Chronic Kidney Disease (CKD): Stages, Symptoms & Treatment
Chronic Kidney Disease (CKD) is a long-term condition where kidneys gradually lose their ability to filter waste and maintain essential body functions. It progresses silently, leading to complications like kidney failure, heart disease, and high blood pressure if untreated.
Key Takeaways
- CKD is staged using eGFR (kidney filtration rate) and albuminuria (protein in urine) levels.
- Major causes include diabetes, high blood pressure, glomerular and genetic diseases.
- Early stages often show no symptoms; fatigue, swelling, and nausea appear as it advances.
- Early screening in high-risk groups (diabetes, hypertension) prevents severe complications.
- Treatment focuses on blood pressure control, sugar management, and kidney-protective drugs (ACE inhibitors, SGLT2 inhibitors).
- Healthy diet, low salt intake, and avoiding nephrotoxic drugs are vital for slowing progression.
What is Chronic Kidney Disease and Why It Matters
Your kidneys are vital organs that filter waste and extra fluid from the blood, support blood pressure, keep bones healthy and more. When kidney function is reduced over a long time, that’s chronic kidney disease (CKD). It matters because CKD often has few early symptoms, can progress silently, and leads to serious health issues like kidney failure, high blood pressure, heart disease, bone problems and more.
How Kidneys Work
Your kidneys perform several key jobs:
- They filter the blood to remove waste and extra fluid, producing urine.
- They regulate electrolyte levels (like potassium and sodium).
- They help control blood pressure via hormones like renin.
- They help make active vitamin D and manage bone-mineral balance. Because of these many roles, damage to kidneys causes ripple effects across the body.
Staging Chronic Kidney Disease (CKD) Precisely
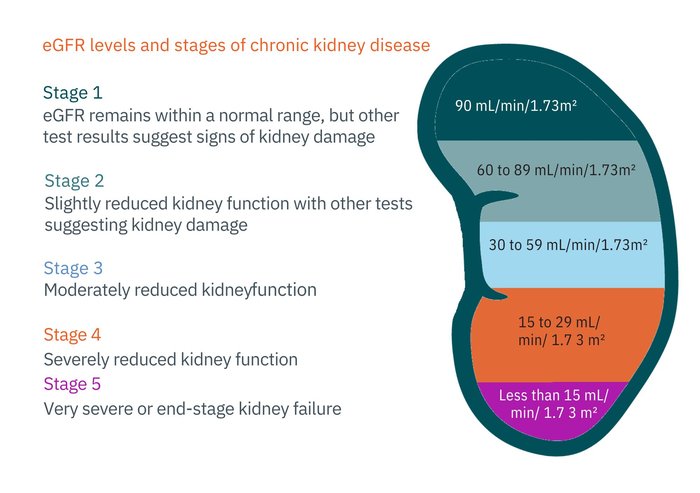
Doctors use a clear and systematic method to classify CKD. Staging helps them understand how well the kidneys are working, estimate the risk of progression, and decide what treatment or monitoring is needed. Two main factors determine your CKD stage how well your kidneys filter blood (eGFR) and how much protein leaks into your urine (albuminuria).
Understanding eGFR and Why It Matters
The estimated glomerular filtration rate (eGFR) tells how much blood your kidneys filter every minute, adjusted for body surface area. A healthy adult typically has an eGFR of about 90 mL/min/1.73 m² or higher.
As kidney function declines, the eGFR number drops. Doctors use eGFR to place you into one of five GFR stages (G1 to G5). Each stage reflects how much kidney function remains and guides how closely your kidneys should be monitored.
GFR Categories (G1–G5)
The GFR (glomerular filtration rate) tells how well your kidneys are filtering waste and fluid from your blood. It’s like checking the efficiency of a water filter the higher the number, the better the filtration. Doctors estimate this number using a blood test called eGFR (estimated GFR), which is adjusted for age, sex, and body size.
| Stage | eGFR (mL/min/1.73 m²) | Description | What It Means |
| G1 | ≥ 90 | Normal or high function with evidence of kidney damage (e.g., protein in urine, abnormal imaging). | Kidneys filter normally, but there are early signs of damage. |
| G2 | 60–89 | Mildly decreased kidney function with signs of damage. | Still near normal, but disease may be starting. |
| G3a | 45–59 | Mild to moderate decrease. | Slight loss of filtration; early symptoms possible. |
| G3b | 30–44 | Moderate to severe decrease. | Greater risk of complications such as anemia, bone changes, and fatigue. |
| G4 | 15–29 | Severe reduction in kidney function. | Requires close specialist care, preparation for kidney replacement may start. |
| G5 | < 15 | Kidney failure or near failure. | Dialysis or transplant may be needed; symptoms often severe. |
Albuminuria Categories (A1–A3)
The second part of staging is albuminuria, which measures how much albumin (a type of protein) leaks into your urine. Healthy kidneys keep albumin in your blood, so its presence in urine means damage to the filtering units (glomeruli).
| Category | Urine ACR (mg/g) | Description | Meaning |
| A1 | < 30 | Normal to mildly increased | Normal or very low risk of progression. |
| A2 | 30–300 | Moderately increased | Early sign of kidney damage; treatable stage. |
| A3 | > 300 | Severely increased | High risk of kidney failure and cardiovascular disease. |
Combining G and A to Gauge Risk
Doctors combine your G-stage (based on eGFR) and your A-stage (based on ACR) to create a complete risk picture. This combination is shown as a “heat map” — the KDIGO risk grid — which helps estimate the likelihood of CKD progression, cardiovascular events, and the need for kidney replacement therapy.
