Rheumatoid arthritis (RA) is a chronic autoimmune disorder where the immune system attacks the joint lining, causing pain, swelling, stiffness, and joint damage. It often affects both sides of the body symmetrically and can impact organs like the heart and lungs.
Key Takeaways
- Autoimmune disease targeting the synovium, causing chronic inflammation and joint deformity.
- Common symptoms: pain, swelling, morning stiffness, fatigue, and symmetrical joint involvement.
- Risk factors include genetics, smoking, hormonal imbalance, and environmental exposures.
- Diagnosis involves clinical evaluation, blood tests (RF, anti-CCP), and imaging for inflammation.
- Main treatments: DMARDs, biologics, corticosteroids, and NSAIDs to slow disease progression.
- Physical therapy, balanced diet, and stress management improve joint mobility and quality of life.
- Early detection prevents irreversible joint damage and long-term disability.
What Is Rheumatoid Arthritis?
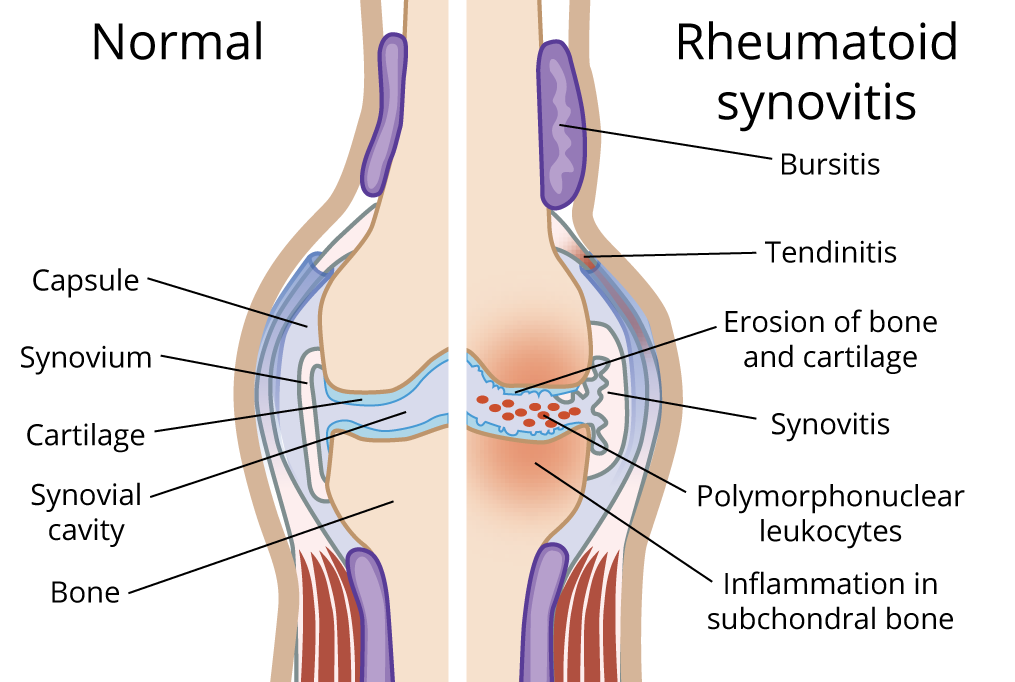
Rheumatoid arthritis is different from osteoarthritis, which typically results from wear and tear over time. While osteoarthritis focuses on cartilage breakdown, RA results from the immune system attacking the lining of the joints, called the synovium. This attack triggers swelling, pain, warmth, and stiffness, most intense in the morning or after rest. Unlike osteoarthritis, RA often involves the same joints on both sides of the body, such as both hands or both knees.
Symptoms of Rheumatoid Arthritis
The symptoms of rheumatoid arthritis (RA) can be wide-ranging and often change over time, affecting both joints and other parts of the body. Recognizing these symptoms early is important for getting timely medical care and preventing lasting joint damage.
