
Sleep health is essential for mental, emotional, and physical well-being. It relies on proper sleep cycles involving NREM and REM stages that restore the body and mind. Understanding sleep disorders their causes, diagnosis, and treatments is crucial for maintaining long-term health and daily functioning.
Key Takeaways
- Sleep quality directly impacts immunity, brain function, emotional stability, and heart health.
- Common disorders include insomnia, sleep apnea, narcolepsy, parasomnias, and restless leg syndrome.
- Major causes: genetics, medical and mental conditions, lifestyle factors, medications, and environment.
- Diagnosis uses tools like polysomnography, actigraphy, and sleep diaries to identify root issues.
- Evidence-based treatments include CBT-I, CPAP, medication, and lifestyle optimization.
- Consistent sleep schedules, stress management, and a healthy environment prevent most sleep disorders.
What is Sleep Health?
Getting enough good quality sleep is as important as eating healthy and exercising. Recent research shows a growing number of people aren’t sleeping well, affecting energy, mood, memory, and long-term health.
The Science of Sleep
Sleep is composed of multiple cycles that include two primary types: NREM (Non-Rapid Eye Movement) and REM (Rapid Eye Movement) sleep. These types serve distinct functions critical for brain and body recovery.
NREM sleep has three stages:
- Stage 1 (Light sleep): Transition from wakefulness to sleep, easy to awaken.
- Stage 2: Deeper sleep where body temperature and heart rate decrease, brain activity shows sleep spindles important for memory.
- Stage 3 (Deep sleep): Slow-wave sleep, crucial for physical restoration, tissue repair, and immune system strengthening.
REM sleep follows NREM stages
- It is characterized by rapid eye movements, active brain patterns similar to wakefulness, dreaming, and muscle paralysis. REM supports emotional regulation, memory consolidation, and learning.
- During a typical night, a person cycles through these stages 4 to 6 times, each cycle lasting about 90 to 110 minutes. Early cycles have more deep NREM sleep; later cycles increase REM duration.Circadian rhythms regulate this cycle, aligning sleep with environmental light and darkness by controlling hormone secretion such as melatonin.
How Much Sleep Do You Really Need?
There’s no single answer that fits everyone. Sleep needs change with age, lifestyle, and health.Some people may need more or less sleep due to genetics or personal health. What matters most: waking up feeling refreshed and alert through the day.
| Age Group | Recommended Sleep (Hours/Night) |
| Children (6–13) | 9–11 |
| Teens (14–17) | 8–10 |
| Adults (18–64) | 7–9 |
| Older adults (65+) | 7–8 |
Most Common Sleep Disorders
Sometimes, trouble while sleeping goes beyond bad habits. The major sleep problems are well-studied and treatable.

Insomnia
Insomnia is the most common sleep disorder. People with insomnia find it hard to fall asleep, stay asleep, or wake up too early and can’t get back to sleep. It can be short-term (due to stress or changes in routine) or chronic (lasting months or longer). Chronic insomnia can lead to daytime fatigue, irritability, trouble concentrating, and a higher risk of health problems like depression and high blood pressure.
Sleep Apnea
Sleep apnea causes repeated pauses in breathing during sleep, often followed by choking or gasping for air. The most common type, obstructive sleep apnea, happens when throat muscles relax and block the airway. People may not realize they wake up many times during the night, but they often feel tired, have headaches in the morning, or experience mood changes. Untreated sleep apnea raises the risk of heart disease, stroke, and high blood pressure.
Restless Leg Syndrome (RLS)
RLS is a strong urge to move the legs, usually due to uncomfortable sensations like tingling, crawling, or aching. Symptoms often get worse in the evening or at night, making it difficult to fall asleep or stay asleep. Moving the legs relieves the discomfort temporarily. RLS can cause chronic sleep loss and impact daytime energy and mood.
Narcolepsy
Narcolepsy is a neurological disorder that causes sudden, uncontrollable episodes of falling asleep during the day, sometimes even in the middle of activities. People may also experience cataplexy (sudden muscle weakness triggered by emotions), sleep paralysis, and vivid dreams. Narcolepsy can be very disruptive to daily life, but treatments are available to help manage symptoms.
Parasomnias
Parasomnias are unusual behaviors during sleep, such as sleepwalking, night terrors, talking, or eating while asleep. These events usually happen in children, but can also affect adults. While most parasomnias are not dangerous, some can lead to injury or disturbed sleep for others in the household. In many cases, children outgrow parasomnias as they get older.