- For example, G2 + A1 represents low risk: kidney function is nearly normal and albumin loss is minimal.
- G3b + A3 indicates very high risk: both kidney function and urine protein levels show advanced disease.
Avoiding Common Mistakes in Staging
Accurate staging depends on proper interpretation of lab results. Some important points:
- Creatinine-based eGFR may not always reflect true kidney function. People who are very muscular, very thin, elderly, or malnourished may have misleading results.
- In such cases, a cystatin C-based eGFR or measured GFR test gives a more precise picture.
- Temporary changes in eGFR can occur due to dehydration, infection, or certain medications, so repeat testing after a few weeks may be needed before confirming CKD.
- Always interpret eGFR together with albuminuria and clinical findings, not in isolation.
Causes and Risk Factors of Chronic Kidney Disease
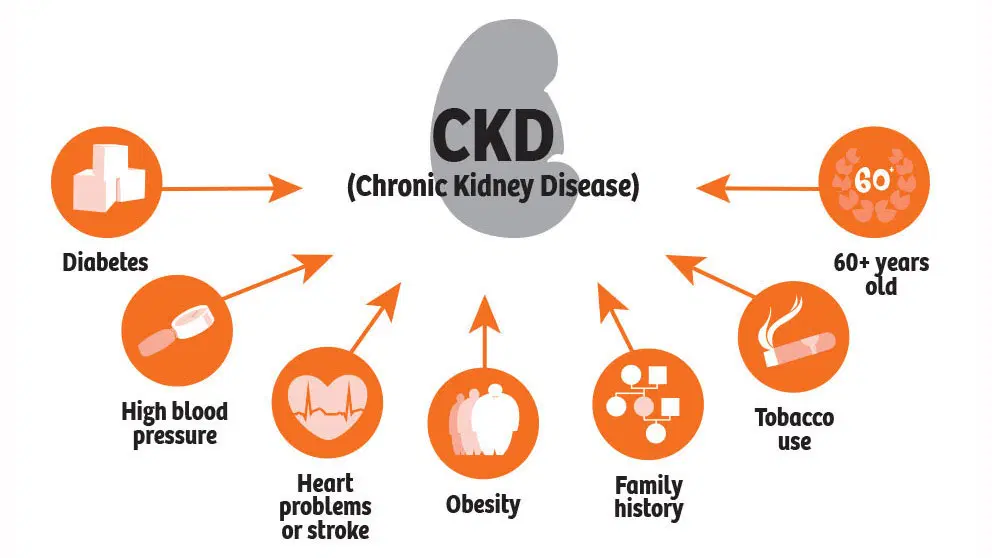
Chronic Kidney Disease (CKD) develops slowly over time and can have multiple causes. Knowing why it happens and who is at risk is the key to preventing it and catching it early. Most causes are linked to conditions or habits that damage the tiny filters in the kidneys (called nephrons) and reduce their ability to clean the blood.
1. Diabetes
Diabetes is the number one cause of CKD worldwide. High blood sugar over time damages the small blood vessels in the kidneys, making them leak protein and lose their filtering ability.
- Uncontrolled diabetes leads to a condition called diabetic kidney disease (DKD).
- Early signs include protein (albumin) in the urine, even when kidney function seems normal.
- Keeping blood sugar within target range and managing blood pressure can greatly slow kidney damage.
2. High Blood Pressure (Hypertension)
High blood pressure is both a cause and consequence of CKD.
- When pressure in the blood vessels is persistently high, it damages the delicate capillaries in the kidneys.
- Over time, this leads to scarring and reduced blood flow, making the kidneys less efficient.
- CKD can then further worsen blood pressure, creating a vicious cycle. Managing blood pressure early, ideally around 120 mm Hg systolic, can prevent long-term kidney injury.