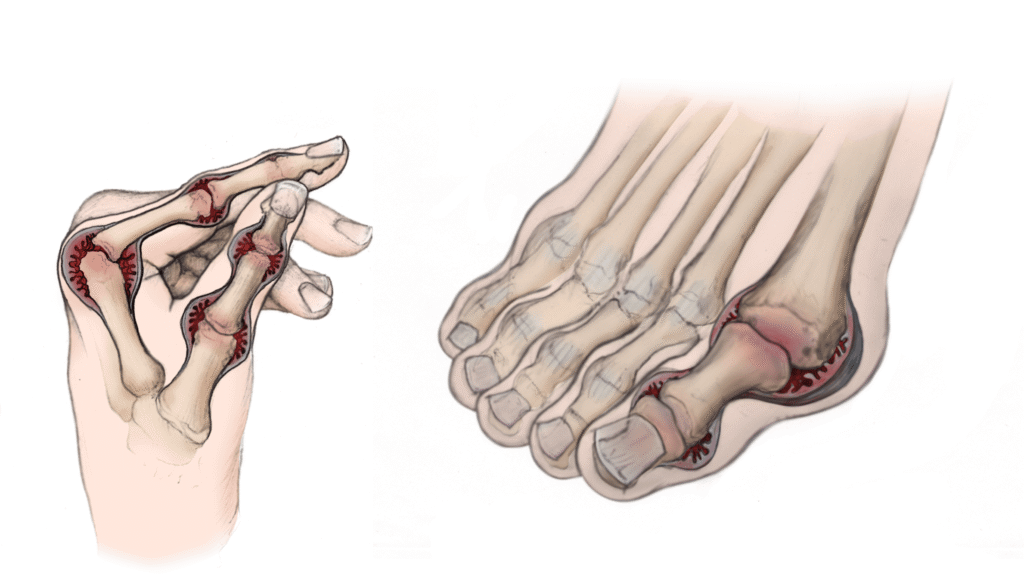
Rheumatoid arthritis most commonly begins subtly, often affecting the small joints in the hands and feet, but any joint can be involved.
Key Symptoms of Rheumatoid Arthritis
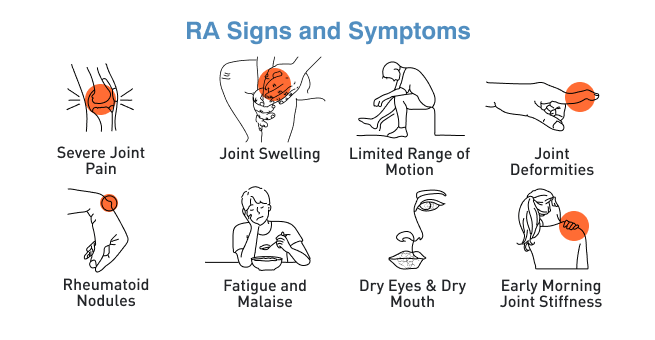
RA produces both joint-related and systemic symptoms. Here are the core signs most often seen:
- Pain and swelling: Joints, especially fingers, wrists, ankles, and toes often become tender, swollen, and may feel warm to the touch.
- Stiffness: Stiffness is usually most noticeable in the morning or after rest and can last for over an hour in RA, which distinguishes it from other types of arthritis like osteoarthritis.
- Redness and warmth: Inflamed joints often look red and feel warm.
- Movement difficulties: Swollen or painful joints can make it hard to grip, bend, or kneel.
- Symmetrical involvement: RA typically affects the same joints on both sides of the body for example, both hands or knees.
Systemic and Other Symptoms
Rheumatoid arthritis affects more than just joints and can cause symptoms throughout the body.
- Fatigue: Many people experience persistent tiredness, even when well-rested.
- Fever: Low-grade fever may occur, especially during disease flares or periods when symptoms intensify.
- Loss of appetite and weight loss: Chronic inflammation can decrease appetite, sometimes resulting in weight loss.
- Rheumatoid nodules: Firm lumps can appear under the skin near affected joints, such as the elbows or fingers.
- Dryness in eyes and mouth: Inflammation can cause dry eyes and mouth, making these areas uncomfortable.
- Mood changes: Ongoing pain and fatigue can affect emotional wellbeing, sometimes resulting in depression or anxiety.
Organ and Tissue Complications
Long-term RA can lead to problems in organs and other tissues:
- Lung involvement: Scarring or inflammation may cause coughing or shortness of breath.
- Heart issues: Inflammation can increase risk for heart conditions.
