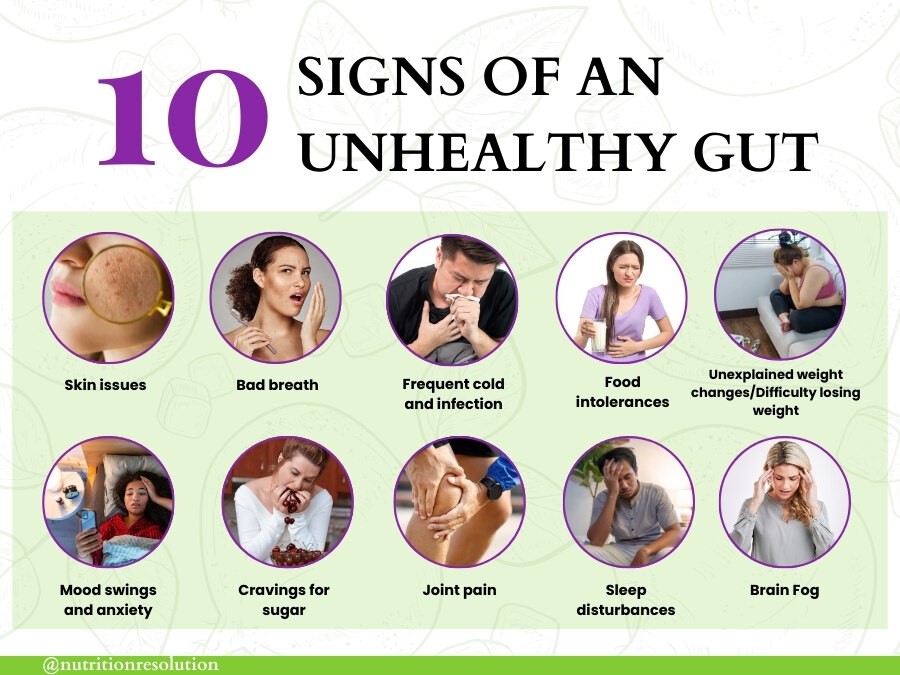
Your gut health affects digestion, energy, immunity, skin, and mood. When gut bacteria become imbalanced, symptoms like bloating, fatigue, skin issues, and frequent illness appear. Recognizing these early helps restore gut balance and overall wellness.
Key Takeaways
- Digestive symptoms like bloating, gas, or irregular bowels signal imbalance.
- Low energy, poor sleep, or mood swings often stem from poor gut function.
- Unexplained weight shifts and recurring skin issues may reflect dysbiosis.
- Food intolerances and frequent illnesses indicate a weakened gut barrier.
- Fiber-rich foods, probiotics, hydration, exercise, and stress control rebuild balance.
- Persistent symptoms or major changes require professional medical evaluation.
Common Signs Unhealthy Gut Needs help
Your gut is like an inner ecosystem, and when it’s out of balance, it can affect your whole body. Spotting the signs early can help you get back on track sooner.