Causes of Sleep Disorders
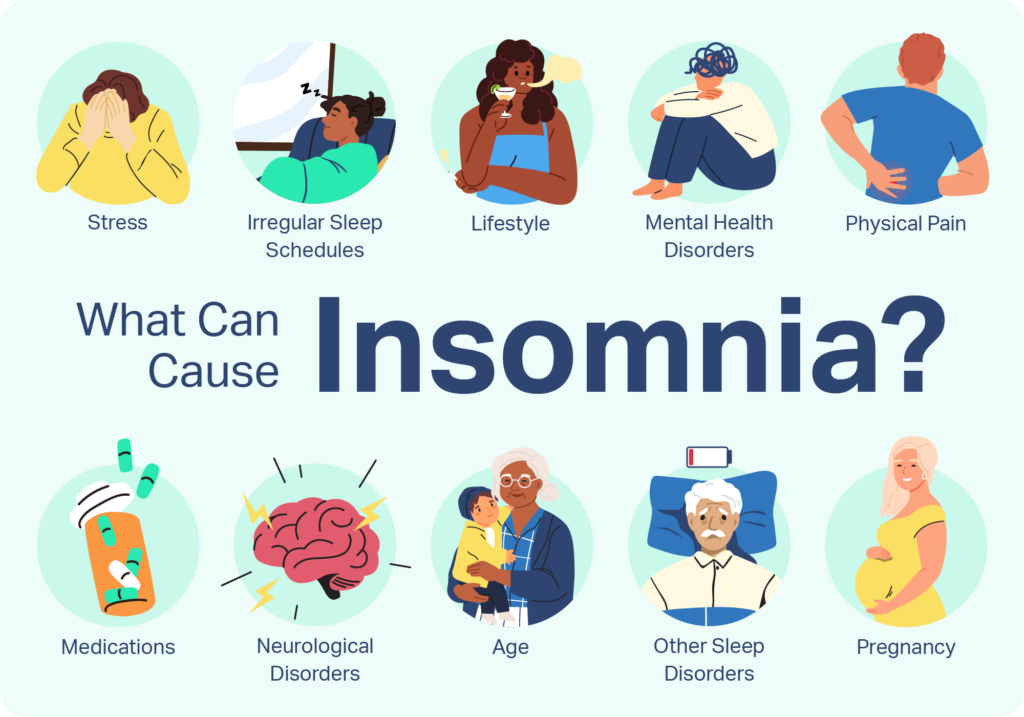
Sleep disorders can develop due to a combination of physical, psychological, and environmental factors. Underlying medical conditions, mental health issues, lifestyle habits, and even genetics can all play a role. In some cases, stress, shift work, or poor sleep environments contribute to ongoing sleep difficulties.
- Genetic Predisposition: Some sleep disorders are familial. Narcolepsy, restless leg syndrome, and specific forms of insomnia have documented genetic links. Family history increases risk, as shown in clinical studies of narcolepsy and insomnia cohorts.
- Age-Related Changes in Sleep Patterns: Older age is linked with lighter, fragmented sleep and reduced deep sleep. These changes increase susceptibility to insomnia and frequent waking. Aging alters circadian rhythms and lessens melatonin production, both supported by sleep research.
- Medical Conditions: Chronic diseases such as arthritis, asthma, COPD, heart failure, and neurological disorders (for example, Parkinson’s or Alzheimer’s disease) commonly disrupt sleep architecture. Pain, breathing difficulties, or abnormal movement during sleep are common mechanisms.
- Mental Health Issues: Anxiety and depression are strongly associated with sleep problems. Persistent stress raises cortisol, activating wakefulness. Psychiatric studies routinely find bi-directional links: sleep disorders increase mental health problems, and vice versa.
- Lifestyle Factors: Shift work, late-night screen use, inconsistent bed and wake times, insufficient exercise, and intake of caffeine or alcohol disrupt normal circadian cues and sleep cycles. Studies confirm these behaviors correlate with higher prevalence of insomnia.
- Environmental Factors: Exposure to noise, light pollution, high or low temperatures, and uncomfortable bedding or bedroom humidity can disrupt sleep continuity. Environmental sleep studies have clearly linked these variables to poorer sleep outcomes.