- Blood vessels: In rare cases, inflammation affects blood vessels, causing nerve, skin, or organ damage.
- Blood problems: Some people develop anemia and a low red cell count due to ongoing inflammation.
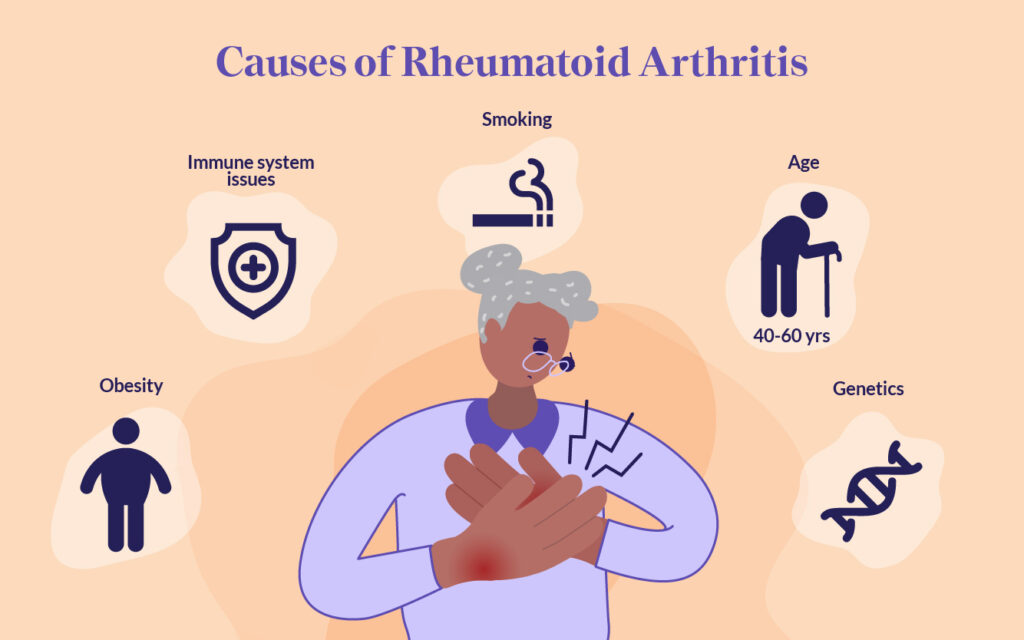
Causes of Rheumatoid Arthritis
Rheumatoid arthritis (RA) doesn’t have one single cause; instead, it develops from a complex mix of genetic, immune, and environmental factors. Understanding these helps people gauge their own risk and take steps to protect joint health.
Autoimmune Mechanisms
RA starts when the immune system misidentifies healthy joint linings as dangerous, triggering an attack. This misfire possibly set off by a virus, bacteria, or other trigger leads immune cells to rush the joint lining (synovium), creating persistent inflammation. Over time, chemicals released during this process damage joint structures and can cause permanent changes if untreated.
Genetic Influences
Genes are important, but not the sole cause. Several genetic markers have been identified, most notably differences in the HLA-DRB1 gene found on chromosome 6. These genes influence how your immune system responds. About half the risk for getting RA comes from genetic factors, with variations such as HLA-DRB1, STAT4, TRAF1/C5, and PTPN22 linked to increased susceptibility and sometimes more severe symptoms. Family history matters too; people with close relatives who have RA are at a higher risk.
Environmental and Lifestyle Factors
Environmental exposures play a big role:
- Smoking: The strongest known lifestyle risk factor, especially in those with a genetic predisposition. Smoking increases both the risk and severity of the disease.
- Hormones: Women are two to three times more likely to develop RA, perhaps due to the effects of estrogen on the immune response.
- Diet: Eating a lot of red meat and lacking vitamin C may raise risk, while diets rich in fish and omega-3s might help lower it.
- Obesity: Being overweight increases risk and may worsen disease progression.
- Gum Disease and Lung Health: Long-term periodontal (gum) infections and lung problems have both been linked to a higher chance of developing RA.
- Age and Sex: RA can begin at any age, but usually starts in middle age and is more common in women.
- Other Exposures: Pollutants, silica dust (found in some jobs), high sodium intake, and certain viral or bacterial infections can also influence risk.