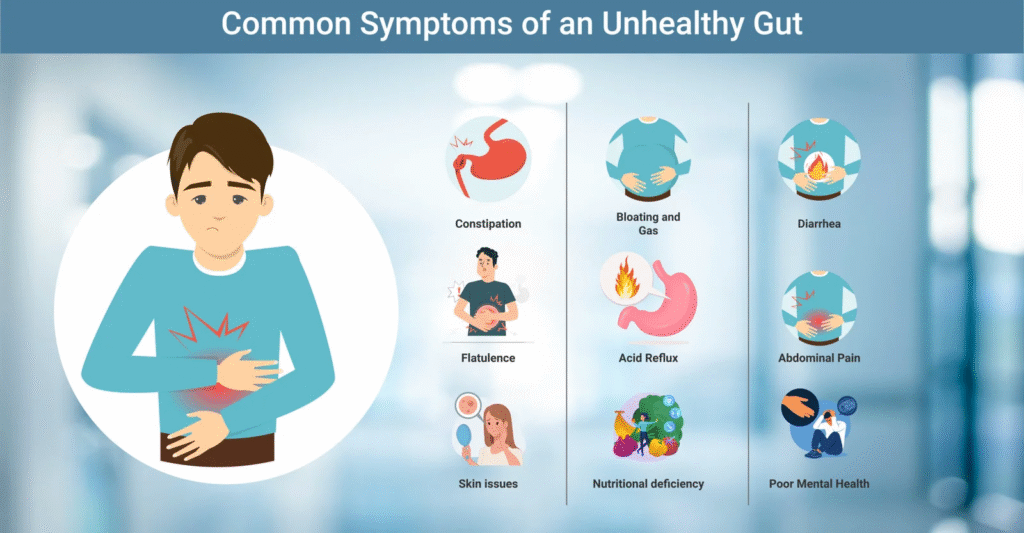
1. Digestive Discomfort
Digestive discomfort such as bloating, gas, constipation, diarrhea, or heartburn is a common yet important indicator of Gut Health. While the occasional episode after a large meal or unusual food is normal, symptoms that occur frequently or persist over time point toward an imbalance in your gut’s ecosystem.
Why Do These Symptoms Occur?
Digestive symptoms can have various causes, including:
- Imbalance in gut bacteria (dysbiosis): Healthy digestion relies on a diverse community of microbes. If harmful bacteria outnumber beneficial ones, digestion becomes less efficient, leading to discomfort.
- Poor diet: Consuming processed foods, excess sugar, or a lack of dietary fiber can change the gut environment and cause gas, bloating, or irregular bowel movements.
- Food intolerances: Ingredients like lactose, gluten, or certain sugars are poorly tolerated, causing gas or loose stools.
- Stress: High stress levels affect how the gut works, sometimes causing cramps, bloating, or changes in bowel habits.
- Lack of movement and hydration: Physical inactivity and insufficient water intake can slow digestion, causing constipation.
When Is Digestive Discomfort a Concern?
Occasional symptoms are usually not a cause for alarm. However, frequent or severe discomfort that disrupts daily life or lasts for more than a few weeks should be evaluated by a healthcare professional, as it signals underlying issues such as irritable bowel syndrome, inflammatory bowel disease, or infections.
Practical Steps to Alleviate Digestive Discomfort
To alleviate digestive discomfort and support gut health, focus on evidence-based, practical steps that address diet, lifestyle, and gentle natural remedies.
- Adopt a high-fiber diet: Eat more vegetables, fruits, whole grains, beans, and legumes to support regular bowel movements.
- Stay hydrated: Aim to drink sufficient water each day to keep digestion running smoothly.
- Incorporate fermented foods: Yogurt, kefir, sauerkraut, and kimchi introduce beneficial bacteria to aid digestion.
- Limit processed foods: Reduce consumption of processed snacks, sugary beverages, and artificial sweeteners.
- Manage stress: Practice relaxation techniques such as deep breathing, meditation, or gentle exercise.
- Eat mindfully: Chew food thoroughly and avoid rushing meals, as this allows your digestive system to process food more efficiently.
- Exercise regularly: Physical activity helps maintain healthy gut motility.
When to See a Doctor
Seek professional advice if you experience:
- Persistent abdominal pain
- Unexplained weight loss
- Blood in stool
- Severe or worsening symptoms
Digestive discomfort is a useful signal from your body. Adopting gut-friendly habits can ease symptoms and support your overall well-being. If symptoms persist, consult with a healthcare provider for personalized care.
2. Low Energy and Poor Sleep
Waking up tired even after a full night’s rest or feeling sluggish throughout the day can sometimes be rooted in gut health problems. Here’s what’s happening and what you can do.
