A heart attack is caused by blocked blood flow damaging heart muscle, while a cardiac arrest results from sudden electrical failure stopping the heart. Prompt recognition and treatment of these different emergencies save lives.
Key takeaways
- Heart attack results from blocked arteries reducing oxygen to the heart muscle.
- Cardiac arrest stems from electrical malfunction causing sudden heart stoppage.
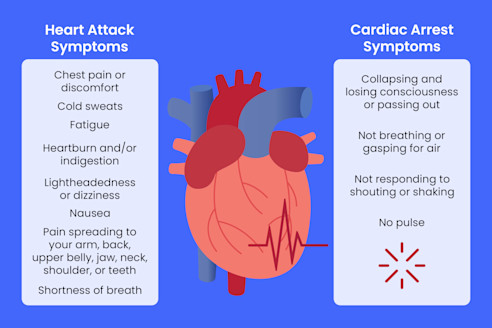
- Symptoms for heart attack include chest pain, discomfort, and shortness of breath; cardiac arrest causes sudden collapse and no pulse.
- Initial treatment for heart attack involves restoring blood flow, while cardiac arrest requires CPR and defibrillation.
- Risk factors for both include smoking, hypertension, diabetes, and family history.
- Prevention focuses on healthy lifestyle changes, medication adherence, and use of implantable defibrillators for high risk.
Understanding Heart Attack and Cardiac Arrest
A heart attack and a cardiac arrest are both critical cardiac emergencies but are very different in cause and outcome. A heart attack involves a problem with blood flow to the heart muscle, while a cardiac arrest involves an electrical failure of the heart. Knowing these distinctions helps in recognizing symptoms quickly and acting decisively to save lives.
Comparative Overview On Heart Attack and Cardiac Arrest
The main difference lies in what happens inside the heart. A heart attack occurs when a blocked artery limits blood supply to part of the heart muscle, causing damage. Cardiac arrest happens when the heart suddenly stops beating due to an electrical malfunction, stopping blood flow to vital organs.
| Feature | Heart Attack | Cardiac Arrest |
| Cause | Blood flow blockage in heart arteries | Electrical disruption causing heart to stop |
| Onset | Gradual or sudden | Sudden, without warning |
| Symptoms | Chest pain, discomfort, shortness of breath | Sudden collapse, no pulse, unconsciousness |
| Immediate Treatment | Medications, angioplasty | CPR, defibrillation |
| Survival without help | Minutes to hours | Seconds to minutes |
Causes and Risk Factors Of Heart Attack

Heart attacks happen mainly due to a blockage in the coronary arteries caused by fatty deposits or blood clots. This blockage limits blood flow to the heart muscle, causing damage. Several factors increase the risk of developing a heart attack:
- High cholesterol: Excess cholesterol builds up in artery walls, forming plaques that narrow arteries and reduce blood flow.
- Smoking: Toxins in cigarettes damage blood vessels, increase clot formation, and reduce oxygen in the blood.
- High blood pressure (Hypertension): Elevated pressure damages artery walls, making them more susceptible to plaque buildup.
- Diabetes: High blood sugar levels damage blood vessels and increase the likelihood of artery plaque formation.
- Sedentary lifestyle: Lack of physical activity contributes to obesity, high blood pressure, and poor cholesterol levels.
- Obesity: Excess body fat strains the heart and negatively affects cholesterol, blood pressure, and blood sugar.
- Family history: A close relative with heart disease increases your genetic risk for heart attacks.
- Stress: Chronic stress raises blood pressure and triggers harmful behaviors like smoking or overeating.
- Unhealthy diet: Diets high in saturated fat, trans fats, and refined sugars promote arterial plaque build-up.
- Age and gender: Risk increases with age, and men are generally at higher risk earlier than women.
