Liver Cancer Awareness: Risk Factors, Prevention, and Early Detection

Liver cancer is one of the most preventable yet life-threatening cancers worldwide. It often develops silently over many years due to chronic infections, poor lifestyle habits, or long-term liver damage. With the right awareness, timely vaccinations, regular health screenings, and simple daily habits like maintaining a healthy weight and avoiding alcohol, most liver cancer cases can either be prevented or detected early when treatment is far more effective and survival chances are significantly higher.
Key Takeaways for Liver Cancer Prevention
- Hepatitis B vaccination is the strongest defense, preventing the majority of virus-linked liver cancers.
- Chronic infections (HBV and HCV), fatty liver disease, alcohol misuse, and obesity are the main risk factors.
- Regular liver screening every six months for at-risk people enables early, curable detection.
- Maintaining a healthy weight, limiting alcohol, and controlling diabetes protect the liver long term.
- Safe medical practices and food hygiene prevent viral and toxin exposure that trigger liver cancer.
- Early action, awareness, and consistent monitoring can save lives by catching disease before symptoms appear.
Why Awareness Matters

Awareness is the first step toward prevention and early detection. Many people develop liver cancer silently without symptoms until it is advanced, but understanding your risks and taking timely action can make all the difference.
Liver cancer is preventable in many cases through vaccination, healthy habits, and regular checkups. Recognizing this empowers people to protect themselves and their families.
Global Burden and Trends
Liver cancer ranks among the leading causes of cancer deaths globally. The disease accounts for about 75–85% of all primary liver cancers and affects millions of people each year.
- High-risk regions: East Asia, Sub-Saharan Africa, and parts of Latin America have the highest rates due to hepatitis B and aflatoxin exposure.
- Changing trends: In developed countries, viral hepatitis cases are declining, while fatty liver disease and alcohol-related liver damage are rising.
- Future projections: By 2050, non-viral causes like obesity and diabetes may become the main drivers of liver cancer.
How Liver Cancer Develops
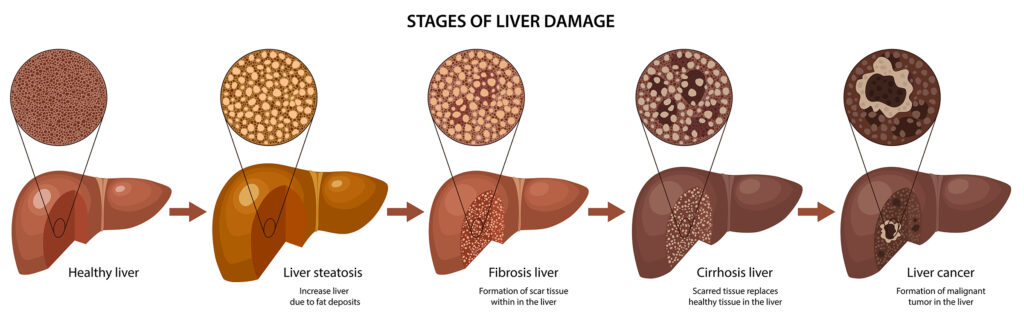
Liver cancer usually develops gradually over many years as a result of chronic liver injury and scarring. The process involves repeated cycles of liver cell damage, inflammation, and regeneration, which can eventually lead to cancerous changes in liver cells.
Chronic Liver Damage as the Starting Point
Liver cancer rarely occurs in a healthy liver. Most cases start in a liver that has been damaged over years. Common causes of chronic liver damage include:
- Hepatitis B and C infections: These viral infections can cause long-term inflammation, scarring, and eventually cirrhosis.
- Alcohol-related liver disease: Chronic heavy alcohol use damages liver cells, leading to cirrhosis.
- Non-alcoholic fatty liver disease (NAFLD): Fat accumulation in the liver, often linked to obesity and diabetes, can progress to inflammation and scarring.
Repeated liver injury triggers cycles of cell death and regeneration, increasing the risk of abnormal changes in liver cells.