Why the Gut Impacts Energy and Sleep
The gut plays a central role in overall well-being, influencing not just digestion but also energy levels and sleep quality. Here’s how the gut can affect both:
- Nutrient Absorption Issues: If your gut isn’t functioning well, it struggle to absorb vital nutrients such as B vitamins, iron, and magnesium. Deficiencies in these nutrients directly contribute to fatigue and low energy levels.
- Disrupted Microbiome: An imbalance in gut bacteria (dysbiosis) can hinder the production and regulation of important sleep and mood hormones including melatonin and serotonin, which are essential for quality sleep and alertness during the day.
- Chronic Inflammation: Ongoing gut inflammation signals the immune system to release cytokines that can interfere with normal sleep cycles and cause ongoing tiredness.
- Blood Sugar Fluctuations: Poor gut health can affect blood sugar regulation, causing energy drops after eating or unexplained fatigue.
Practical Steps to Improve Energy and Sleep via Gut Health
Here are some practical steps you can take to boost your energy and improve your sleep by supporting your gut health:
- Eat for Gut Health: Emphasize fiber-rich vegetables, whole grains, legumes, nuts, and seeds. These feed beneficial bacteria and help stabilize blood sugar.
- Prioritize Fermented Foods: Incorporate yogurt, kefir, kimchi, and sauerkraut to boost your intake of probiotics, which can support hormone production and sleep quality.
- Manage Stress: Chronic stress disrupts gut flora and hormone balance. Try deep breathing, yoga, or short walks to ease tension.
- Keep a Regular Sleep Routine: Going to bed and waking up at the same time helps regulate your body’s internal clock, which is influenced by your gut-brain axis.
- Limit Caffeine and Alcohol: Both can negatively affect gut bacteria and disrupt deep sleep.
- Consider Prebiotics and Probiotics: These can restore balance to your gut microbiome and have been shown to impact both energy and sleep quality.
3. Unexpected Weight Changes
Sudden changes in weight gain or loss without major shifts in eating habits or physical activity can signal underlying gut health issues.
- Poor Nutrient Absorption: Inflammation or damage to the gut lining can result in the body absorbing fewer nutrients from food, leading to unintentional weight loss.
- Dysbiosis (Imbalanced Gut Flora): An increase in harmful bacteria or a loss of beneficial microbes can affect how your body extracts calories from food, regulates appetite, and stores fat. This imbalance can trigger either weight gain or loss.
- Chronic Inflammation: Persistent inflammation in the gut cause the body to retain fluid, store more fat, or break down muscle, all impacting weight.
- Hormonal Disruption: The gut influences hormones related to hunger and fullness (like leptin and ghrelin). Microbial imbalance disrupts these signals, increasing cravings or blunting satiety.
- Altered Blood Sugar Regulation: Disturbed gut health can affect blood sugar stability, which sometimes leads to overeating, fat storage, or unintended weight fluctuations.
What You Can Do
Improving gut health doesn’t require extreme changes; it starts with consistent, practical steps that support digestive balance and overall wellness. Whether you’re dealing with fatigue, sleep issues, weight fluctuations, or digestive discomfort, making a few targeted adjustments can help restore your gut and improve how you feel day to day.
- Eat a balanced diet rich in fiber: Focus on vegetables, fruits, legumes, and whole grains to nourish beneficial gut bacteria.
- Include probiotic and prebiotic foods: Yogurt, kefir, sauerkraut, and fiber-rich foods support a healthy microbiome.
- Minimize ultra-processed foods: These can aggravate inflammation and promote unhealthy bacterial growth.
- Manage stress: Chronic stress may harm gut health and disrupt hormonal balance.
- Regular exercise: Supports a healthy metabolism and microbial diversity.
- Monitor portion sizes and meal regularity: Consistent eating patterns help regulate metabolism.
- Consult a healthcare provider: Persistent or severe weight changes especially when unexplained warrant professional evaluation to rule out serious conditions.
When to Seek Medical Advice
Most gut-related symptoms can be managed with healthy lifestyle changes, but certain signs indicate the need for professional evaluation. If you notice any of the following, consult a healthcare provider.
