How Diabetes Affects Liver Health: Understanding the Connection

Diabetes doesn’t just disturb blood sugar it also affects the liver, a vital organ responsible for managing fats, energy storage, and detoxification. When insulin or glucose control goes off balance, the liver becomes overwhelmed, leading to excessive fat buildup inside its cells. Over time, this triggers inflammation, scarring, and reduced liver function, increasing the risk of serious complications such as cirrhosis and liver cancer. Maintaining healthy blood sugar levels and supporting liver health are equally important to prevent long-term damage and protect overall metabolic well-being.
Key Takeaways on How Diabetes Affects Liver Health
- Over 70% of people with type 2 diabetes develop some degree of fatty liver.
- Liver disease in diabetes can advance silently, even with normal blood tests.
- Insulin resistance promotes fat accumulation and liver inflammation.
- Early screening using FIB-4 or ultrasound helps detect disease before scarring.
- Weight loss, balanced diet, and select diabetes medications improve liver health.
- Untreated, liver disease may progress to cirrhosis, liver failure, or cancer.
Quick Facts and Why It Matters
Diabetes doesn’t just affect blood sugarit also places a heavy load on the liver, one of the body’s main organs for managing energy and fats. Understanding this link helps people take timely steps to protect their liver before irreversible damage occurs. Research shows that:
- Over 70% of people with type 2 diabetes have some degree of fatty liver.
- Diabetes increases the risk of liver fibrosis, cirrhosis, and even cancer.
- Liver disease can progress silently, with normal blood tests in early stages.
Understanding the Liver’s Role in Blood Sugar
The liver is your body’s chemical factory. It stores energy, filters toxins, and manages fat and glucose. When working properly, it keeps blood sugar balanced between meals.
- Glucose Storage and Release: The liver stores excess glucose as glycogen and releases it when blood sugar drops.
- Fat Metabolism: It converts excess carbohydrates into fats and exports them as lipoproteins.
- Detoxification: The liver filters waste and metabolizes medications and hormones.
How Diabetes Affects Liver health
Diabetes, especially type 2, has a profound impact on the liver because the liver is central to regulating blood sugar, storing energy, and managing fat metabolism. When blood sugar is consistently high, the liver’s normal functions can be disrupted, leading to short- and long-term damage. Here’s how diabetes harms the liver:
- Fat Accumulation (Non-Alcoholic Fatty Liver Disease – NAFLD / MASLD): High blood sugar and insulin resistance cause the liver to convert excess glucose into fat. Over time, fat builds up in liver cells, leading to a condition called fatty liver. This is the most common liver complication in people with diabetes.
- Inflammation and Fibrosis: Excess fat triggers inflammation, which damages liver cells. Persistent inflammation can progress to fibrosis (scarring), reducing liver function. In severe cases, it can lead to cirrhosis, which impairs the liver’s ability to detoxify the body, store nutrients, and regulate metabolism.
- Increased Risk of Liver Cancer: Chronic liver damage from fatty liver and cirrhosis increases the risk of hepatocellular carcinoma, a type of liver cancer. Diabetes itself, independent of liver fat, is considered a risk factor.
- Altered Glucose Regulation: The liver normally stores glucose as glycogen and releases it when needed. In diabetes, insulin resistance impairs this process, leading to fluctuating blood sugar levels and further metabolic stress on the liver.
- Higher Susceptibility to Infections and Liver Stress: Diabetes can weaken the immune system and increase oxidative stress in liver cells, making the liver more vulnerable to damage from toxins, medications, and infections.
