Sleep disorders are conditions that disrupt the body’s normal sleep cycle, leading to poor rest and daytime fatigue. They include insomnia, sleep apnea, narcolepsy, and restless legs syndrome. These disorders can impact overall health, cognitive performance, and mood if left untreated.
Key Takeaways
- Over 80 types of sleep disorders are recognized, with varying causes and symptoms.
- Common signs include difficulty sleeping, excessive tiredness, snoring, and abnormal nighttime behavior.
- Causes range from genetics and medical or mental conditions to poor lifestyle and environmental factors.
- Diagnosis involves clinical assessment, sleep studies, and monitoring tools like polysomnography or actigraphy.
- Treatments include cognitive-behavioral therapy (CBT-I), CPAP devices, medications, and lifestyle modification.
- Early diagnosis and consistent management restore sleep quality and prevent long-term health risks.
What Are Sleep Disorders?
Sleep disorders impair your ability to obtain restful and sufficient sleep. The body requires 7 to 9 hours of quality sleep nightly for optimal functioning, but many people fail to meet this standard due to underlying sleep issues. The International Classification of Sleep Disorders (ICSD) categorizes over 80 types of sleep disorders based on symptoms, affected body systems, and underlying causes.
Recognizing the Signs of Sleep Disorders
Sleep disorders often present through a range of symptoms that affect both nighttime rest and daytime functioning. Being aware of these signs can help identify when professional evaluation and treatment are needed.
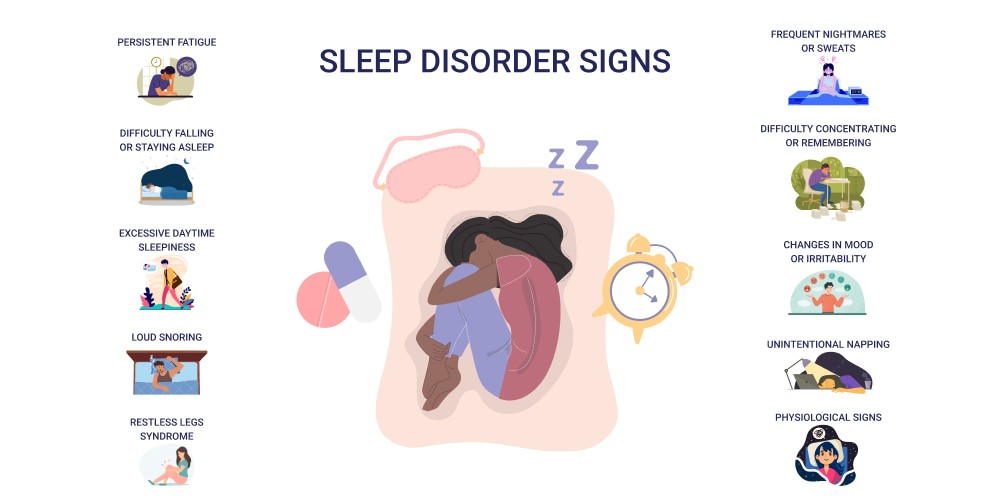
- Difficulty Falling or Staying Asleep: This is often the hallmark of insomnia, where individuals struggle to initiate sleep (sleep onset insomnia) or wake up frequently during the night and have trouble returning to sleep (maintenance insomnia). This disruption can leave a person feeling unrested despite spending sufficient time in bed.
- Excessive Daytime Sleepiness: This symptom is typical in conditions such as narcolepsy and sleep apnea. It manifests as an overwhelming urge to sleep during the day, which can interfere with daily activities and increase the risk of accidents. People may find themselves unintentionally dozing off even during important or routine tasks.
- Loud Snoring: Loud, habitual snoring often suggests obstructive sleep apnea (OSA), a disorder where airway obstruction causes repeated breathing pauses during sleep. People with OSA may experience disrupted sleep and oxygen deprivation, leading to daytime fatigue and other health risks.
- Restless Sensations in the Legs: This describes symptoms of restless legs syndrome (RLS), characterized by uncomfortable sensations such as tingling, crawling, or itching in the legs. These sensations often worsen in the evening or night, compelling the person to move their legs, which interrupts the ability to fall asleep or stay asleep.
- Sudden Sleep Attacks: Sudden, irresistible bouts of sleep during the day are a classic sign of narcolepsy. These episodes can occur without warning and severely affect a person’s ability to function safely, especially when driving or operating machinery.