- Persistent, rapid weight changes (gain or loss) with no clear cause
- Accompanying symptoms like digestive distress, fatigue, or weakness
- Blood in stool or severe abdominal pain
- History of metabolic, thyroid, or gastrointestinal disorders
4. Skin Troubles
Emerging research consistently demonstrates a strong link between gut health and skin conditions such as acne, eczema, rosacea, and psoriasis. This relationship is often described as the gut-skin axis, a complex communication pathway through which changes in gut microbiota can directly affect skin health.
How an Unhealthy Gut Impacts the Skin
The health of your gut and your skin are closely linked, a relationship often referred to as the “gut-skin axis.” When the gut is imbalanced or inflamed, it can manifest in a variety of skin conditions through several biological pathways.
- Inflammatory Response: An imbalance in the gut microbiome (dysbiosis) can trigger systemic inflammation, which frequently manifests as skin flare-ups acne, eczema, or psoriasis, for example.
- Leaky Gut: Compromised gut lining, often referred to as “leaky gut,” allows toxins and bacteria to enter the bloodstream. This process increases inflammation throughout the body, making skin conditions worse or causing new rashes and irritation.
- Immune System Dysregulation: The gut plays a critical role in regulating immune function. Altered gut flora can over-activate the immune system, leading to skin sensitivities and chronic dermatological issues.
- Microbial Byproducts: Healthy gut bacteria produce substances like short-chain fatty acids (SCFAs), which help reduce inflammation and strengthen both gut and skin barriers. Low production of SCFAs due to poor gut health can reduce the skin’s resilience.
Which Skin Conditions Are Commonly Linked to Gut Health?
Disruptions in gut health are increasingly recognized as contributing factors to various skin conditions. This connection often called the gut-skin axis means that imbalances, inflammation, or dysfunction in the digestive system can manifest as dermatological concerns.
- Acne: Changes in gut bacteria can promote inflammatory pathways that increase oil production and contribute to acne development.
- Eczema (Atopic Dermatitis): Reduced diversity and imbalance of gut microbes are associated with more frequent or severe eczema flare-ups.
- Rosacea: Studies have shown that small intestinal bacterial overgrowth (SIBO) and other gut conditions are significantly more common in people with rosacea; targeting gut health often improves symptoms.
- Psoriasis and Urticaria: Gut dysbiosis and increased intestinal permeability have been observed in individuals with psoriasis and chronic urticaria, suggesting bidirectional communication between gut and skin health.
When to Seek Medical Advice
You should seek medical help for skin troubles related to gut health if you experience persistent or worsening symptoms, especially when skin conditions (like acne, eczema, or rosacea) occur alongside ongoing digestive problems. Warning signs include:
- Chronic skin irritation or flare-ups that don’t respond to topical treatments or lifestyle changes.
- Frequent digestive issues such as frequent bloating, gas, indigestion, or unexplained changes in bowel habits accompanying skin symptoms.
- Severe, spreading, or painful skin lesions, or new skin rashes with fever or signs of infection.
- Unexplained weight changes, fatigue, or mood changes together with skin and gut concerns.
- Sudden or multiple food intolerances that seem to trigger both gut and skin reactions.
- Signs of systemic illness (such as joint pain, persistent malaise, high fever, or blood in stool)
5. Food Intolerances
Food intolerances occur when your digestive system struggles to properly break down or absorb certain foods. Unlike allergic reactions, intolerances typically don’t involve the immune system but can cause significant discomfort:
- Bloating and discomfort after eating: These are common signs that your gut lining may be compromised or that your microbiome lacks diversity.
- Underlying causes: An unhealthy gut can mean reduced numbers or types of beneficial microbes, weakening your ability to digest specific nutrients like lactose or gluten.
- Cycle of irritation: Repeated exposure to poorly tolerated foods can further irritate the gut, worsening symptoms over time.