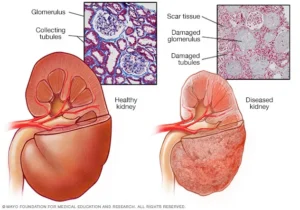
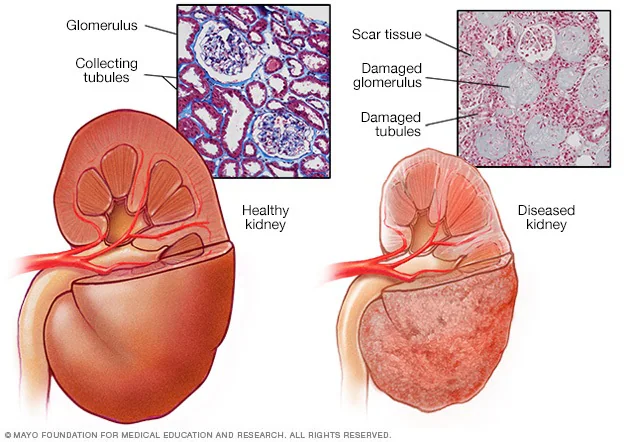
3. Glomerular Diseases
These are conditions where the glomeruli, the tiny filtering units in the kidneys, become inflamed or scarred.
- Examples include glomerulonephritis, IgA nephropathy, and lupus nephritis (caused by autoimmune disease).
- Symptoms may include blood in the urine, swelling in the legs, or foamy urine.
- Some forms are sudden and reversible, while others can lead to chronic damage if not treated promptly.
4. Inherited or Genetic Disorders
Some people inherit kidney conditions from their family. The most common is Polycystic Kidney Disease (PKD).
- In PKD, clusters of fluid-filled cysts grow inside the kidneys, gradually replacing healthy tissue.
- Over time, this leads to enlarged kidneys and reduced function.
- Genetic screening and early monitoring help slow progression through blood pressure and lifestyle control.
5. Urinary Tract and Obstructive Causes
When the flow of urine is blocked or slowed, pressure builds up in the kidneys, causing damage.
- Causes include kidney stones, enlarged prostate (in men), or structural problems in the urinary tract.
- Long-standing obstruction can lead to infection and scarring.
- Prompt treatment of urinary infections and obstruction helps prevent irreversible injury.
6. Autoimmune Diseases
Autoimmune conditions such as lupus or vasculitis can mistakenly attack kidney tissues.
- In lupus, immune complexes deposit in the kidneys, causing inflammation.
- Early diagnosis through blood and urine tests allows for treatments that can protect kidney function.
7. Medications and Toxic Substances
Certain drugs and toxins can silently harm the kidneys when used long term or in high doses.
- NSAIDs (non-steroidal anti-inflammatory drugs) such as ibuprofen and diclofenac are common causes when overused.
- Contrast dyes used in imaging tests can cause acute injury, especially in those with existing CKD.
- Some herbal supplements and traditional remedies contain heavy metals or unknown ingredients that strain the kidneys.
- Always check with a healthcare provider before taking any new medication or supplement.
8. Demographic and Social Risk Factors
Some people are more vulnerable to CKD because of their age, genetics, or social circumstances.
- Older adults naturally lose some kidney function with age, increasing vulnerability to CKD.
- Family history of kidney disease increases risk significantly.
- Certain ethnic groups (such as people of South Asian, African, or Indigenous descent) have higher genetic risk.
- Low access to healthcare and financial barriers often delay diagnosis and treatment, leading to faster progression.
9. Lifestyle and Preventable Risk Factors
Several modifiable habits can damage the kidneys over time, but they are fully preventable with awareness and action:
- Obesity increases the risk of diabetes and hypertension, both leading causes of CKD.
- Smoking directly injures kidney blood vessels and reduces oxygen flow.
- High-salt diets raise blood pressure and accelerate kidney strain.
- An unhealthy diet low in fruits and vegetables and high in processed foods worsens kidney burden.
- A sedentary lifestyle contributes to poor blood pressure and metabolic health.
Symptoms and Clinical Features by Stage
Chronic Kidney Disease (CKD) develops slowly and quietly. In the early stages, most people feel perfectly fine, which is why CKD is often called a “silent” disease. Recognizing even subtle signs early can make a huge difference in slowing its progression and preventing complications.
Early-Stage CKD (G1–G2)
In the first stages, kidney function remains mostly normal, but small amounts of damage have already begun. The kidneys are still able to filter waste effectively, so symptoms rarely appear.
- No noticeable symptoms most people discover CKD accidentally through a blood test showing slightly reduced eGFR or a urine test showing albumin (protein).
- Mild high blood pressure may appear, often the first visible clue.
- Some people with diabetes may notice microalbuminuria (early protein leak in urine).
Mid-Stage CKD (G3a–G3b)
At this stage, kidney function drops to about 30–59% of normal. Waste products start building up slowly, and symptoms can begin to surface. These may seem general or mild, making them easy to miss.
- Persistent fatigue or tiredness: The kidneys produce less erythropoietin, a hormone that stimulates red blood cells, leading to mild anemia.
- Nocturia (frequent urination at night): The kidneys lose their ability to concentrate urine, causing more trips to the bathroom.
- Swelling in ankles, feet, or hands (edema): Due to sodium and fluid retention.