Risk Factors of Rheumatoid Arthritis
Research shows that RA is an autoimmune disease, meaning the immune system mistakenly attacks the tissue lining the joints. This causes inflammation, pain, and swelling, but can also affect nearby bones, cartilage, tendons, and ligaments. Let’s break down the main factors linked to the onset of RA.
Autoantibodies & Biomarkers
Certain proteins produced by the immune system (autoantibodies), especially rheumatoid factor (RF) and anti-citrullinated peptide antibodies (ACPA), mark the presence of RA and often signal a more severe disease. These autoantibodies may exist years before symptoms start.
Social and Economic Factors
Access to healthcare and resources also affects risk, with people from disadvantaged backgrounds facing higher chances due to stress, limited access to preventive care, and poorer overall health habits.
Diagnosis
Diagnosing RA combines careful clinical review, targeted blood tests, and imaging methods. It’s important to seek expert advice promptly if symptoms persist, as early diagnosis is key to preventing irreversible joint damage.
Clinical Evaluation
Doctors start by reviewing symptoms and conducting a thorough physical exam. They look for swollen, tender joints, symmetry, and stiffness patterns. Additional signs like nodules or dry eyes might be present. Gathering detailed information about symptom onset, family history, and daily function guides further testing.
Laboratory Tests
Blood tests help confirm rheumatoid arthritis and rule out other conditions with similar symptoms. They measure inflammation levels, detect specific antibodies, and identify changes in blood cell counts that often occur with RA.
- Rheumatoid factor (RF): An antibody seen in many RA cases but not specific.
- Anti-cyclic citrullinated peptide (anti-CCP/ACPA): Highly specific to RA and signals a potentially more aggressive disease.
- Inflammation markers: Erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) rise during inflammation.
- Complete blood count (CBC): Can show anemia or low red cell count from chronic inflammation.
- Other autoantibodies: Tests rule out similar diseases (lupus, Sjogren’s) and viral triggers.
Proven Treatments for Rheumatoid Arthritis
While there is no cure for rheumatoid arthritis, modern treatments can manage symptoms, slow disease progression, and improve quality of life. Treatment plans are tailored to each person based on how severe the disease is and how well they respond to medications.
Medications
The main aims are to reduce inflammation, relieve pain, maintain joint mobility, and prevent long-term damage. Early treatment offers the best chance to protect joint health.
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): NSAIDs, such as ibuprofen and naproxen, help ease pain and reduce swelling. They do not stop the disease from progressing, but they can make daily activities more comfortable.
- Disease-Modifying Antirheumatic Drugs (DMARDs): Drugs like methotrexate slow the immune system’s attack on joints, helping to prevent permanent damage. Other options, such as sulfasalazine and hydroxychloroquine, may be used alone or in combination. Regular blood tests are needed to monitor for side effects.
- Biologic Agents: Biologics, including TNF inhibitors and IL-6 blockers, target specific parts of the immune system. They are often prescribed when standard DMARDs are not enough to control symptoms.
- Corticosteroids:These powerful anti-inflammatory drugs, such as prednisone, can quickly calm inflammation during flares. They are usually used short term to avoid side effects from long-term use.
Therapy
Therapy plays a key role in managing rheumatoid arthritis alongside medication, helping people maintain movement, reduce stiffness, and protect joint function in daily life.
- Physical Therapy: Specialized exercises improve flexibility, joint function, and muscle strength. This helps maintain mobility and reduces stiffness.
- Occupational Therapy:Therapists teach ways to perform daily tasks with less strain on joints. This may include using adaptive tools or changing movement techniques.
Surgery and Advanced Care
When severe joint damage occurs despite treatment, surgery may restore function and relieve pain. Common procedures include:
- Knee or hip replacement
- Tendon repair
- Corrective surgery for joint deformities
Lifestyle Changes to Manage Rheumatoid Arthritis
While medications are essential for managing RA, lifestyle changes can play a crucial role in improving quality of life and managing symptoms.
- Exercise: Regular exercise, including range-of-motion exercises, strength training, and aerobic activities like walking or swimming, helps maintain joint flexibility and muscle strength.
- Diet: A balanced diet rich in omega-3 fatty acids, fruits, and vegetables can help reduce inflammation. Avoiding processed foods and red meats may also be beneficial.