Symptoms: Recognizing a Heart Attack
Recognizing a heart attack quickly is vital for timely treatment. The most common symptom is chest pain or discomfort, often described in the following ways:
- Pressure, fullness, or squeezing sensation in the center of the chest
- Pain or discomfort that lasts for several minutes or comes and goes
- Pain or discomfort radiating to the arms, especially the left arm
- Jaw pain or discomfort
- Pain in the back or stomach area
- Shortness of breath, which can occur with or without chest discomfort
- Nausea or vomiting
- Lightheadedness or dizziness
- Cold sweat or clammy skin
Immediate Response and What to Do
When heart attack symptoms appear, fast action can save a life. Follow these steps immediately:
- Call emergency services right away: Do not wait or try to drive yourself to the hospital. Professional medical help is critical.
- Have the person sit down and rest: Keep them calm and comfortable to reduce the heart’s workload.
- Give aspirin if appropriate: If the person is not allergic and is conscious, have them chew a regular-strength aspirin (usually 325 mg). This helps thin the blood and may reduce clot formation.
- Avoid physical exertion: Do not let the person walk, stand, or perform any strenuous activity.
- Do not offer food or drink: Unless instructed by medical responders, avoid giving anything to eat or drink as it might complicate treatment later.
- Stay with the person until help arrives: Monitor their condition, be ready to provide CPR if they lose consciousness or stop breathing.
Long-Term Management and Prevention
Post-heart attack care focuses on lifestyle modification, including a healthy diet, regular exercise, quitting smoking, and controlling blood pressure and diabetes. Medication adherence and regular follow-ups are essential for preventing recurrence.
What Is Cardiac Arrest?

Cardiac arrest is when the heart suddenly stops beating effectively, cutting off blood flow to the brain and organs. It often occurs without warning and requires immediate action. Without treatment, death can occur within minutes.
Causes and Risk Factors of Cardiac Arrest
Cardiac arrest occurs when the heart suddenly stops pumping blood due to an electrical disturbance disrupting its rhythm. The primary causes and risk factors include:
- Arrhythmias (Irregular Heart Rhythms): The most common cause is ventricular fibrillation, where the heart’s electrical signals become erratic, preventing effective beating.
- Heart Disease: Coronary artery disease or previous heart attacks increase the risk by damaging the heart muscle or its electrical system.
- Cardiomyopathy: Disease of the heart muscle that weakens its ability to pump and may trigger dangerous arrhythmias.
- Electrical Abnormalities: Inherited or acquired conditions like Long QT syndrome or Brugada syndrome disrupt normal heart rhythm.
- Severe Trauma: Injuries to the chest or major blood loss can cause cardiac arrest.
- Drowning or Asphyxiation: Oxygen deprivation rapidly leads to heart stoppage.
- Drug Overdose or Poisoning: Certain drugs or toxins can interfere with heart rhythm or depress heart function.
Symptoms and Warning Signs
Cardiac arrest is sudden and often unexpected. The key signs that someone is experiencing cardiac arrest include:
- Sudden collapse: The person may fall or slump to the ground without warning.
- Loss of consciousness: They become unresponsive and do not wake up when shaken or spoken to.
- No detectable heartbeat or pulse: The heart stops beating effectively, so there is no pulse.
- No breathing or abnormal breathing: The person either stops breathing entirely or takes only gasping breaths.
Prevention Strategies
Preventing cardiac arrest focuses on managing risk factors and early intervention for those at high risk. Key prevention strategies include:
- Implantable Cardioverter Defibrillators (ICD): For individuals with known serious arrhythmias or previous cardiac arrest, ICD devices monitor heart rhythm and deliver shocks to restore normal heartbeat if dangerous arrhythmias occur.
- Managing Underlying Heart Conditions: Control of coronary artery disease, heart failure, and cardiomyopathy through medication and lifestyle changes reduces risk.
- Avoiding Triggers: Limiting stimulants like excessive caffeine, managing stress, and avoiding illicit drugs or medications that affect heart rhythm help prevent arrhythmias.
- Regular Health Screenings: Routine cardiac check-ups and monitoring of blood pressure, cholesterol, and diabetes facilitate early detection and treatment.
- Healthy Lifestyle Choices: A balanced diet, regular exercise, quitting smoking, and maintaining a healthy weight are fundamental in reducing overall cardiac risk.