- Dry, itchy skin caused by imbalances in minerals and waste buildup.
- Changes in appetite or mild nausea in some cases.
Advanced CKD (G4–G5)
As kidney function falls below 30%, toxins and fluid begin to accumulate in the body. The symptoms become stronger and more disruptive, often affecting several organs.
- Itchy skin (pruritus): Due to waste buildup and mineral imbalance.
- Loss of appetite and unexplained weight loss.
- Nausea or vomiting: Waste accumulation irritates the digestive system.
- Sleep disturbances and restless legs: Caused by toxin buildup and nerve irritation.
- Shortness of breath and swelling: Fluid overload may cause breathlessness or signs of heart failure.
- Bone and joint pain: From changes in calcium, phosphate, and parathyroid hormone (PTH) levels, known as CKD-MBD (mineral and bone disorder).
- Uncontrolled blood pressure: The kidneys’ inability to regulate fluid and salt increases cardiovascular strain.
Complications That Can Occur at Any Stage
Some problems can develop gradually across all stages of CKD and worsen as function declines:
- High blood pressure: Common at every stage and both a cause and consequence of kidney damage.
- Mineral and bone disorders: Imbalance of calcium, phosphate, and vitamin D leads to bone weakness and vascular calcification.
- Metabolic acidosis: When the kidneys can’t remove acid effectively, it causes muscle weakness and accelerates bone loss.
- Hyperkalemia (high potassium): Can cause irregular heartbeats and, if severe, life-threatening arrhythmias.
- Anemia: Reduced red blood cell production leads to constant fatigue, paleness, and poor concentration.
Red Flags That Need Immediate Medical Attention
Certain warning signs should never be ignored and require urgent evaluation by a healthcare provider:
- Sudden drop in eGFR or rapid rise in creatinine.
- Doubling of albuminuria (protein in urine) within a short time.
- New or severe fluid overload: Swelling of legs, face, or sudden weight gain.
- Very high potassium levels: May cause muscle weakness or heart rhythm changes.
- Severe shortness of breath or chest pain.
Screening, Case-Finding & Diagnosis of Chronic Kidney Disease
Early detection of Chronic Kidney Disease (CKD) gives the best opportunity to slow its progression, protect kidney function, and prevent complications like heart disease. Because CKD develops silently, screening focuses on people who are at higher risk rather than testing everyone.
Who Should Be Screened for CKD
Doctors recommend targeted screening for individuals more likely to develop kidney problems. These people benefit the most from regular testing and early treatment:
- People with diabetes (type 1 or type 2): High blood sugar over time damages kidney filters, so annual kidney checks are essential.
- People with hypertension (high blood pressure): Constant high pressure injures kidney blood vessels and accelerates decline.
- People with cardiovascular disease: Heart disease and kidney disease share risk factors, and each worsens the other.
- People with a family history of kidney disease: Genetic conditions like polycystic kidney disease or strong family trends increase risk.
- People who have had episodes of acute kidney injury (AKI): Even one serious kidney insult can leave lasting damage that later leads to CKD.
- Older adults or those using kidney-affecting medicines: Especially those on long-term painkillers (NSAIDs) or chemotherapy drugs.
How Often Should Testing Be Done
The frequency of testing depends on how high your risk is:
- High-risk patients (diabetes, hypertension, A2/A3 albuminuria): every 6 months or more often if values are changing quickly.
- Moderate-risk patients (mild albuminuria, family history): once a year.
- Low-risk individuals: every 1–2 years, especially if blood pressure and sugar remain normal.
How to Interpret the Results Correctly
Proper interpretation prevents misdiagnosis and unnecessary worry. Some key rules:
- CKD is defined by persistence: A single abnormal result does not mean you have CKD. The change must last at least 3 months on repeat testing.
- Confirm with repeat testing: Temporary changes can happen from dehydration, infection, or medications.
- Urine dipsticks are not enough: They can miss small protein leaks or give false positives; ACR testing is preferred for accuracy.
- Look at trends, not just one number: A slow decline over years is different from a sudden drop, which may indicate acute injury.
Why General Screening Isn’t Universal
While CKD is common, mass screening of everyone is not currently recommended. The reasons:
- CKD is more frequent in high-risk groups, making targeted testing more effective.
- False positives in healthy people can cause unnecessary anxiety and costs.
- The focus is on smart screening finding CKD early in those who can most benefit from treatment.
Monitoring Progression & Prognosis
Once CKD is diagnosed, you need to monitor over time to understand how fast it’s progressing and adjust management accordingly.
- eGFR slope: the rate at which eGFR falls over time gives insight into progression speed. A drop of more than 5 mL/min/1.73 m² per year is often considered “rapid” progression.
- Use of risk prediction tools such as the kidney failure risk equation (KFRE) helps estimate the risk of needing dialysis or transplant within 2-5 years.