- Rest: Adequate rest is necessary, especially during flare-ups, to allow the body to recover and reduce inflammation.
- Stress Management: Techniques like meditation, deep breathing, and acupuncture may help manage stress and pain.
Complications of Rheumatoid Arthritis
Rheumatoid arthritis can lead to several complications, including:
- Joint Damage: Over time, RA can cause irreversible joint damage, deformities, and loss of mobility.
- Heart Disease: RA increases the risk of heart disease, as inflammation can contribute to the buildup of plaque in the arteries.
- Lung Disease: Chronic inflammation can lead to scarring in the lungs, causing breathing difficulties.
Infections: Treatments for RA, especially those that suppress the immune system, can increase the risk of infections.
Conclusion
Rheumatoid arthritis is a complex autoimmune disease that can affect far more than just the joints. Left untreated, it may lead to lasting damage and impact overall health, but early diagnosis and proactive management can change the course of the condition.
With modern medications, tailored therapy, and healthy lifestyle habits, many people successfully control symptoms, protect joint function, and maintain an active life. Understanding the signs, knowing the risk factors, and working closely with healthcare professionals are the most effective steps toward living well with RA.
FAQs
Can I live a normal life with rheumatoid arthritis?
Yes, with proper treatment and lifestyle changes, many people with rheumatoid arthritis lead full and active lives.
What foods should I avoid with rheumatoid arthritis?
Avoid processed foods, sugary snacks, and red meats, as they can increase inflammation. Opt for a diet rich in omega-3 fatty acids, fruits, and vegetables.
Is rheumatoid arthritis genetic?
Yes, genetics play a significant role in the development of rheumatoid arthritis. A family history of RA increases the risk of developing the disease.
What is the most common medication for rheumatoid arthritis?
The most commonly prescribed medications for RA include disease-modifying antirheumatic drugs (DMARDs), such as methotrexate, and nonsteroidal anti-inflammatory drugs (NSAIDs).
Can exercise help manage rheumatoid arthritis?
Yes, regular exercise helps maintain joint mobility, build muscle strength, and reduce stiffness. It’s important to work with a physical therapist to design a safe exercise routine.
When is surgery necessary for rheumatoid arthritis?
Surgery may be needed if joint damage is severe and other treatments, such as medications and physical therapy, are ineffective. Joint replacement surgeries, such as knee or hip replacement, are common in advanced cases.
Reference
- Mayo Clinic – Rheumatoid Arthritis Overview
https://www.mayoclinic.org/diseases-conditions/rheumatoid-arthritis/symptoms-causes/syc-20353648 - Centers for Disease Control and Prevention (CDC) – RA Facts
https://www.cdc.gov/arthritis/basics/rheumatoid-arthritis.html - NHS UK – Rheumatoid Arthritis
https://www.nhs.uk/conditions/rheumatoid-arthritis/ - Causes of Rheumatoid Arthritis: Pfizer
https://www.pfizer.com/disease-and-conditions/rheumatoid-arthritis - Diagnosis and Treatment Guidelines: NIAMS (National Institute of Arthritis and Musculoskeletal and Skin Diseases)
https://www.niams.nih.gov/health-topics/rheumatoid-arthritis/diagnosis-treatment-and-steps-to-take - Detailed Diagnosis Criteria: ACR/EULAR 2010 Classification Criteria
https://pubmed.ncbi.nlm.nih.gov/23221588/ - Rheumatoid Arthritis Treatment Overview: Mayo Clinic
https://www.mayoclinic.org/diseases-conditions/rheumatoid-arthritis/diagnosis-treatment/drc-20353653 - Prognosis and Disease Course: Wikipedia
https://en.wikipedia.org/wiki/Rheumatoid_arthritis
Dr. Carlos Mendoza, MD, PhD, is a rheumatologist and clinical researcher with 15 years of experience in musculoskeletal health, joint preservation, and inflammation management. He earned his PhD in Immunology from University of Toronto and completed his medical residency at Mayo Clinic. Dr. Mendoza’s practice bridges traditional rheumatology with emerging nutraceutical and anti-inflammatory interventions. He has published extensively on cartilage repair and omega-3 supplementation for joint function.