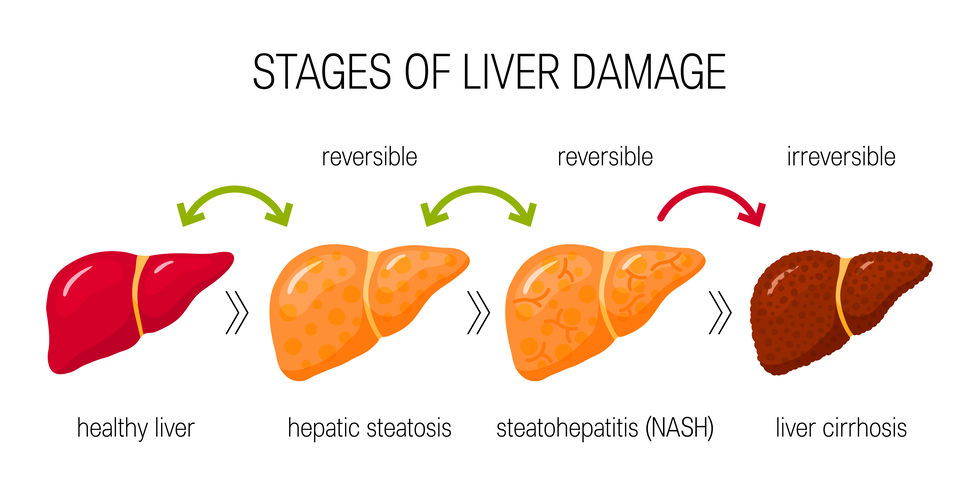
Stages of Liver Disease in Diabetes
The impact of diabetes on the liver happens gradually. It usually starts with mild fat buildup that seems harmless but can silently progress into inflammation, scarring, and serious liver damage if not addressed early. Recognizing these stages helps in taking preventive action before complications arise.
- Steatosis (Fatty Liver): This is the earliest stage, where fat builds up inside liver cells. It’s often reversible with lifestyle changes.
- Steatohepatitis (MASH): When fat buildup leads to inflammation and cell injury, it becomes metabolic dysfunction–associated steatohepatitis (MASH). This stage carries a higher risk of scarring.
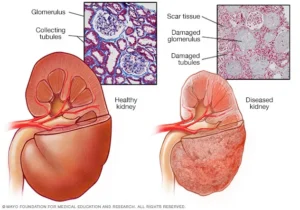
- Fibrosis: Scar tissue starts forming. The more scarring, the stiffer and less efficient the liver becomes.
- Cirrhosis: At this advanced stage, scar tissue replaces most healthy liver tissue, causing serious problems like fluid buildup, jaundice, and bleeding.
- Liver Cancer (HCC): Long-term inflammation and scarring raise the risk of hepatocellular carcinoma (HCC), especially in diabetics.
The Two-Way Connection
The relationship between diabetes and liver disease isn’t one-directional. Each condition fuels the other, creating a cycle that can speed up both liver damage and blood sugar complications. Understanding this mutual impact is key to breaking the cycle through early lifestyle and medical intervention.
- Diabetes increases liver fat and inflammation, accelerating liver damage.
- Liver disease worsens insulin resistance, making blood sugar harder to control.
Risk Factors That Make Liver Damage Worse
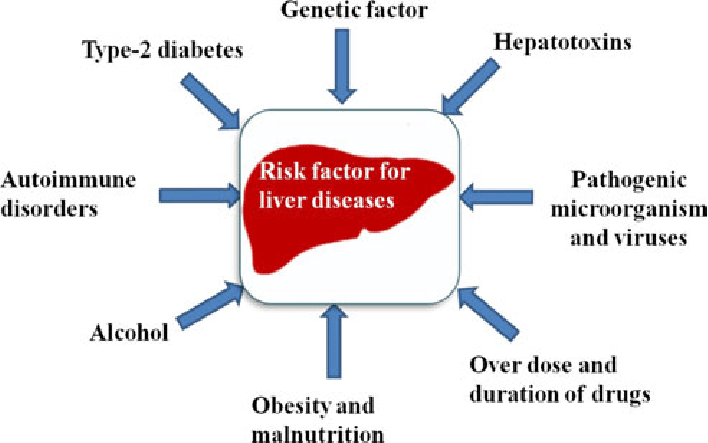
Certain lifestyle and health factors amplify the risk for liver problems in diabetics. These risks often act together, increasing inflammation and fat buildup in the liver while making blood sugar control more difficult. Identifying and managing them early can greatly reduce long-term liver damage.