- Monitor albuminuria changes: worsening A-category (for example A2 to A3) signals higher risk.
- Keep an eye on cardiovascular status: people with CKD are at high risk of heart disease and stroke, sometimes the risk of cardiovascular death exceeds that of kidney failure.
- Adjust follow-up interval based on risk: higher risk means more frequent review, labs, and possibly referral to a nephrologist.
Treatment: Slow Progression and Reduce Risk
Treatment of Chronic Kidney Disease (CKD) focuses on slowing down the loss of kidney function, preventing complications, and reducing the risk of heart disease and kidney failure. The aim is not only to protect the kidneys but also to safeguard overall health, since CKD and cardiovascular problems are closely linked.
Successful management involves a combination of lifestyle changes, medications, and close monitoring. Each area of care plays a vital role in keeping the kidneys stable for as long as possible.
Blood Pressure Control
Blood pressure management is the cornerstone of CKD treatment. High blood pressure damages the kidney’s delicate filtering units, and CKD in turn raises blood pressure forming a harmful cycle that must be broken.
Targets and Approach
- Aim for systolic blood pressure around 120 mmHg, if this is tolerated and safe.
- Use both lifestyle measures and medication to achieve targets.
Lifestyle strategies
- Reduce salt intake less than 2 grams of sodium daily (about 5 grams of salt).
- Maintain a healthy weight through regular exercise and balanced meals.
- Limit alcohol and avoid smoking, which both worsen blood vessel damage.
RAS Blockade (ACE Inhibitors / ARBs)
Medications such as ACE inhibitors (e.g., lisinopril, enalapril) or ARBs (e.g., losartan, valsartan) are first-line therapy in CKD.
Benefits
- They protect kidneys by reducing pressure inside the filtering units (glomeruli).
- They lower protein leakage (albuminuria) in urine, which directly slows CKD progression.
- They also help control blood pressure effectively.
When to start: Begin early in CKD, especially if albuminuria (A2 or A3) is present.
Monitoring tips
- After starting or increasing the dose, check serum creatinine and potassium within 1–2 weeks.
- A small rise in creatinine is expected (up to 30% from baseline), but a sharp increase may indicate a problem such as dehydration or blocked kidney blood flow.
Caution: Avoid combining ACE inhibitors and ARBs — this provides no extra benefit and increases risk of side effects.
SGLT2 Inhibitors
SGLT2 inhibitors (such as dapagliflozin or empagliflozin) were originally developed for diabetes but now play a major role in CKD care for people with or without diabetes.
Key benefits
- Slow down kidney disease progression.
- Reduce protein in urine.
- Lower risk of hospitalization for heart failure and cardiovascular death.
Usage and safety
- Can be used if eGFR is above 20–25 mL/min/1.73 m² (varies by medication).
- Pause during dehydration, vomiting, or major illness (“sick-day rule”) to prevent excessive fluid loss or kidney stress.
- Monitor eGFR and hydration status regularly.
Non-Steroidal Mineralocorticoid Receptor Antagonists (ns-MRA)
Drugs such as finerenone are newer options for people with CKD and diabetes, especially when albuminuria remains high despite ACEi or ARB therapy.
How they help
- Block harmful effects of hormones that cause inflammation and scarring in the kidneys.
- Reduce progression to kidney failure and lower cardiovascular events.
Precautions
- Regularly monitor potassium levels and kidney function, as these drugs can raise potassium.
- Should be used only under medical supervision.
Glycaemic Control in CKD (for people with diabetes)
Keeping blood sugar well-controlled protects kidneys from further damage.
Targets and medications:
- Aim for an HbA1c around 7%, individualized based on age, health, and risk of hypoglycaemia.
- Metformin is generally safe until eGFR falls below 30 mL/min/1.73 m²; doses may need reduction earlier.
- SGLT2 inhibitors and GLP-1 receptor agonists (e.g., semaglutide, liraglutide) offer heart and kidney protection beyond glucose control.
Lipid Management and Antiplatelet Therapy
CKD significantly increases the risk of heart attack, stroke, and vascular disease. Managing cholesterol is crucial.
- Statins are advised for most adults with CKD, regardless of cholesterol level, unless contraindicated.
- Antiplatelet therapy (like low-dose aspirin) may be recommended for those with established cardiovascular disease.
- Combine medication with exercise, weight management, and healthy diet for full benefit.
Diet and Lifestyle Modifications
A kidney-friendly lifestyle complements medication and greatly influences how fast CKD progresses.
- Sodium restriction: Less than 2 g sodium/day (about one teaspoon of salt).
- Protein intake: Around 0.8 g per kg body weight per day enough for health but not excessive, as too much protein increases kidney workload.
- Monitor potassium and phosphorus: Limit high-potassium foods (like bananas, potatoes, oranges) and high-phosphate foods (like processed meats, cola drinks) in advanced CKD.
- Maintain healthy weight: Regular physical activity helps control blood pressure and insulin sensitivity.