- Abnormal Movements During Sleep: These include behaviors like periodic limb movements, sleep talking, sleepwalking, or acting out dreams (REM sleep behavior disorder). Such activities can fragment sleep or suggest underlying neurological issues.
- Daytime Problems: Sleep disorders don’t just affect nighttime rest; they also impair daytime functioning. Symptoms can include difficulty concentrating or remembering, irritability, mood swings, increased anxiety or depression, and decreased work or academic performance.
Causes of Sleep Disorders
Sleep disorders can develop due to a combination of physical, psychological, and environmental factors. Underlying medical conditions, mental health issues, lifestyle habits, and even genetics can all play a role. In some cases, stress, shift work, or poor sleep environments contribute to ongoing sleep difficulties.
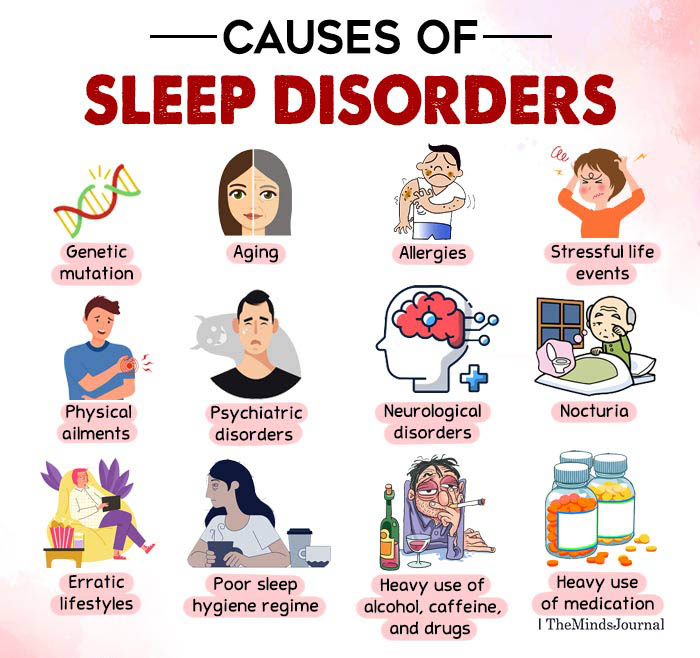
- Genetic Predisposition: Some sleep disorders are familial. Narcolepsy, restless leg syndrome, and specific forms of insomnia have documented genetic links. Family history increases risk, as shown in clinical studies of narcolepsy and insomnia cohorts.
- Age-Related Changes in Sleep Patterns: Older age is linked with lighter, fragmented sleep and reduced deep sleep. These changes increase susceptibility to insomnia and frequent waking. Aging alters circadian rhythms and lessens melatonin production, both supported by sleep research.
- Medical Conditions: Chronic diseases such as arthritis, asthma, COPD, heart failure, and neurological disorders (for example, Parkinson’s or Alzheimer’s disease) commonly disrupt sleep architecture. Pain, breathing difficulties, or abnormal movement during sleep are common mechanisms.
- Mental Health Issues: Anxiety and depression are strongly associated with sleep problems. Persistent stress raises cortisol, activating wakefulness. Psychiatric studies routinely find bi-directional links: sleep disorders increase mental health problems, and vice versa.
- Lifestyle Factors: Shift work, late-night screen use, inconsistent bed and wake times, insufficient exercise, and intake of caffeine or alcohol disrupt normal circadian cues and sleep cycles. Studies confirm these behaviors correlate with higher prevalence of insomnia.
- Environmental Factors: Exposure to noise, light pollution, high or low temperatures, and uncomfortable bedding or bedroom humidity can disrupt sleep continuity. Environmental sleep studies have clearly linked these variables to poorer sleep outcomes.
- Medications and Substances: Stimulants (e.g., some antidepressants, corticosteroids, beta-agonists), decongestants, and psychoactive drugs cause sleep-onset or maintenance problems. Nicotine, alcohol, and some recreational drugs likewise interfere with normal sleep architecture.
Who Is At Risk?
Sleep disorders can affect anyone but are more prevalent among women and increase with age, particularly in adults over 65. Lifestyle factors, medical conditions, stress, and certain medications can contribute to the development of sleep disorders.
Sleep Disorder Diagnosis
Diagnosing sleep disorders involves a careful evaluation combining clinical history, physical exams, questionnaires, and specialized tests. The process aims to identify the specific type of sleep disorder and its underlying causes for effective treatment.