Heart Attack vs Cardiac Arrest: Key Differences
Understanding the key differences between a heart attack and cardiac arrest is essential for effective response and treatment. Here is how they differ:
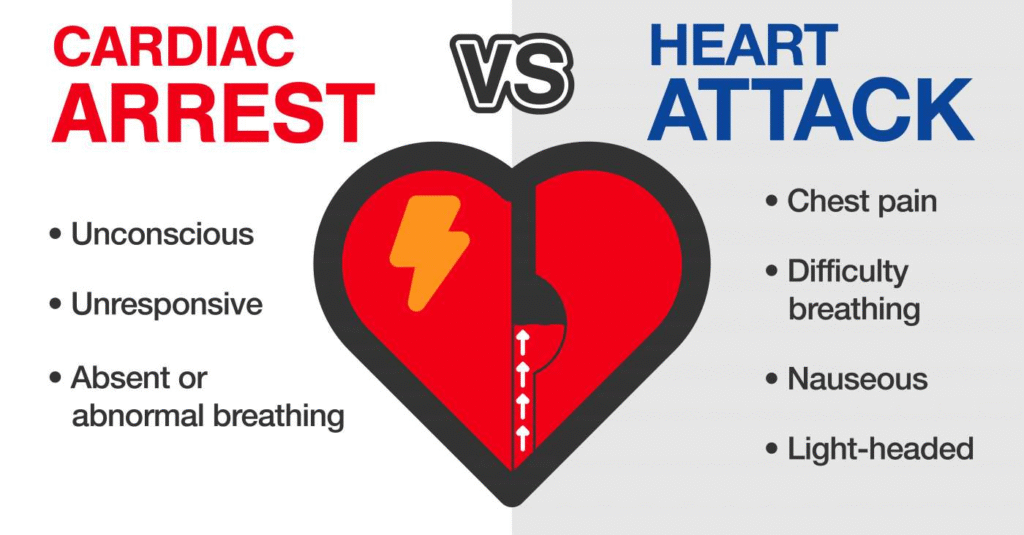
- Cause: Heart attack occurs due to a blockage in the blood vessels supplying the heart muscle, leading to damage or death of heart tissue. Cardiac arrest happens because of an electrical malfunction that causes the heart to stop beating suddenly.
- Onset and Symptoms: Heart attacks often have warning signs such as chest pain, discomfort, or shortness of breath. Cardiac arrest typically strikes without warning, causing immediate collapse and loss of consciousness.
- Impact on Heart Function: During a heart attack, the heart usually continues to beat, though less effectively, while cardiac arrest stops the heart entirely from pumping blood.
- Immediate Treatment: Heart attack treatment focuses on restoring blood flow through medication or surgery. Cardiac arrest requires immediate CPR and defibrillation to restart the heart.
- Relationship: If a heart attack causes severe damage or disrupts the heart’s electrical system, it can trigger cardiac arrest. Early recognition and treatment of a heart attack help prevent this progression.
At-Risk Groups
Certain groups of people are more vulnerable to heart attacks and cardiac arrests due to underlying health conditions and lifestyle factors. These include:
- Older Adults: Risk increases with age as arteries harden and heart function may decline.
- People with Existing Heart Problems: Those with coronary artery disease, heart failure, or previous heart attacks face higher risk.
- Individuals with Hypertension (High Blood Pressure): Persistent high blood pressure damages arteries and the heart over time.
- People with Obesity: Excess weight strains the heart and contributes to other risk factors like diabetes.
- Diabetics: High blood sugar levels damage blood vessels and increase cardiovascular risks.
- Smokers: Tobacco use significantly raises the risk of artery damage, blood clots, and arrhythmias.
- Family History of Heart Disease: Genetic factors play a strong role in predisposition to heart conditions.
- Men: Generally at greater risk and tend to experience heart attacks earlier than women.
- Women: Have unique symptoms and risk factors, including hormonal influences and higher risk post-menopause.
Latest Research and Advances
Advances in heart care have transformed prevention and treatment, boosting survival rates and recovery. Some key developments include:
- Improved clot-busting medications: New drugs dissolve clots faster and with fewer side effects, reducing heart muscle damage during heart attacks.