- Medications and Substances: Stimulants (e.g., some antidepressants, corticosteroids, beta-agonists), decongestants, and psychoactive drugs cause sleep-onset or maintenance problems. Nicotine, alcohol, and some recreational drugs likewise interfere with normal sleep architecture.
Sleep Disorder Diagnosis
Diagnosing sleep disorders involves a careful evaluation combining clinical history, physical exams, questionnaires, and specialized tests. The process aims to identify the specific type of sleep disorder and its underlying causes for effective treatment.
- Clinical Interview: The healthcare provider reviews the patient’s symptoms, medical history, and sleep habits. For reliable insights, input from a bed partner (if possible) is valuable, as they may notice snoring, gasping, limb movements, or unusual behaviors during sleep.
- Sleep Diary: Patients may be asked to keep a sleep log for 1–2 weeks, detailing sleep and wake times, waking events, naps, exercise, caffeine, and alcohol use. This gives the clinician an overview of patterns and potential triggers.
- Polysomnography: Conducted overnight in a sleep laboratory or at home (limited data for the latter). Sensors record several physiologic parameters. Essential for diagnosing complex disorders or when initial evaluations are inconclusive.
- Home Sleep Apnea Test: Portable devices to record breathing and oxygen levels at home. Used when obstructive sleep apnea is suspected and there are no other serious medical conditions.
- MSLT/MWT: Measure propensity for daytime sleepiness, diagnosis of narcolepsy, or assessment of fitness for occupations that require alertness (e.g., pilots).
- Actigraphy: Used for several days to weeks, especially for detecting circadian rhythm or insomnia issues.
- Other Laboratory Tests: Assess for underlying causes such as hypothyroidism, anemia, or substance use that can disrupt sleep
Physical Examination
A physical exam may reveal risk factors such as obesity (linked with sleep apnea), nasal obstruction, or neurological findings indicative of sleep-related movement disorders.
| Test Name | What It Measures | Most Common Uses |
| Polysomnography (PSG) | Brain waves, eye movements, muscle activity, heart rate, respiratory patterns, oxygen levels | Gold standard for diagnosing sleep apnea, narcolepsy, periodic limb movement disorder, parasomnias |
| Home Sleep Apnea Test | Breathing, oxygen levels, heart rate | Diagnosing obstructive sleep apnea (mild cases or high suspicion) |
| Actigraphy | Movement (usually wrist device) | Assessing sleep-wake cycles, circadian rhythm disorders |
| Multiple Sleep Latency Test (MSLT) | Time to fall asleep/enter REM during scheduled naps | Diagnosing narcolepsy and hypersomnia |
| Maintenance of Wakefulness Test (MWT) | Ability to remain awake under soporific conditions | Assessing daytime sleepiness in safety-sensitive roles |
| Overnight Oximetry | Oxygen saturation during sleep | Screen for sleep apnea, hypoventilation |
| Electroencephalogram (EEG), EMG, and EOG | Brain, muscle, and eye electrical activity | Identify seizures, confirm sleep stages as part of polysomnography |
| Laboratory Blood Tests | Thyroid, anemia, drug screens | Rule out medical contributors to sleep symptoms |
Sleep Disorder Treatments
Treatment options for sleep disorders are tailored to the specific condition, focusing on addressing symptoms, improving sleep quality, and enhancing overall well-being. Below are detailed explanations of the key approaches:
- Cognitive Behavioral Therapy for Insomnia (CBT-I): Structured therapy targets negative thoughts and behaviors about sleep. Uses techniques like sleep restriction, stimulus control, and relaxation. Proven in randomized trials as the first-line treatment for chronic insomnia, with durable results.
- Sleep Hygiene Improvements: Establishes regular sleep-wake times, limits screen time before bed, and creates a quiet, dark, and comfortable environment. Evidence supports improved sleep quality by reducing behavioral and environmental triggers.
- Medications: Prescribed according to disorder. Sedative-hypnotics or melatonin agonists for insomnia, stimulants for narcolepsy, and dopamine agonists or anticonvulsants for restless legs syndrome. Used short-term or with therapy, with close monitoring for side effects and dependency.
- Continuous Positive Airway Pressure (CPAP): Device delivers pressurized air via mask, keeping airways open for patients with obstructive sleep apnea. Multiple trials show CPAP improves sleep architecture, reduces daytime sleepiness, and lowers cardiovascular risks.
- Light Therapy: Timed exposure to bright light resets circadian rhythms. Used for delayed sleep phase disorder and seasonal affective disorder, with clinical trials showing benefit in improving sleep-timing and mood.