- Clinical Interview: The healthcare provider reviews the patient’s symptoms, medical history, and sleep habits. For reliable insights, input from a bed partner (if possible) is valuable, as they may notice snoring, gasping, limb movements, or unusual behaviors during sleep.
- Sleep Diary: Patients may be asked to keep a sleep log for 1–2 weeks, detailing sleep and wake times, waking events, naps, exercise, caffeine, and alcohol use. This gives the clinician an overview of patterns and potential triggers.
- Polysomnography: Conducted overnight in a sleep laboratory or at home (limited data for the latter). Sensors record several physiologic parameters. Essential for diagnosing complex disorders or when initial evaluations are inconclusive.
- Home Sleep Apnea Test: Portable devices to record breathing and oxygen levels at home. Used when obstructive sleep apnea is suspected and there are no other serious medical conditions.
- MSLT/MWT: Measure propensity for daytime sleepiness, diagnosis of narcolepsy, or assessment of fitness for occupations that require alertness (e.g., pilots).
- Actigraphy: Used for several days to weeks, especially for detecting circadian rhythm or insomnia issues.
- Other Laboratory Tests: Assess for underlying causes such as hypothyroidism, anemia, or substance use that can disrupt sleep
Physical Examination For Sleep Disorder Diagnosis
A physical exam may reveal risk factors such as obesity (linked with sleep apnea), nasal obstruction, or neurological findings indicative of sleep-related movement disorders.
| Test Name | What It Measures | Most Common Uses |
| Polysomnography (PSG) | Brain waves, eye movements, muscle activity, heart rate, respiratory patterns, oxygen levels | Gold standard for diagnosing sleep apnea, narcolepsy, periodic limb movement disorder, parasomnias |
| Home Sleep Apnea Test | Breathing, oxygen levels, heart rate | Diagnosing obstructive sleep apnea (mild cases or high suspicion) |
| Actigraphy | Movement (usually wrist device) | Assessing sleep-wake cycles, circadian rhythm disorders |
| Multiple Sleep Latency Test (MSLT) | Time to fall asleep/enter REM during scheduled naps | Diagnosing narcolepsy and hypersomnia |
| Maintenance of Wakefulness Test (MWT) | Ability to remain awake under soporific conditions | Assessing daytime sleepiness in safety-sensitive roles |
| Overnight Oximetry | Oxygen saturation during sleep | Screen for sleep apnea, hypoventilation |
| Electroencephalogram (EEG), EMG, and EOG | Brain, muscle, and eye electrical activity | Identify seizures, confirm sleep stages as part of polysomnography |
| Laboratory Blood Tests | Thyroid, anemia, drug screens | Rule out medical contributors to sleep symptoms |
Sleep Disorder Treatments
Treatment options for sleep disorders are tailored to the specific condition, focusing on addressing symptoms, improving sleep quality, and enhancing overall well-being. Below are detailed explanations of the key approaches:

- Cognitive Behavioral Therapy for Insomnia (CBT-I): Structured therapy targets negative thoughts and behaviors about sleep. Uses techniques like sleep restriction, stimulus control, and relaxation. Proven in randomized trials as the first-line treatment for chronic insomnia, with durable results.
- Sleep Hygiene Improvements: Establishes regular sleep-wake times, limits screen time before bed, and creates a quiet, dark, and comfortable environment. Evidence supports improved sleep quality by reducing behavioral and environmental triggers.
- Medications: Prescribed according to disorder. Sedative-hypnotics or melatonin agonists for insomnia, stimulants for narcolepsy, and dopamine agonists or anticonvulsants for restless legs syndrome. Used short-term or with therapy, with close monitoring for side effects and dependency.
- Continuous Positive Airway Pressure (CPAP): Device delivers pressurized air via mask, keeping airways open for patients with obstructive sleep apnea. Multiple trials show CPAP improves sleep architecture, reduces daytime sleepiness, and lowers cardiovascular risks.
- Light Therapy: Timed exposure to bright light resets circadian rhythms. Used for delayed sleep phase disorder and seasonal affective disorder, with clinical trials showing benefit in improving sleep-timing and mood.
- Lifestyle Modifications: Regular exercise, management of stress with meditation or yoga, and avoiding caffeine/alcohol in the evening. Lifestyle changes are associated with better long-term outcomes in observational and interventional studies.
