, cost, and suitability for your case.
Oral Health and Overall Wellness Connection
The mouth serves as a mirror and gateway to the body’s overall health. Oral health encompassing the teeth, gums, and oral tissues closely reflects and impacts systemic wellness. Poor oral health can contribute to or exacerbate various diseases, while systemic conditions can manifest symptoms in the mouth.
- Cardiovascular Disease: Inflammation Link: Chronic inflammation from gum disease (periodontitis) can increase systemic inflammatory markers, contributing to arterial inflammation and atherogenesis. This inflammation may raise the risk of heart attack, stroke, and other cardiovascular events.
- Bidirectional Relationship with Gum Health: Diabetes impairs blood sugar control and weakens immune response, increasing vulnerability to gum infections. Conversely, severe gum disease can worsen blood glucose control, making diabetes management more difficult.
- Respiratory Infections: Oral pathogens can be inhaled into the lungs, especially in individuals with compromised respiratory health or older adults, leading to pneumonia and other respiratory infections.
Advanced Dental Treatments and Innovations
Restorative dentistry plays a crucial role in maintaining oral health by repairing damaged teeth and restoring functionality and aesthetics. It combines traditional techniques with modern materials and technology to provide durable, natural-looking solutions for various dental issues.
Key aspects of restorative dentistry include:
- Use of modern filling materials like composite resins and ceramics that offer strength and a natural appearance.
- Application of crowns and bridges to protect damaged teeth and replace missing ones, ensuring proper chewing and smile restoration.
- Performance of root canal therapy to save infected or damaged teeth by removing pulp, disinfecting canals, and sealing them.
- Incorporation of cosmetic procedures such as whitening, veneers, and bonding to enhance tooth color, shape, and alignment.
- Utilization of dental implants as a permanent solution for tooth loss, with high success rates following surgical placement and bone integration.
- Adoption of laser and regenerative therapies to offer minimally invasive treatments and promote gum and bone regeneration.
- Implementation of digital dentistry techniques, including 3D scanning, printing, and CAD/CAM technology, for precise, efficient, and comfortable dental restorations.
Special Considerations in Oral Care
Special considerations in oral care are essential to address the unique needs of different populations, ensuring effective prevention, treatment, and maintenance of oral health across all life stages and medical conditions.
- Elderly Oral Health Needs: Challenges include gum recession, dry mouth (xerostomia) often due to medications, increased root caries risk. Prevention involves regular hygiene, saliva substitutes, and monitoring medication effects.
- Pediatric Oral Care: Focus on monitoring tooth eruption stages, establishing hygiene habits, motivating children through education, and preventive methods such as fluoride and sealants.
- Care for Immunocompromised Patients: These patients have higher oral infection risks, requiring close coordination with medical teams and personalized oral hygiene protocols.
- Dental Anxiety Management: Psychological approaches like cognitive behavioral therapy and sedation options (nitrous oxide, oral, or IV sedation) improve patient comfort and compliance.
- Denture and Prosthetic Care: Daily cleaning and tissue health monitoring prevent infections and discomfort. Professional adjustments are needed to maintain fit and function.
Building and Sustaining a Lifelong Oral Health Plan
Building and sustaining a lifelong oral health plan is vital for maintaining strong, healthy teeth and gums throughout all stages of life. Successful long-term oral health requires consistent habits, adaptation to changing needs, and proactive education.
Key elements include:
- Parental guidance is essential in establishing proper oral hygiene routines early in childhood.
- Encouraging adolescents to develop independent self-care promotes responsibility and durable oral health habits.
- Oral care routines must evolve to meet changing needs due to age, health status, and lifestyle factors.
- Promoting oral health literacy within families and communities increases awareness of best practices and risks.
- Community-based prevention programs provide screenings, fluoride treatments, and education to wider populations.
- Utilization of digital tools like oral health apps and smart toothbrushes supports consistent care and monitoring.
- Recognizing early symptoms such as gum inflammation or tooth sensitivity enables timely treatment.
- Regular dental check-ups provide professional oversight and early detection of dental issues.
- Promptly addressing oral health problems prevents progression and costly interventions.
- Embedding these practices fosters lifelong oral wellness and reduces risks of disease and tooth loss.
This table provides a clear, concise overview helping readers quickly grasp important oral health issues and management approaches
| Oral Health Topic | Common Causes | Prevention Strategies | Treatment Options |
| Dental Caries (Tooth Decay) | Poor oral hygiene, sugary/acidic diet, dry mouth | Regular brushing and flossing, fluoride use, diet control | Fillings, crowns, root canal therapy |
| Periodontal Diseases | Plaque buildup, smoking, systemic diseases | Proper cleaning, smoking cessation, regular dental visits | Professional cleaning, scaling and root planing |
| Oral Cancer | Tobacco, alcohol, HPV infection, sun exposure | Avoid tobacco and alcohol, HPV vaccination, screenings | Surgical removal, radiation, chemotherapy |
| Oral Thrush | Weakened immunity, antibiotics, steroids | Good oral hygiene, managing underlying conditions | Antifungal medications |
| Dental Erosion | Acid reflux, frequent acidic food/drink intake | Diet modifications, fluoride treatments | Restorative treatments, bonding, crowns |
| Dry Mouth (Xerostomia) | Medications, dehydration, systemic diseases | Hydration, saliva substitutes, avoid alcohol | Medications to stimulate saliva, oral moisturizers |
Conclusion
Oral health impacts vital functions and overall wellness. Maintaining it involves good daily hygiene brushing, flossing, and tongue cleaning alongside proper nutrition and avoiding harmful habits like smoking. Common problems include tooth decay, gum disease, and oral cancer. Regular dental visits ensure early detection and professional care such as cleaning, fluoride application, and screenings.