Why Food Intolerances Develop
Food intolerances often arise when the gut’s ability to process or absorb certain foods becomes impaired due to imbalances in the digestive system. These intolerances can develop because of changes in gut bacteria, weakened gut lining, or insufficient digestive enzymes, making it harder for your body to handle specific foods without discomfort.
- Gut Microbiome Imbalance (Dysbiosis): A healthy, diverse gut microbiome is essential for breaking down a variety of food components. If beneficial bacteria are lacking or outnumbered by harmful microbes, it becomes harder to process certain foods, leading to intolerance symptoms.
- Weakened Gut Lining (“Leaky Gut”): Damage to the gut lining allows undigested food particles to cross into the bloodstream, triggering discomfort and sometimes immune reactions even if true allergies are not present.
- Enzyme Deficiencies: Some people naturally lack enzymes needed to digest specific foods (e.g., lactase for dairy), but poor gut health can further reduce enzyme efficiency, increasing the likelihood of intolerance.
- Sensitivity to Additives: An unhealthy gut may make you more susceptible to discomfort from food additives, preservatives, or artificial sweeteners.
When to Seek Medical Help
Food intolerances are usually manageable with dietary adjustments, but certain warning signs suggest it’s time to consult a healthcare professional. Early evaluation helps ensure you’re not missing a more serious underlying condition.
- Symptoms persist or worsen: If food intolerance symptoms (such as bloating, abdominal pain, diarrhea, or nausea) continue despite eliminating suspected foods, seek medical advice.
- Severe or disruptive symptoms: Consult a doctor if you experience severe pain, vomiting, dehydration, or symptoms that disrupt your daily life or sleep.
- Unexpected weight loss: Any unintentional, unexplained weight loss associated with digestive complaints should always be discussed with a healthcare provider.
- Blood in stool: The appearance of blood (bright red or dark, tarry stools) signals the need for immediate evaluation.
- Signs of malnutrition: Symptoms like fatigue, hair loss, brittle nails, or slow-healing wounds may suggest that intolerances are affecting nutrient absorption.
- Widespread or multiple intolerances: If you develop new or multiple intolerances suddenly, especially with other symptoms, this may indicate a broader gut issue or underlying disease.
6. Frequent Illness or Allergies
Frequent infections, catching every cold that goes around, or suffering from ongoing allergies can all be connected to the health of your gut. This is because nearly 70% of your immune system is located within your digestive tract, making the gut a central player in immune defense and regulation.
How Gut Health Affects Immunity and Allergies
A balanced gut microbiome not only protects against invading pathogens but also educates the immune system, helping it distinguish between harmful substances and harmless particles, reducing excess immune reactions such as allergies and supporting overall resilience.
- Microbial Balance Guides Immune Function: A well-balanced gut microbiome educates and regulates immune cells, helping your body distinguish between harmless particles and real threats. Dysbiosis (imbalanced gut bacteria) can disrupt this process, making you more susceptible to frequent infections or excessive immune reactions like allergies.
- Gut Barrier Integrity: The gut lining acts as a protective shield, keeping pathogens and toxins at bay. If this barrier becomes weakened or “leaky,” foreign particles can slip into the bloodstream, triggering inflammation and inappropriate immune responses, sometimes manifesting as new or worsening allergies.
- Inflammation and Immune Control: Chronic inflammation in the gut can overactivate or suppress immune cells, disrupting the body’s natural ability to fight off infections and manage allergic responses.
Warning Signs
Certain symptoms suggest your gut health need more careful attention. Recognizing these warning signs allows for timely intervention and the prevention of more serious problems.
- Regular colds, respiratory infections, or slow recovery from minor sickness.
- Development of new or worsening allergies (including foods and environmental triggers).
- Frequent sinus, nasal, or chest congestion.
What You Can Do
You can support and improve your gut health through several science-backed strategies focused on diet, lifestyle, and daily habits:
- Support Microbial Diversity: Eat a fiber-rich, plant-based diet to feed beneficial gut bacteria.