- Lifestyle Modifications: Regular exercise, management of stress with meditation or yoga, and avoiding caffeine/alcohol in the evening. Lifestyle changes are associated with better long-term outcomes in observational and interventional studies.
- Hypoglossal Nerve Stimulation: Implanted device stimulates tongue muscle via hypoglossal nerve to maintain airway for obstructive sleep apnea. Effective for patients who do not tolerate CPAP, supported by clinical trial data.
Impact of Sleep on Health & Well-being
Quality sleep is essential for maintaining and optimizing multiple vital systems in the body. Sleep affects immunity, mental health, cognitive function, and cardiometabolic health in distinct but interconnected ways.
1. Immunity
Sleep plays a critical role in strengthening the immune system. During sleep, the body produces and releases cytokines proteins that help fight infection and inflammation. Adequate sleep improves the body’s ability to respond to pathogens such as viruses and bacteria.
- Research Evidence: A 2020 clinical study showed individuals who slept fewer than 6 hours were significantly more likely to catch the common cold after exposure compared to those getting 7 or more hours.
- Sleep restores immune memory, improving how the body remembers and attacks previously encountered microbes.
- Poor or insufficient sleep suppresses immune function, leading to higher susceptibility to infections and slower recovery.
2. Mental Health
Good sleep is closely linked to emotional resilience and mental well-being.
- People with consistent, high-quality sleep report fewer symptoms of anxiety and depression.
- Sleep, particularly REM stages, supports emotional regulation by processing stress and traumatic memories.
- Disrupted sleep can increase emotional reactivity, worsen mood disorders, and is a risk factor for developing psychiatric conditions.
- The Lancet Psychiatry (2022) review confirmed that improving sleep can reduce symptoms of depression and anxiety, serving as a potential therapeutic target.
3. Memory and Cognitive Function
Deep sleep stages (mostly slow-wave sleep, NREM stage 3) are critical for memory consolidation, the process where the brain transfers short-term memories into stable long-term storage.
- During deep sleep, the brain clears out metabolic waste products facilitating neuroplasticity (brain cell communication).
- Lack of deep sleep is linked to impaired learning, concentration, and decision-making.
- REM sleep also plays a role in integrating emotional and procedural memories (like skills).
4. Heart and Metabolic Health
Poor or insufficient sleep disrupts multiple metabolic processes:
- Sleep deprivation affects hormone balance, increasing cortisol and altering appetite-regulating hormones (ghrelin increases hunger, leptin decreases satiety), contributing to weight gain.
- It also raises blood pressure, promotes inflammation, and impairs glucose metabolism, increasing the risk of insulin resistance and type 2 diabetes.
- Chronic inadequate sleep is a significant risk factor for cardiovascular diseases, including hypertension, coronary artery disease, and stroke.
- A 2023 meta-analysis confirmed that adults sleeping less than 6 hours per night have a 20–30% higher risk of cardiovascular events.
Sleep Disorder Prevention and Management
While not all sleep disorders can be prevented, certain lifestyle changes can improve sleep quality and significantly reduce the risk of developing sleep-related issues. Here’s how each measure helps.
- Maintaining a Consistent Sleep Schedule: Going to bed and waking up at the same time every day helps regulate your body’s internal clock, making it easier to fall asleep and wake up refreshed. This consistency is especially important for preventing circadian rhythm disorders.
- Creating a Relaxing Bedtime Routine: Engaging in calming activities like reading, meditation, or a warm bath signals your brain that it’s time to wind down. This routine prepares your mind and body for restful sleep and reduces insomnia symptoms.
- Optimizing the Sleep Environment: Keeping the bedroom quiet, dark, and cool, along with investing in a comfortable mattress and pillows, enhances sleep quality. A well-designed environment minimizes disturbances and promotes deeper sleep cycles.
- Limiting Exposure to Screens Before Bedtime: Blue light emitted by screens suppresses melatonin production, delaying sleep onset. Avoiding electronic devices an hour before bed helps reset your natural sleep-wake cycle.
- Managing Stress Through Relaxation Techniques: Practices such as yoga, deep breathing, and mindfulness reduce stress and anxiety, which are common contributors to sleep disturbances. Relaxation lowers cortisol levels, allowing the body to transition into sleep more easily.