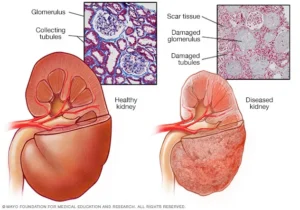
Cirrhosis: A Key Risk Factor
Cirrhosis is severe scarring of the liver tissue. It is the most common precursor to liver cancer.
- Scarred tissue disrupts normal liver function and creates a stressed environment for liver cells.
- Chronic regeneration of liver cells in cirrhosis increases the chances of genetic mutations, which may lead to cancerous growths.
Genetic and Cellular Mutations
As liver cells repeatedly repair themselves, DNA damage can accumulate:
- Mutations may cause uncontrolled cell growth.
- Some mutated cells evade normal mechanisms that prevent cancer development.
- Over time, clusters of these abnormal cells can form tumors.
Silent Progression
Liver cancer often grows without noticeable symptoms:
- Early-stage liver cancer may not cause pain or discomfort.
- Symptoms typically appear only after the tumor has grown large or spread, such as abdominal pain, jaundice, unexplained weight loss, or fatigue.
Tumor Growth and Spread
- Initially, cancer may stay localized in the liver.
- With time, it can invade nearby tissues or spread (metastasize) to other organs like the lungs or bones.
- Advanced liver cancer is harder to treat, which is why early detection in high-risk individuals is critical.
Other Contributing Factors
Certain lifestyle and environmental factors can accelerate liver cancer development:
- Exposure to aflatoxins (toxins in moldy food)
- Obesity, diabetes, and metabolic syndrome
- Smoking and unhealthy diets
Key Risk Factors of Liver Cancer
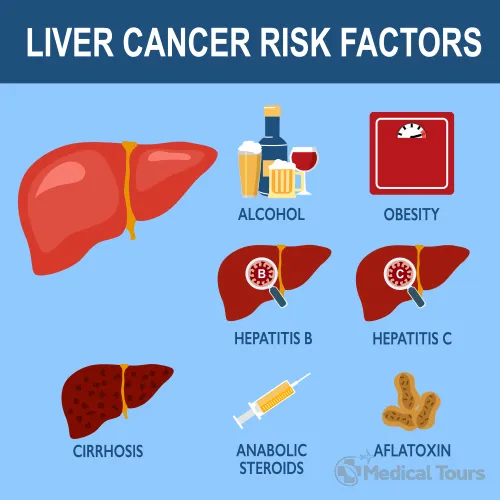
Several common and preventable conditions can raise your risk of liver cancer. Knowing them helps you take control of your health, make informed lifestyle choices, and take preventive medical steps. Each factor contributes differently, but many can be managed or avoided with awareness and timely care.
Chronic Hepatitis B Infection
Hepatitis B is one of the leading global causes of liver cancer. It can silently damage the liver for decades before symptoms appear. Early detection and treatment are key to reducing long-term complications.
Key points:
- People infected at birth or during childhood often develop chronic hepatitis B.
- The virus can remain in the body for life, even without visible symptoms.
- Continuous inflammation and scarring increase cancer risk over time.
- Regular monitoring and antiviral medicines can lower the chance of liver cancer significantly.
- Hepatitis B vaccination is the best preventive measure.
Chronic Hepatitis C Infection
Hepatitis C is a bloodborne virus that can persist for many years before causing visible liver damage. Although modern treatment cures most infections, the risk of liver cancer remains in people who already have scarring.
Key points:
- Infection often occurs through unscreened blood transfusions, needle sharing, or unsafe medical practices.
- People infected before the 1990s may still carry the virus unknowingly.
- New antiviral treatments can completely cure hepatitis C in a few months.
- Even after cure, those with cirrhosis or severe fibrosis must continue regular liver checks.
Cirrhosis
Cirrhosis is advanced liver scarring that disrupts normal liver structure and function. Once cirrhosis develops, the risk of liver cancer increases sharply regardless of its cause.