- Add Fermented Foods: Incorporate yogurt, kefir, sauerkraut, or kimchi to increase probiotic intake.
- Limit Antibiotic Use: Take antibiotics only when necessary to avoid disrupting healthy gut flora.
- Stay Active and Manage Stress: Physical activity and stress reduction help balance gut and immune health.
When to Seek Medical Help
Frequent infections or ongoing allergies can sometimes be managed with lifestyle changes, but certain warning signs mean medical evaluation is necessary to rule out serious or underlying problems.
- Persistent or Recurrent Infections: Repeated colds, flu, respiratory tract infections, or other illnesses that do not improve or keep returning despite healthy habits.
- Worsening or New Allergies: Sudden development of new allergies, more severe allergic reactions than previously experienced, or allergies that begin affecting multiple organ systems (e.g., skin, digestion, breathing).
- Ongoing Fever or High Temperature: Persistent fever (above 101°F/38.3°C) with or without other symptoms.
- Unusually Slow Recovery: Illnesses (even minor) that last much longer than normal or recovery that takes weeks rather than days.
- Combination with Other Symptoms: Frequent illness or allergies accompanied by unexplained weight loss, night sweats, chronic fatigue, digestive disturbances, blood in stool, or significant skin changes (such as rashes that don’t heal).
- Signs of Dehydration or Malnutrition: Dizziness, very dark urine, extreme thirst, or evidence that frequent illness is affecting your ability to eat and hydrate properly.
- Family or Personal History of Immune Disorders: Increased risk if there is a history of autoimmune disease, immunodeficiency, or cancers of the immune system.
- Children, Elderly, or Immunocompromised: Symptoms in these populations progress quickly and need earlier evaluation.
Causes, Impacts, and Remedies for Unhealthy Guts
Poor diet, stress, antibiotics, and lifestyle factors disrupt gut bacteria, increasing inflammation and health risks. Restoring gut health requires fiber-rich foods, reduced stress, exercise, sleep, and mindful medication use.
| Cause | Impact on Health | Remedy/Recommended Action |
| Poor Diet (low fiber, high sugar) | Digestive discomfort, gut dysbiosis, increased inflammation | Eat more fiber-rich, plant-based foods; reduce added sugars and processed foods |
| Antibiotic Overuse | Reduced microbial diversity, vulnerability to infections | Use antibiotics only when necessary; replenish with probiotics and prebiotic foods |
| Chronic Stress | Altered gut motility, increased inflammation, imbalanced microbiota | Practice stress management, mindfulness, relaxation techniques |
| Lack of Sleep | Weakened immunity, disturbance in gut bacteria balance | Prioritize sleep hygiene and regular sleep patterns |
| Excessive Alcohol/Caffeine | Gut lining irritation, microbiome imbalance, increased inflammation | Limit intake of alcohol and caffeine; increase water consumption |
| Sedentary Lifestyle | Reduced microbial diversity, sluggish digestion | Engage in regular physical activity |
| Frequent Infection or Illness | Inflammation, gut permeability (“leaky gut”) | Address underlying illness promptly, support immunity through nutrition |
| Environmental Exposures (toxins, pollution) | Disrupts beneficial bacteria, may trigger inflammation | Reduce exposures, maintain indoor air quality, wash produce |
| Food Intolerances/Allergies | Bloating, diarrhea, gut inflammation | Identify and eliminate trigger foods; seek professional advice |
| Aging, Chronic Disease | Decline in microbial diversity, impaired barrier function | Adopt dietary/lifestyle habits that support gut health across lifespan |
Ways to Improve Your Gut Health
Supporting your gut health is a powerful way to moderate immune system activity and lower the risk of autoimmune flare-ups. Here’s a comprehensive guide to fostering a balanced, resilient gut microbiome and strengthening your body’s defenses.