- Stay hydrated: Drink enough fluids, but avoid overhydration if swelling or heart failure is present.
- Avoid smoking and excessive alcohol.
Avoiding Nephrotoxins
Certain substances can harm the kidneys and should be limited or avoided in CKD.
Key precautions
- Avoid long-term NSAIDs (like ibuprofen, diclofenac, naproxen).
- Contrast dyes used for CT or angiography should be used only when necessary and with kidney protection measures (hydration, lower dose).
- Follow “sick-day rules”: During illness, vomiting, or dehydration, temporarily stop medications such as ACE inhibitors, ARBs, SGLT2 inhibitors, and diuretics, then restart once you recover.
- Always inform your doctor that you have CKD before new medications or procedures.
Vaccination and Infection Prevention
People with CKD are more prone to infections because of a weakened immune response. Preventive care makes a big difference.
Recommended vaccines
- Influenza (flu shot) annually.
- Pneumococcal vaccine to protect against pneumonia.
- Hepatitis B vaccine, especially for those who may need dialysis later.
Additional tips
- Treat urinary tract infections early.
- Practice good hygiene and stay current with all routine immunizations.
Managing Complications of Chronic Kidney Disease
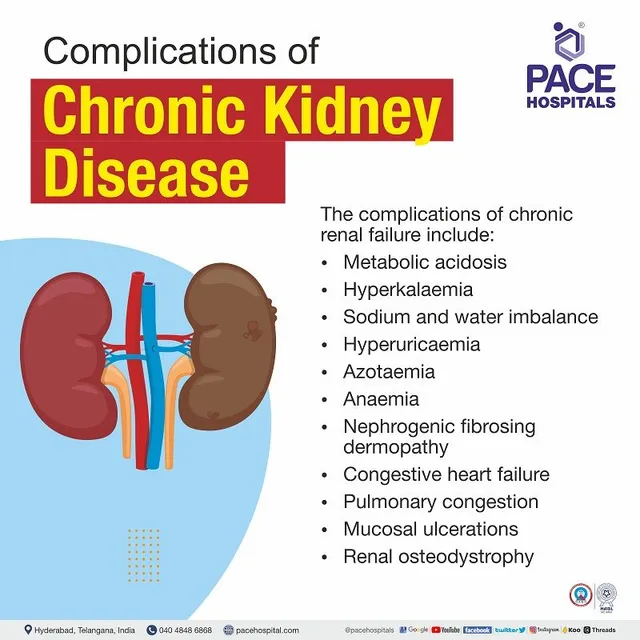
As Chronic Kidney Disease (CKD) advances, the kidneys lose more of their ability to balance fluids, electrolytes, and hormones. This leads to several complications that can affect multiple body systems. Managing these issues early and effectively helps improve quality of life, prevents hospitalizations, and slows overall disease progression.
- Anaemia of CKD
Healthy kidneys produce a hormone called erythropoietin (EPO) that signals the bone marrow to make red blood cells. When kidney function declines, less EPO is made, leading to anaemia a shortage of red blood cells.
- Monitor blood levels of haemoglobin, ferritin, and transferrin saturation (TSAT) regularly.
- Iron supplementation is often needed either oral tablets or intravenous (IV) iron if absorption is poor.
- If anaemia persists after correcting iron levels, erythropoiesis-stimulating agents (ESAs) can be prescribed to boost red blood cell production.
- Blood transfusions are used only when absolutely necessary, as repeated transfusions can complicate future kidney transplant options.
Common symptoms: Tiredness, shortness of breath, pale skin, and poor concentration. Treating anaemia improves energy, mood, and exercise tolerance.
- CKD Mineral and Bone Disorder (CKD–MBD)
CKD disrupts the body’s delicate balance of calcium, phosphate, vitamin D, and parathyroid hormone (PTH). When kidneys fail to excrete phosphate or activate vitamin D, bones weaken, and calcium deposits can form in blood vessels.
- Phosphate levels rise,
- Active vitamin D falls,
- PTH increases, which pulls calcium from bones, leading to bone pain and fractures.
How it’s managed
- Monitor calcium, phosphate, and PTH levels regularly.
- Restrict phosphate intake by limiting processed foods, dark colas, and high-phosphate meats.
- Phosphate binders (taken with meals) reduce phosphate absorption.
- Vitamin D supplements help restore balance.
- PTH-lowering medications may be added if hormone levels remain high.
Early management prevents bone disease, muscle weakness, and vascular calcification, all of which are major complications in CKD.
- Metabolic Acidosis
As the kidneys fail, they cannot remove acid efficiently, leading to metabolic acidosis, a condition where the blood becomes too acidic. This can cause muscle breakdown, bone loss, and faster kidney decline.
Management steps:
- Check blood bicarbonate levels during routine lab tests.
- If levels are low, oral sodium bicarbonate or other alkalinizing agents can correct acidity.