Key points:
- Caused by chronic hepatitis, alcohol misuse, or fatty liver disease.
- Creates an environment where cancer cells can form more easily.
- Requires lifelong monitoring and regular imaging for early tumor detection.
Metabolic Liver Disease (MASLD / MASH)
Metabolic dysfunction–associated liver disease is now one of the fastest-growing causes of liver cancer worldwide. It is closely linked to obesity and diabetes.
Key points:
- Results from excess fat buildup in the liver due to poor diet or inactivity.
- Can progress from simple fat accumulation to inflammation (MASH) and fibrosis.
- In some cases, liver cancer can develop even without cirrhosis.
- Weight loss, exercise, and better metabolic control lower risk dramatically.
Heavy Alcohol Use
Chronic and heavy drinking damages liver cells and promotes cirrhosis. When combined with other risk factors, alcohol multiplies the chances of liver cancer.
Key points:
- Long-term intake exceeding safe limits causes inflammation and scarring.
- Alcohol-related liver disease often progresses silently.
- Stopping alcohol use can halt or reverse early liver damage.
- People with hepatitis or fatty liver should avoid alcohol completely.
Aflatoxin Exposure
Aflatoxins are toxins produced by certain molds that grow on food crops stored in warm, damp conditions. Long-term exposure can lead to liver cancer, especially when combined with hepatitis B.
Key points:
- Commonly found in contaminated peanuts, maize, and grains.
- Risk is higher in tropical regions with poor food storage.
- Drying crops properly and keeping food away from moisture helps prevent contamination.
- Food safety regulations and awareness reduce community exposure.
Diabetes and Obesity
Both diabetes and obesity contribute to chronic inflammation and fat buildup in the liver, which promote cancer formation.
Key points:
- Insulin resistance causes metabolic changes that injure liver cells.
- Obese individuals often have overlapping fatty liver disease.
- Maintaining healthy weight, diet, and blood sugar helps lower the risk.
Genetic and Rare Disorders
Some inherited metabolic disorders can overload the liver with iron, copper, or abnormal proteins, leading to damage and eventual cancer.
Key points:
- Includes hemochromatosis, Wilson’s disease, and alpha-1 antitrypsin deficiency.
- Early diagnosis through blood tests or genetic screening can prevent complications.
- Regular follow-up and targeted treatment protect liver health.
Smoking and Chemical Exposure
Tobacco and environmental toxins also play a role in liver cancer by adding chemical stress to the liver.
Key points:
- Smoking increases oxidative stress and DNA mutations in liver cells.
- Exposure to arsenic in water or long-term anabolic steroid use raises risk.
- Avoiding tobacco and limiting toxin exposure helps protect the liver.
Family History and Demographics
Certain demographic and genetic factors influence how the liver responds to injury and disease.
Key points:
- Men and older adults face higher risk compared to women and younger individuals.
- Family history of liver cancer indicates possible inherited vulnerability.
- Regular checkups are essential for those with combined lifestyle and family risks.
Immunosuppression and Co-Infections
People with weakened immune systems or multiple viral infections require special attention.
Key points:
- HIV infection, organ transplants, or long-term immune-suppressing therapy increase cancer risk.
- Co-infection with hepatitis viruses speeds up liver injury.
- Regular medical follow-up and early antiviral treatment are critical.
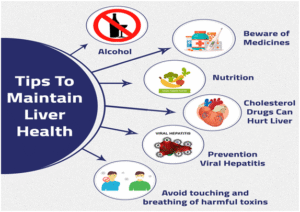
How to Reduce Risk (Primary Prevention) of Liver Cancer
Preventing liver cancer begins with tackling its main causes. Small but consistent lifestyle and medical steps can drastically reduce the chances of liver damage and cancer over time.
Hepatitis B Vaccination
The hepatitis B vaccine is the strongest tool against liver cancer. It prevents infection before it starts and offers long-term protection for both children and adults.
Main points:
- The first dose should be given within 24 hours of birth, followed by full vaccination.