- Hypoglossal Nerve Stimulation: Implanted device stimulates tongue muscle via hypoglossal nerve to maintain airway for obstructive sleep apnea. Effective for patients who do not tolerate CPAP, supported by clinical trial data.
Conclusion
Sleep disorders are a diverse group of conditions that disrupt normal sleep, resulting in poor rest and significant daytime challenges. With common forms like insomnia, sleep apnea, restless legs syndrome, and narcolepsy, these disorders can manifest through a variety of symptoms from difficulty sleeping to abnormal night-time behaviours. Their causes range from genetics and medical issues to lifestyle and environmental factors, affecting people of all ages, though risk increases with age and certain health conditions.
Accurate diagnosis is essential and may involve clinical evaluation, sleep diaries, and specialized testing. Fortunately, a wide range of effective treatments exist, including behavioural therapies, improved sleep hygiene, medications, and medical devices. By recognizing symptoms early and seeking appropriate management, individuals can restore healthy sleep, enhance overall quality of life, and lower the risk of long-term health complications.
FAQs
1: How many hours of sleep do adults need per night?
Most adults need 7-9 hours of quality sleep each night, although individual needs may vary slightly.
2: Is it bad to use my phone before bed?
Yes, because screens emit blue light that suppresses melatonin production, delaying sleep onset and reducing sleep quality.
3: Can exercise improve sleep?
Yes, regular exercise promotes deeper and better-quality sleep, but avoid vigorous workouts close to bedtime.
4: Are naps good or bad for nighttime sleep?
Short naps (about 20–30 minutes) early in the afternoon can improve alertness without disturbing nighttime sleep. Long or late naps can disrupt your sleep schedule.
5: How can I stop my mind from racing at bedtime?
Relaxation techniques such as deep breathing, progressive muscle relaxation, meditation, and journaling can help calm the mind.
6: Is alcohol helpful for sleep?
While it may initially cause drowsiness, alcohol disrupts sleep cycles and reduces overall sleep quality.
7: What is the ideal bedroom temperature for sleep?
A cool environment, around 60–67°F (16–19°C), is optimal for promoting restful sleep.
8: Can certain foods help improve sleep?
Yes, foods containing melatonin, tryptophan, magnesium, or antioxidants, like tart cherries, kiwi, bananas, and almonds, can support better sleep.
9: Are natural sleep supplements safe and effective?
Supplements such as melatonin, magnesium, valerian root, or lavender can aid sleep for some people, but should be used under medical advice to avoid side effects or interactions.
10: What should I do if I can’t fall asleep after 20 minutes?
Get out of bed and engage in a calming, non-stimulating activity in dim light until you feel sleepy, then return to bed.
Reference
- Harvard Health Publishing: “Successful aging: 10 tips for better sleep” — https://www.health.harvard.edu/staying-healthy/successful-aging-10-tips-for-better-sleep
- UC Davis Health: “Try these 13 tips to help you sleep better” — https://health.ucdavis.edu/news/headlines/try-these-13-tips-to-help-you-sleep-better/2023/07
- Sleep Foundation: “The 20 ultimate tips for how to sleep better” — https://www.sleepfoundation.org/sleep-hygiene/healthy-sleep-tips
- Somnee (Dr. Matthew Walker): “10 Tips for Better Sleep” — https://somneesleep.com/blogs/post/matt-walker-sleep-tips
- American Academy of Sleep Medicine: “Improve your sleep in five simple steps” — https://sleepeducation.org/improve-your-sleep-in-five-simple-steps/
- National Center for Biotechnology Information (NCBI): “Sleep health promotion interventions and their effectiveness” — https://pmc.ncbi.nlm.nih.gov/articles/PMC8196727/
- Healthline: “Top 15 proven tips to sleep better at night” — https://www.healthline.com/nutrition/17-tips-to-sleep-better
- Mayo Clinic: “Sleep tips: 6 steps to better sleep” — https://www.mayoclinic.org/healthy-lifestyle/adult-health/in-depth/sleep/art-20048379
Eryn Ellison is a PharmD with 8 years in hospital and ambulatory care. A graduate of the UNC Eshelman School of Pharmacy (2017), Eryn completed a PGY-1 Pharmacy Residency at Cleveland Clinic and holds BCPS certification from the Board of Pharmacy Specialties. They evaluate supplement efficacy, safety, and interactions with common prescriptions. Eryn has authored formulary reviews for P&T committees and consults on deprescribing protocols within large health systems. Credentials: state pharmacist license, BCPS ID, and professional profiles.