1. Eat a Diverse, Whole-Food Diet
Microbial diversity is a hallmark of a healthy gut. Improved diversity helps maintain balance, suppress harmful bacteria, and support overall health.
- Aim for variety: Strive to eat 30+ different plant-based foods weekly, including vegetables, fruits, legumes, nuts, seeds, and herbs.
- Prebiotic-rich foods: Garlic, onions, leeks, asparagus, and bananas fuel healthy gut bacteria.
- Polyphenols for the microbiome: Include berries, green tea, olive oil, and dark chocolate for their powerful antioxidant and gut-supporting properties.
- Resistant starches: Add cooked-and-cooled potatoes, green bananas, and lentils, which reach the colon undigested and feed good microbes.
2. Use Probiotics for Gut Health
Probiotics are live, beneficial microorganisms that help restore microbial balance and support gut integrity.
- Lactobacillus rhamnosus GG: Enhances gut lining and immune function
- Bifidobacterium longum: Reduces inflammation
- Lactobacillus plantarum: Strengthens the gut barrier
- Saccharomyces boulardii: Protects against harmful pathogens
- Bifidobacterium infantis: Reduces IBS symptoms and systemic inflammation
Sources of probiotics:
- Fermented foods: Yogurt, kefir, kimchi, sauerkraut, miso, kombucha
- High-quality supplements: Aim for 10+ billion CFUs, covering several strains.
3. Prioritize the Best Foods for Gut Health
Select foods proven to nourish beneficial bacteria and build a resilient gut:
- Leafy greens (spinach, kale)
- Fermented foods (see above)
- Berries (antioxidant-rich)
- Bone broth (contains amino acids like glutamine for repair)
- Fatty fish (salmon, sardines, rich in omega-3s)
- Turmeric and ginger (natural anti-inflammatories)
4. Avoid the Worst Foods for Gut Health
Certain foods undermine gut barrier function and foster harmful bacteria, particularly problematic for those with autoimmunity.
- Refined sugars, artificial sweeteners
- Processed foods and additives (emulsifiers, preservatives)
- Gluten and dairy (if sensitive)
- Fried or fast food
- Excess alcohol and caffeine
- Large amounts of red and processed meat
5. Manage Stress Levels
Chronic stress increases levels of the hormone cortisol, which can disrupt the balance of your gut microbiome and weaken the protective gut barrier. To support gut and immune health, integrate regular stress management practices:
- Meditation and deep breathing: Calms the nervous system and reduces stress hormones.
- Yoga, walking, and time in nature: Physical movement and exposure to natural environments reduce psychological stress and benefit gut diversity.
- Journaling and gratitude practices: Help process emotions and cultivate a positive mindset, further lowering stress’s physiological impact.
6. Prioritize Quality Sleep
Quality sleep is essential for gut microbial stability and effective immune function.
- Target 7–9 hours each night: Sleep enables repair and balancing of gut bacteria.
- Limit screen time before bed: Blue light can disrupt sleep hormones.
- Maintain a consistent schedule and environment: Stick to regular bedtimes and create a cool, dark, quiet space to support restful sleep.
7. Exercise Regularly
Moderate, consistent exercise encourages a more diverse and balanced gut microbiome and reduces inflammation.
- Aim for 30 minutes of activity daily: Walking, swimming, or cycling are excellent choices.
- Avoid overtraining: Excessive exercise can damage the gut barrier and impair immune response. Balance movement with adequate rest.
8. Use Antibiotics and Medications Wisely
While sometimes necessary, antibiotics can eliminate both beneficial and harmful gut bacteria.
- Take only as prescribed: Avoid unnecessary antibiotic use.
- Replenish good bacteria: After a course, consume probiotic-rich foods or supplements.
- NSAIDs caution: Medications like ibuprofen can irritate the gut lining sparingly and consult your healthcare provider for alternatives.
9. Consider Functional Testing
If you experience ongoing digestive or immune issues:
- Consult a functional medicine provider: Specialized practitioners can assess gut health more comprehensively.