- Unvaccinated children and adults can receive catch-up doses at any age.
- Vaccination also protects family members and healthcare workers exposed to blood.
Screening and Treatment for HBV
Early detection and treatment of hepatitis B help prevent liver scarring and cancer. Regular checkups are essential for those at risk.
Main points:
- Simple blood tests identify chronic infection.
- Antiviral medicines can suppress the virus and lower cancer risk.
- Regular monitoring helps catch liver damage early.
Screening and Cure of HCV
Hepatitis C is now curable with modern medicines. Testing and early treatment can stop further liver damage.
Main points:
- People who had transfusions before 1992 or shared needles should get tested.
- New antiviral drugs cure over 95% of cases in a few weeks.
- Those with prior liver damage still need follow-up care.
Manage Metabolic Health
Good metabolic health protects your liver from fatty buildup and inflammation. Lifestyle changes can make a major difference.
Main points:
- Maintain a healthy weight through balanced diet and regular activity.
- Control blood sugar and cholesterol levels.
- Even a small amount of weight loss improves liver function.
Limit Alcohol Consumption
Alcohol is a major cause of liver disease and cancer when used excessively. Reducing or quitting protects liver cells from further injury.
Main points:
- Avoid binge drinking and stick to recommended limits.
- People with hepatitis or liver disease should not drink at all.
- Seek professional help if quitting feels difficult.
Control Aflatoxin Exposure
Aflatoxins are harmful toxins found in moldy foods. Proper food handling can eliminate this hidden risk.
Main points:
- Keep grains, nuts, and cereals dry and mold-free.
- Avoid eating discolored or spoiled food.
- Store crops in clean, well-ventilated areas.
Safe Medical and Sexual Practices
Simple precautions can prevent infections that lead to liver damage. Protecting yourself and others reduces long-term risks.
Main points:
- Use sterile needles and screened blood for medical procedures.
- Practice safe sex and avoid sharing razors or toothbrushes.
- Healthcare workers should stay vaccinated and follow safety protocols.
Early Detection and Surveillance (Secondary Prevention)
Detecting liver cancer early can transform outcomes. Surveillance focuses on high-risk people to find small, treatable tumors before symptoms appear.
- Who needs it: People with cirrhosis from any cause and those with chronic hepatitis B at high risk.
- How it’s done: Liver ultrasound with or without a blood test (AFP) every six months.
- Why six months: Tumors can grow quickly, and this interval catches them early enough for treatment.
If ultrasound is unclear or suspicious, doctors may recommend contrast CT or MRI scans. Radiology reports may use LI-RADS categories to describe how likely a lesion is cancer.
In some cases, advanced blood markers like AFP-L3 and DCP can help, but ultrasound remains the foundation.
Surveillance saves lives, but only if followed consistently. Missing appointments or tests can allow cancers to progress silently.