Modern dentistry offers restorative and cosmetic treatments like fillings, crowns, implants, and laser therapies. Special attention is needed for children, elderly, and immunocompromised individuals. Creating lifelong oral care habits through education and preventive strategies supports long-term health and reduces systemic disease risks.
FAQs
What is oral health, and why is it important?
Oral health means being free from mouth pain, infections, gum disease, and tooth decay. It impacts our ability to chew, speak, and smile, influences nutrition, and affects social interactions and self-esteem.
What are the main types of teeth and their functions?
Teeth types include incisors (cutting), canines (tearing), premolars, and molars (grinding). Their layers enamel, dentin, and pulp work together to protect and perform chewing efficiently.
How does saliva contribute to oral health?
Saliva lubricates the mouth, helps digestion, has antimicrobial properties, and buffers acids to protect tooth enamel from decay.
What causes dental caries (tooth decay)?
Tooth decay occurs when acid-producing bacteria metabolize sugars, eroding the enamel. Risk factors include poor oral hygiene, frequent sugary or acidic food intake, dry mouth, deep tooth grooves, and certain medical conditions.
How do periodontal diseases affect oral health?
Gingivitis causes gum inflammation and bleeding; if untreated, it can progress to periodontitis, leading to tissue and bone damage, gum recession, tooth mobility, and loss.
What are some common oral conditions besides caries and gum disease?
These include aphthous ulcers (canker sores), oral thrush (fungal infection), dental trauma, and dental erosion from acids unrelated to bacteria.
What are the best daily oral hygiene practices?
Brushing twice daily for two minutes with proper technique, flossing daily, cleaning the tongue, using mouthwash appropriately, and choosing fluoride toothpaste support healthy teeth and gums.
How do nutrition and lifestyle affect oral health?
Nutrients like calcium, vitamin D, and vitamin C help maintain strong teeth and gums. Avoiding sugary, acidic, and sticky foods protects enamel. Hydration supports saliva flow, while smoking and alcohol increase risks of gum disease and oral cancers.
Why are regular dental visits important?
Regular check-ups enable early detection and treatment of dental issues, professional cleaning to remove tartar, fluoride applications, sealants, and oral cancer screenings to maintain overall oral health.
What advanced dental treatments are available?
Modern options include durable composite fillings, crowns, bridges, root canal therapy, cosmetic procedures (whitening, veneers), dental implants, laser therapy, regenerative treatments, and digital dentistry technologies for precise restorations.
Are there special considerations for oral care in certain groups?
Yes, elderly individuals, children, immunocompromised patients, and those with dental anxiety or prosthetics require tailored hygiene practices and professional support.
How can I build and maintain a lifelong oral health plan?
Start early with parental guidance, encourage independent care during adolescence, adapt routines with age and health changes, engage in community programs, use self-monitoring tools, maintain a preventive mindset, and keep regular dental appointments.
Reference
- American Dental Association: Oral Health Topics
https://www.ada.org/en/member-center/oral-health-topics - Centers for Disease Control and Prevention (CDC): Oral Health
https://www.cdc.gov/oralhealth/index.html - Mayo Clinic: Dental Health Tips and Oral Care
https://www.mayoclinic.org/healthy-lifestyle/adult-health/in-depth/dental/art-20047475 - World Health Organization (WHO): Oral Health
https://www.who.int/health-topics/oral-health - National Institute of Dental and Craniofacial Research (NIDCR)
https://www.nidcr.nih.gov/health-info - Oral Health Foundation (UK)
https://www.dentalhealth.org/ - British Dental Association (BDA)
https://bda.org/advice/Pages/Oral-health-advice.aspx - National Health Service (NHS) – Oral Health
https://www.nhs.uk/live-well/healthy-body/take-care-of-your-teeth-and-gums/ - Cleveland Clinic: Oral Health and Hygiene
https://my.clevelandclinic.org/health/articles/10916-oral-health
Dr. Amiah Rainey researches diet–disease relationships with expertise in vitamins, minerals, and biomarker methods. She earned a PhD from Harvard T.H. Chan School of Public Health (2019) and completed a postdoctoral fellowship at the NIH/NIDDK. With ~20 peer-reviewed publications (example) and experience on NIH-funded cohort studies, Amiah translates complex evidence into practical guidance. She advises on study design, evidence grading, and data transparency. Profiles: ORCID, Google Scholar; list affiliations and any disclosures.