- Correcting acidosis not only improves muscle strength and bone health but also slows the rate of CKD progression.
- Hyperkalemia (High Potassium Levels)
Potassium is vital for nerve and muscle function, but when levels become too high, it can disrupt the heart’s rhythm sometimes dangerously. CKD and certain medications (ACE inhibitors, ARBs, MRAs) increase this risk.
How to manage
- Monitor potassium regularly, especially after medication changes.
- Adjust diet to reduce high-potassium foods like bananas, oranges, tomatoes, and potatoes if advised.
- Use potassium-binding medications when needed to remove excess potassium.
- If levels are persistently high, doctors may reduce or pause kidney-protective drugs until balance is restored.
- Volume and Hypertension Management
When kidneys cannot regulate fluid effectively, fluid overload becomes common. This leads to swelling, high blood pressure, and sometimes heart failure.
Key measures
- Monitor body weight daily: Sudden gain may signal fluid buildup.
- Use diuretics (water pills) to remove excess fluid under medical guidance.
- Limit salt and fluid intake to prevent further retention.
- Keep blood pressure well controlled with medications, as uncontrolled hypertension speeds kidney damage.
- Symptom Management (Pruritus, Neuropathy, Sleep Problems)
As waste builds up in advanced CKD, many people develop uremic symptoms—discomforts caused by toxin accumulation in the body.
Common symptoms include
- Itchy skin (pruritus): Often widespread and worse at night.
- Nerve pain or tingling (neuropathy): Due to toxin effects on nerves.
- Restless legs and poor sleep: Caused by nerve irritation and muscle discomfort.
Relief strategies
- Skin care: Use moisturizers, avoid very hot baths, and keep skin hydrated.
- Medications: Antihistamines or specific drugs for CKD-related itch and nerve pain may help.
- Good sleep habits: Consistent bedtime, limited caffeine, and relaxation routines.
- Address underlying CKD issues: Managing toxins and electrolyte imbalances often improves these symptoms naturally.
Conclusion
Chronic Kidney Disease (CKD) is a long-term loss of kidney function that progresses silently and can lead to kidney failure and heart disease. It’s staged using eGFR and albuminuria levels. Diabetes, hypertension, and genetic disorders are the main causes. Early CKD shows no symptoms, but fatigue, swelling, and nausea develop later. Treatment focuses on controlling blood pressure, blood sugar, and protein loss using ACE inhibitors or SGLT2 inhibitors. A low-salt diet, hydration, and avoiding kidney-toxic drugs help slow progression. Regular screening in high-risk individuals enables early detection and better management.
FAQs
What is Chronic Kidney Disease (CKD) and why is it important?
Chronic Kidney Disease (CKD) is a long-term condition in which the kidneys gradually lose their ability to filter waste, extra fluid, and toxins from the blood. This decline usually happens over months or years and often goes unnoticed in the early stages. CKD matters because it can silently progress to kidney failure and increase the risk of heart disease, high blood pressure, bone problems, and anemia if not detected early.
How do kidneys normally work?
Your kidneys filter the blood to remove waste and extra water, producing urine. They also regulate important minerals such as sodium and potassium, control blood pressure through hormones like renin, and help activate vitamin D to keep your bones strong. Because they perform so many critical functions, damage to the kidneys can cause widespread problems throughout the body.
How is CKD diagnosed and staged?
Doctors diagnose CKD using two key tests:
- eGFR (estimated Glomerular Filtration Rate): measures how well your kidneys filter blood.
- Albuminuria (Urine Albumin-to-Creatinine Ratio, ACR): checks how much protein leaks into your urine.
Based on these, CKD is divided into five G-stages (G1–G5) and three A-stages (A1–A3). The combination of both results determines how severe the disease is and how high the risk of kidney failure or cardiovascular complications might be.
What are the stages of CKD?
- Stage G1: eGFR ≥ 90 : Kidneys work well but show early signs of damage.
- Stage G2: eGFR 60–89 : Mild loss of kidney function.
- Stage G3a–G3b: eGFR 30–59 : Moderate loss; symptoms like fatigue and swelling may begin.
- Stage G4: eGFR 15–29 : Severe loss; preparation for dialysis or transplant may start.
- Stage G5: eGFR < 15 : Kidney failure; dialysis or transplant often required.
Albuminuria stages (A1–A3) indicate how much protein is in your urine higher levels mean more severe kidney damage.
What causes CKD?
The main causes of CKD include:
- Diabetes: high blood sugar damages kidney filters.
- High blood pressure (Hypertension): injures delicate blood vessels in the kidneys.
- Glomerular diseases: such as glomerulonephritis and lupus nephritis.
- Genetic disorders: like Polycystic Kidney Disease (PKD).
- Long-term NSAID use: painkillers like ibuprofen can harm kidneys.
- Urinary blockages or infections: such as stones or prostate enlargement.
- Lifestyle factors: smoking, obesity, and high-salt diets increase risk.