Symptoms That Deserve Evaluation
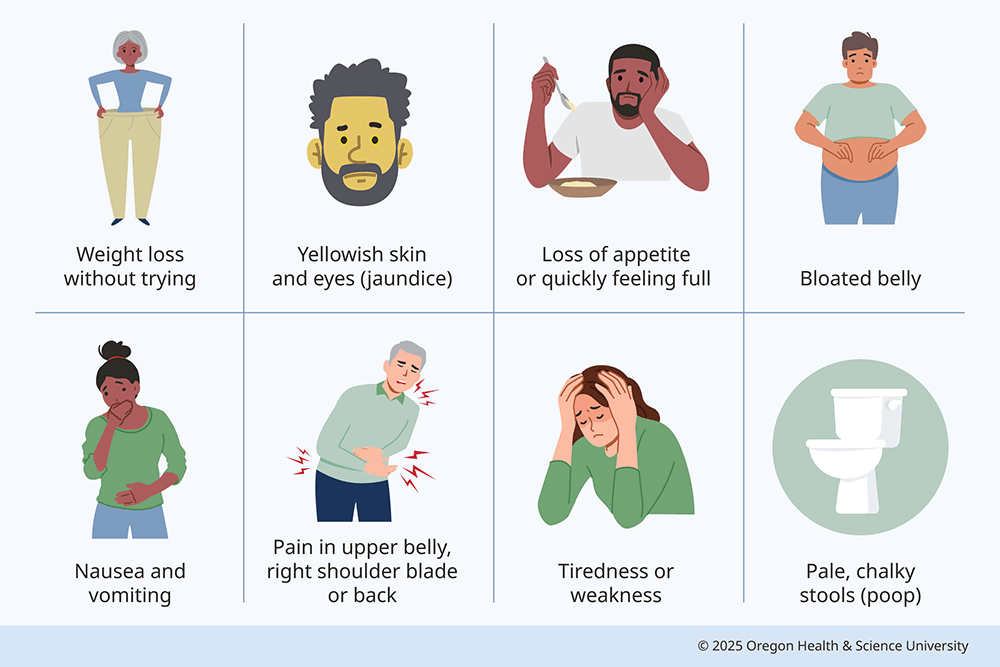
Liver cancer often develops quietly, showing little to no symptoms in its early stages. However, when signs do appear, they usually signal that the liver is already under significant stress. Recognizing these symptoms early and seeking medical help can make a critical difference in treatment outcomes.
- Unexplained weight loss or loss of appetite: The body may start using more energy to fight the disease, or the liver’s impaired function can affect digestion and metabolism.
- Persistent right upper abdominal pain: The liver is located on the right side under the ribs. Pain here can indicate swelling, inflammation, or tumor growth.
- Yellowing of skin or eyes (jaundice): This happens when the liver cannot properly process bilirubin, a substance created during the breakdown of red blood cells. Jaundice is often a clear sign of liver dysfunction.
- Swelling of the abdomen or legs: Fluid buildup (ascites in the abdomen or edema in the legs) can occur because the liver isn’t regulating proteins and fluids properly.
- Fatigue, nausea, or sudden worsening in someone with liver disease: The liver is key in energy metabolism and detoxification. When it’s stressed, it can lead to general weakness, nausea, or worsening of pre-existing liver conditions.
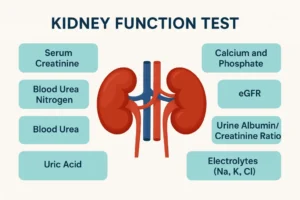
Diagnostic Approach and Staging Overview
Once an abnormality is found, doctors confirm it with specialized tests and imaging. These steps help determine the stage and best treatment.
- Blood tests: Liver enzymes, AFP, viral markers, and clotting profiles.
- Imaging tests: CT or MRI with contrast helps visualize the tumor precisely.
- Diagnosis without biopsy: In high-risk individuals, certain imaging findings can confirm cancer without biopsy.
- Staging: The BCLC system classifies the cancer by size, liver function, and health status to plan treatment.
Questions to Ask Your Healthcare Provider
Having an open and informed discussion with your doctor helps you take control of your health. Knowing the right questions ensures you understand your risks, treatment options, and the steps needed to protect your liver in the long run. Bring these points up during your next visit for a clearer, personalized plan.
- Am I at risk for liver cancer, and do I need surveillance?
- If I have hepatitis or fatty liver, what treatments are best for me?
- How often should I get ultrasounds or blood tests?
- What happens if a lesion is found?
- What lifestyle habits will help protect my liver?