- Avoiding Caffeine, Alcohol, and Heavy Meals Close to Bedtime: Stimulants like caffeine and alcohol disrupt sleep by interfering with natural sleep stages. Similarly, heavy meals can cause discomfort, keeping you awake longer.
- Regular Exercise (but Not Too Close to Bedtime): Physical activity promotes better sleep by reducing stress and increasing time spent in deep sleep stages. However, exercising too close to bedtime can elevate energy levels, making it harder to fall asleep.
Conclusion
Sleep disorders profoundly affect brain health, cognitive abilities, and overall physical and emotional well-being. Identifying and understanding different types of sleep disorders including insomnia, sleep apnea, parasomnias, and circadian rhythm disorders is critical to applying the correct treatments that target their root causes. Effective management requires a combination of approaches: working with healthcare providers, following evidence-based therapies, and making key lifestyle adjustments like maintaining consistent sleep schedules, managing stress, and creating an optimal sleep environment.
These steps help restore healthy sleep patterns, support mental clarity, emotional balance, and physical energy. Raising awareness of the causes and treatment options for sleep disorders not only benefits those directly affected but also emphasizes the essential role sleep plays in long-term health. Proactive care leads to better outcomes, reducing risks of cognitive decline, mood disorders, and chronic diseases while improving quality of life.
FAQs
- What is the most common sleep disorder?
Insomnia is the most common sleep disorder, affecting approximately 10–30% of adults. - Can sleep disorders be cured?
While some sleep disorders can be effectively managed or resolved, others may require ongoing treatment and lifestyle adjustments. - How much sleep do adults need?
Most adults need 7–9 hours of sleep per night, although individual needs may vary. - Are sleep disorders more common in certain age groups?
Sleep disorders can affect people of all ages, but some are more prevalent in specific age groups. For example, sleep apnea is more common in older adults. - Can stress cause sleep disorders?
Yes, stress can contribute to the development of sleep disorders, particularly insomnia. - Is snoring always a sign of sleep apnea?
While snoring is a common symptom of sleep apnea, not all snoring indicates sleep apnea. - Can diet affect sleep quality?
Yes, diet can impact sleep quality. Consuming caffeine, alcohol, or heavy meals close to bedtime can disrupt sleep. - Are sleep disorders hereditary?
Some sleep disorders, such as narcolepsy and restless legs syndrome, may have a genetic component. - Can exercise help with sleep disorders?
Regular exercise can improve sleep quality for many people, but it’s best to avoid vigorous exercise close to bedtime. - What is sleep hygiene?
Sleep hygiene refers to practices and habits that promote good sleep quality and quantity.
References
- Sleep Foundation. (2024, May 7). Sleep Disorders – Common Types, Symptoms, Treatments. Retrieved from https://www.sleepfoundation.org/sleep-disorders
- MercyOne. (2025, January 22). Top treatment options for sleep disorders. Retrieved from https://www.mercyone.org/newsroom/blog-articles/top-treatment-options-sleep-disorders
- Sprint Diagnostics. (n.d.). Sleep Disorders Causes, Types, and Solutions. Retrieved from https://www.sprintdiagnostics.in/blog/sleep-disorders-causes-types-and-solutions
- Aurora Health Care. (2024). Sleep Disorder Treatment. Retrieved from https://www.aurorahealthcare.org/services/sleep-disorders/treatment-options
- Care Insurance. (2024, November 22). Sleep Disorders: Types, Causes, Symptoms & Treatment. Retrieved from https://www.careinsurance.com/blog/health-insurance-articles/8-tips-to-make-sleep-disorders-ineffective
- American Family Physician. (2013, August 15). Management of Common Sleep Disorders. Retrieved from https://www.aafp.org/pubs/afp/issues/2013/0815/p231.html
- Healthline. (n.d.). Sleep Disorders: Causes, Diagnosis, and Treatments. Retrieved from https://www.healthline.com/health/sleep/disorders
- Cleveland Clinic. (n.d.). Sleep Disorders: Types, Causes, Symptoms & Treatment. Retrieved from https://my.clevelandclinic.org/health/articles/11429-sleep-disorders
Dr. Nathalia Estes is an ND trained at Accredited ND Program, Year, licensed in States With 10 years in integrative practice, she focuses on evidence guided botanicals, nutrient repletion, and lifestyle counseling. She has presented at conference and participated in quality-assurance reviews for herbal products. Verify licensure scope by state, see NPI, and review disclosures on affiliations and samples.