What are the symptoms of CKD?
In early stages, CKD may cause no noticeable symptoms. As it progresses, signs can include:
- Fatigue and weakness
- Swelling in ankles, feet, or hands
- Frequent urination (especially at night)
- Dry or itchy skin
- Loss of appetite or nausea
How is CKD treated?
Treatment aims to slow progression and prevent complications. Key measures include:
- Blood Pressure Control: Aim for around 120 mmHg systolic using ACE inhibitors or ARBs.
- Diabetes Control: Keep blood sugar and HbA1c around target levels.
- SGLT2 Inhibitors (dapagliflozin, empagliflozin): slow kidney decline and protect the heart.
- Finerenone (ns-MRA): used for CKD with diabetes to reduce inflammation and scarring.
- Lifestyle changes: low-salt diet, regular exercise, quitting smoking, and maintaining a healthy weight.
- Avoid harmful drugs: limit NSAIDs and inform doctors about CKD before new prescriptions.
What diet is recommended for people with CKD?
A kidney-friendly diet can slow disease progression and manage complications:
- Limit sodium: less than 2 grams per day (about 1 teaspoon of salt).
- Moderate protein: about 0.8 g per kg of body weight daily.
- Control potassium and phosphorus: reduce high-potassium (bananas, oranges) and high-phosphate foods (processed meats, cola).
- Stay hydrated: drink enough water but avoid excess if swelling or heart problems exist.
- Avoid smoking and excessive alcohol.
What are common complications of CKD?
As kidney function declines, several complications can occur:
- Anemia: reduced red blood cell production causes fatigue.
- Bone-Mineral Disorder: weak bones due to calcium and phosphate imbalance.
- Metabolic Acidosis: too much acid in the blood causing muscle loss.
- Hyperkalemia: high potassium levels affecting heart rhythm.
- Fluid Overload & Hypertension: swelling, breathlessness, and increased heart strain.
What lifestyle changes help manage CKD?
- Maintain a healthy weight through exercise and balanced diet.
- Quit smoking and avoid secondhand smoke.
- Limit alcohol and avoid sugary drinks.
- Monitor blood pressure and sugar regularly.
- Get vaccinated (flu, pneumococcal, hepatitis B) to reduce infection risk.
- Follow your doctor’s advice on medications and follow-up visits.
When should I see a kidney specialist (nephrologist)?
You should see a nephrologist if:
- Your eGFR is below 30 (Stage G4 or G5).
- You have A3 albuminuria (high protein in urine).
- There’s a rapid decline in kidney function.
- You have difficult-to-control blood pressure or complications like anemia and bone disease.
Can CKD be reversed?
CKD usually cannot be completely reversed, but its progression can be slowed or stabilized with the right treatment and lifestyle choices. Managing blood pressure, diabetes, and cholesterol, along with avoiding kidney-damaging substances, can preserve kidney function for many years.
What are warning signs that need urgent attention?
Seek medical help immediately if you experience:
- A sudden drop in eGFR or rise in creatinine
- Severe swelling or shortness of breath
- Chest pain or irregular heartbeat
- Persistent vomiting or loss of appetite
- Very high potassium levels causing muscle weakness or palpitations
What is the long-term outlook for people with CKD?
With early diagnosis, proper medication, and lifestyle changes, many people live long, healthy lives without needing dialysis or a kidney transplant. Regular follow-up with your healthcare provider, monitoring of kidney function, and staying informed about your condition can make a huge difference in maintaining quality of life.
Reference
- National Health Service (NHS) UK – Chronic Kidney Disease (CKD) Overview
Provides a complete overview of CKD, its stages, causes, symptoms, and treatment approaches. https://www.nhs.uk/conditions/kidney-disease/ - Centers for Disease Control and Prevention (CDC) – Chronic Kidney Disease Basics Covers CKD causes, risk factors, prevention, and management strategies. https://www.cdc.gov/kidneydisease/basics.html
- National Institute for Health and Care Excellence (NICE) – CKD: Assessment and Management (NG203) Clinical guideline detailing diagnosis, monitoring, and treatment recommendations for CKD. https://www.nice.org.uk/guidance/ng203
- Mayo Clinic – Chronic Kidney Disease Describes symptoms, causes (diabetes, hypertension, glomerular diseases), and treatment options including ACE inhibitors, ARBs, and SGLT2 inhibitors.
https://www.mayoclinic.org/diseases-conditions/chronic-kidney-disease
Aubrey Carson is an RDN with 9 years across hospital, outpatient, and private practice settings. They earned an MS in Clinical Nutrition from Tufts University – Friedman School (2016) and completed a Dietetic Internship at Mayo Clinic. Aubrey specializes in micronutrient assessment, evidence-based supplementation, and patient education. Their work includes CE presentations for the Academy of Nutrition and Dietetics and collaborations with Mass General Brigham on nutrition education resources.