Common Myths Corrected
Many myths about liver cancer prevent people from taking the right steps. Knowing the facts can save lives.
| Myth | Fact |
| Only heavy drinkers get liver cancer | Viral infections, obesity, metabolic disorders, and genetic conditions are also major causes of liver cancer. |
| A cured hepatitis C infection means zero risk | People who had cirrhosis before being cured still need lifelong monitoring, as their cancer risk remains. |
| Screening once a year is enough | Experts recommend screening every six months for those at high risk to catch tumors at an early, treatable stage. |
| Blood tests alone can detect it | Imaging, such as ultrasound or MRI, is essential for accurate detection; blood tests support but cannot replace imaging. |
Trusted Sources for More Information
Always refer to reliable, evidence-based organizations for guidance and updates:
- American Association for the Study of Liver Diseases (AASLD)
- European Association for the Study of the Liver (EASL)
- National Cancer Institute (NCI)
- National immunization programs and public health portals in your country
Conclusion
Liver cancer remains a major global health challenge, but it is largely preventable through awareness, vaccination, and lifestyle changes. Regular screening for those at risk, early treatment of hepatitis B and C, maintaining a healthy weight, and avoiding excessive alcohol use are crucial to protecting liver health. Recognizing early warning signs and acting promptly can greatly improve survival rates. Prevention begins with informed choices—vaccinate children, practice safe medical and sexual habits, eat safely stored food, and get regular checkups. With consistent vigilance and responsible health practices, liver cancer can be reduced significantly. Awareness, early detection, and prevention together form the strongest shield against this deadly yet avoidable disease.
FAQs
- Who should get liver cancer screening every six months?
People with cirrhosis or chronic hepatitis B with risk factors should have an ultrasound and AFP test every six months. Regular screening helps detect cancer early when treatment works best. - Does curing hepatitis C eliminate my cancer risk?
Not completely. Treatment greatly lowers risk, but if you already have liver scarring or cirrhosis, ongoing surveillance remains essential. - Is ultrasound alone enough for screening?
Ultrasound is the main and most effective tool for detecting liver tumors. Adding AFP blood tests can sometimes improve early detection accuracy. - Can obesity or fatty liver cause cancer even without cirrhosis?
Yes. In metabolic liver disease, cancer can occasionally develop before cirrhosis forms, especially when insulin resistance and inflammation persist. - How effective is the hepatitis B vaccine in prevention?
Extremely effective it prevents over 90% of chronic infections, dramatically lowering the lifetime risk of liver cancer. - Are new blood tests like AFP-L3 or DCP more accurate?
They can enhance accuracy when combined with ultrasound but are not reliable as standalone screening tools. - What does LI-RADS mean on my scan report?
LI-RADS is a system radiologists use to classify liver lesions by cancer risk, helping doctors decide on follow-up or further testing. - Do I still need screening if I’m cured of hepatitis C?
Yes, if you had cirrhosis before being cured. Regular surveillance should continue indefinitely to detect any new cancer early. - How dangerous is aflatoxin exposure?
Very dangerous, it’s a potent toxin that can damage liver DNA and trigger cancer. Safe food storage and avoiding moldy grains reduce risk. - Which lifestyle changes most effectively lower risk?
Avoid alcohol, maintain a healthy weight, eat a balanced diet, and stay vaccinated against hepatitis B to protect your liver long-term.
Reference
- American Cancer Society – Liver Cancer Risk Factors
This page outlines the primary risk factors for liver cancer, including chronic hepatitis B and C infections, cirrhosis, and other conditions.
https://www.cancer.org/cancer/types/liver-cancer/causes-risks-prevention/risk-factors.html - UT Southwestern – Liver Cancer Awareness and Prevention
UT Southwestern Medical Center offers patient education on liver cancer awareness and prevention, emphasizing the importance of regular screenings for those at high risk.
https://utswmed.org/conditions-treatments/liver-cancer/liver-cancer-awareness-and-prevention/ - Prevent Cancer Foundation – Liver Cancer Prevention and Screening
This foundation offers guidance on liver cancer prevention and screening, including vaccination recommendations and lifestyle modifications. https://preventcancer.org/preventable-cancer/liver-cancer/
Dr. Nathalia Estes is an ND trained at Accredited ND Program, Year, licensed in States With 10 years in integrative practice, she focuses on evidence guided botanicals, nutrient repletion, and lifestyle counseling. She has presented at conference and participated in quality-assurance reviews for herbal products. Verify licensure scope by state, see NPI, and review disclosures on affiliations and samples.