- Investigate imbalances: Testing can reveal gut microbiome disruptions, increased intestinal permeability (“leaky gut”), food sensitivities, and nutrient deficiencies so you can receive personalized recommendations.
Conclusion
Many everyday symptoms like bloating, unexplained fatigue, mood swings, frequent illness, or skin flare-ups can be signs of an unhealthy gut. These issues often stem from imbalances in gut bacteria, poor nutrient absorption, inflammation, or a weakened gut barrier. Recognizing these connections allows you to address root causes instead of just treating symptoms.
Improving gut health involves consistent habits, eating a high-fiber, plant-rich diet, including fermented foods, staying active, managing stress, and getting quality sleep. If symptoms persist or worsen, a healthcare provider can help identify deeper issues such as food intolerances, infections, or underlying conditions. With the right changes, your gut can recover and support better overall health.
FAQ
What are typical symptoms of an unhealthy gut?
Digestive issues, fatigue, skin problems, frequent colds, mood changes, and food intolerances can all signal your gut health needs attention.
Can gut health impact mental health?
Yes, the gut-brain connection means gut imbalances can influence anxiety, depression, and overall mood.
Why do I crave sugar when my gut is unhealthy?
Certain gut bacteria thrive on sugar and can increase cravings when the microbiome is unbalanced.
Does poor sleep mean I have an unhealthy gut?
Sleep disturbances can be related to gut health since the gut affects hormone production linked to sleep cycles.
How does diet affect my gut?
Eating processed foods and low-fiber diets can harm good bacteria, leading to gut imbalance.
Can antibiotics harm my gut?
Yes, antibiotics can kill both harmful and helpful bacteria, sometimes causing digestive upset or imbalance.
How can I naturally improve gut health?
Eat more fiber and fermented foods, manage stress, sleep well, and exercise regularly to support a healthier gut.
Are probiotics always necessary for gut health?
Not everyone needs them. A balanced diet often supports gut health, but probiotics can help some people ask your doctor.
Can gut problems cause skin issues?
Yes, conditions like eczema, acne, or rashes may be linked to poor gut health or inflammation.
When should I see a doctor about gut symptoms?
If digestive issues are severe, ongoing, or affecting your quality of life, consult a healthcare professional for proper diagnosis and treatment.
References
- Mayo Clinic – Gut health symptoms and irritable bowel syndrome:
https://www.mayoclinic.org/diseases-conditions/irritable-bowel-syndrome/symptoms-causes/syc-20360016 - Cleveland Clinic – Leaky gut, causes, and immune implications:
https://my.clevelandclinic.org/health/diseases/22724-leaky-gut-syndrome - Cleveland Clinic – Gut microbiome basics:
https://my.clevelandclinic.org/health/body/25201-gut-microbiome - Johns Hopkins Medicine – Gut microbiome and immunity:
https://pure.johnshopkins.edu/en/publications/gut-microbiome-features-associate-with-immune-checkpoint-inhibito - Harvard Health – The gut-brain connection:
https://www.health.harvard.edu/diseases-and-conditions/the-gut-brain-connection - ScienceDirect – Gut-skin axis and skin health:
https://www.sciencedirect.com/science/article/abs/pii/S0738081X21001930 - NIH (National Institutes of Health) / Frontiers – Microbiome, energy, sleep, mental health links:
https://academic.oup.com/sleepadvances/advance-article/doi/10.1093/sleepadvances/zpaf023/8115573
Dr. Emily Zhang, MD, is a gastroenterologist and integrative medicine specialist with 10 years of clinical experience in digestive health and microbiome science. She completed her medical degree at University of Chicago Pritzker School of Medicine and fellowship at Massachusetts General Hospital. Dr. Zhang specializes in gut-brain interactions, microbiota diversity, and nutrition-driven gut repair. She has contributed to NIH-funded studies on probiotics and authored patient education resources on functional gut disorders.