- Advanced stenting and angioplasty techniques: Modern procedures quickly open blocked arteries with less risk and shorter recovery times.
- Wearable heart monitors: Compact devices track heart rhythms and detect problems early, helping at-risk patients manage their condition.
- Smarter defibrillators: Next-generation devices deliver precise shocks and provide easier guidance for rescuers during cardiac arrest.
- Community CPR training initiatives: Widespread training empowers more people to respond quickly to emergencies, increasing survival rates.
- Cooling therapies (therapeutic hypothermia): After cardiac arrest, medically managed cooling protects the brain and improves chances of meaningful recovery.
Real Cases and Patient Stories
Stories from real patients and families highlight how fast, correct action makes a difference.
- People who received immediate CPR and defibrillation after cardiac arrest survived and made strong recoveries, emphasizing the importance of public readiness.
- Heart attack survivors describe how adopting healthier habits such as quitting smoking, eating better, and regular exercise helped them avoid future heart problems.
- Families who recognized unusual symptoms, especially in women and older adults, called for help sooner and achieved better outcomes.
Conclusion
Heart attacks and cardiac arrests are serious heart emergencies with different causes. A heart attack is caused by blocked arteries reducing blood flow to the heart muscle, resulting in chest pain and discomfort. Cardiac arrest occurs due to sudden electrical failure stopping the heartbeat, causing immediate collapse and loss of pulse.
Heart attacks need medications or surgery, while cardiac arrest requires CPR and defibrillation. Risk factors include smoking, high blood pressure, and diabetes. Prevention involves healthy living and medical devices like implantable defibrillators. Quick recognition and treatment drastically improve survival chances for both.
FAQs
What is the main difference between a heart attack and cardiac arrest?
Heart attack is a blocked artery causing heart muscle damage; cardiac arrest is sudden heart stoppage due to electrical failure.
What are early warning signs of a heart attack?
Chest pain, discomfort, shortness of breath, nausea, pain in jaw or arms.
Can a heart attack be silent?
Yes, some experience no clear symptoms, especially women and diabetics.
What should I do if someone is having a heart attack?
Call emergency services immediately, keep the person calm, and give aspirin if safe.
How is a heart attack diagnosed?
Through ECG, blood tests for enzymes, and imaging.
How is cardiac arrest diagnosed?
By absence of pulse and ECG during resuscitation.
Who should learn CPR and AED?
Everyone, especially families of high-risk individuals and public workers.
What is the survival rate outside hospital?
Low but improves dramatically with quick CPR and defibrillation.
What are long-term effects after cardiac arrest?
Possible brain injury, cognitive issues, physical limitations.
How are high-risk groups protected?
Implantable defibrillators and regular cardiac monitoring.
How can families support survivors?
Through rehabilitation support, lifestyle encouragement, and emotional care.
Reference
- British Heart Foundation: Difference between cardiac arrest and heart attack
- MSD Manuals: What’s the difference between a heart attack and cardiac arrest?
- StatPearls (NCBI): Cardiac Arrest – Clinical overview
- Healthline: Difference between a heart attack and a cardiac arrest
- BYJU’S Biology: Key differences between heart attack & cardiac arrest
- American Heart Association: Heart attack vs cardiac arrest — key differences
- Mayo Clinic: Heart attack symptoms & causes
- Medical News Today: Heart attack symptoms, treatment, and causes
- Cleveland Clinic: Sudden Cardiac Arrest: Causes & Symptoms
- CDC: About heart attack symptoms, risk, and recovery
Autum Harkins is a CNS with an MS in Clinical Nutrition from Maryland University of Integrative Health (2017) and 8 years in integrative clinics. She develops individualized protocols for deficiencies, digestive health, and women’s wellness, prioritizing third-party-tested supplements. Autum contributes to case series and webinars and mentors practitioners on lab interpretation. Credentials: CNS Board (ANA/BCNS) number, state nutrition licensure where applicable, and professional memberships with links.