- Obesity and central fat: Excess belly fat directly affects liver metabolism.
- High cholesterol and triglycerides: These worsen fatty liver and insulin resistance.
- Sleep apnea: Low oxygen levels during sleep increase oxidative stress.
- Polycystic ovary syndrome (PCOS): Adds to metabolic imbalance in women.
- Hypothyroidism: Slower metabolism aggravates fat accumulation.
- Alcohol consumption: Even moderate drinking can worsen fatty liver when combined with diabetes.
How to Detect Liver Problems Early
Most people with diabetes and liver disease feel perfectly fine until it’s advanced. That’s why regular screening is important. Detecting liver problems early allows treatment to start before irreversible scarring develops, improving long-term outcomes and overall metabolic health.
- Who Should Be Screened: All adults with type 2 diabetes should be screened for liver disease, regardless of symptoms or liver enzyme levels.
- Simple Initial Tests: Doctors usually start with: FIB-4 Index, A simple calculation using age, liver enzymes, and platelets.Ultrasound or elastography, Measures liver fat and stiffness.
- Why Normal ALT Can Mislead: A “normal” ALT test does not mean the liver is healthy. Many people with advanced liver disease have normal enzyme levels.
- When to Refer to a Specialist: If noninvasive tests suggest advanced fibrosis or cirrhosis, a hepatologist (liver specialist) should be consulted.
Managing Diabetes When Liver Is Involved
Good news: liver health can improve with the right approach. Diabetes management and liver protection go hand in hand.
1. Lifestyle Comes First
Small, consistent changes make a big difference:
- Weight loss: Aim for at least 7–10% reduction in body weight.
- Balanced diet: Prefer whole grains, vegetables, lean protein, and healthy fats.
- Avoid added sugars and refined carbs: They drive fat production in the liver.
- Exercise: 150 minutes of activity per week improves insulin sensitivity and fat burning.
2. Medications That Benefit the Liver
Some diabetes medications have proven liver benefits:
- GLP-1 receptor agonists (like semaglutide): Help with weight loss and reduce liver fat.
- Pioglitazone: Improves liver inflammation and fat metabolism.
- SGLT2 inhibitors: Lower blood sugar and modestly improve liver enzymes.
3. Managing Cholesterol and Blood Pressure
- Statins are safe and recommended for diabetics with fatty liver.
- Controlling cholesterol and blood pressure lowers both liver and heart risks.
4. When to Escalate
Referral is essential if:
- Liver stiffness or fibrosis markers increase
- Imaging shows cirrhosis or nodules
- Symptoms like swelling, fatigue, or jaundice appear
Special Considerations
Some groups with diabetes face unique challenges when it comes to liver health. Factors like age, gender, and hormonal changes can influence how liver disease develops and progresses. Recognizing these differences helps ensure that prevention and monitoring are tailored to individual needs.
- Type 1 Diabetes: Although less common, fatty liver can still occur, especially with obesity or insulin resistance. Regular screening is worthwhile.
- Pregnancy: Women with diabetes during pregnancy should be monitored for liver function, as fatty liver can increase complications.
- Younger Adults: Early-onset diabetes and obesity raise lifetime risk. Prevention and education at younger ages can reduce long-term liver damage.
Long-Term Outcomes
If ignored, fatty liver linked with diabetes can cause serious complications. Over time, continuous inflammation and scarring weaken the liver’s ability to function and also impact overall health. These outcomes highlight why early diagnosis and lifestyle intervention are critical for long-term well-being.
- Cirrhosis and liver failure
- Liver cancer (HCC)
- Higher cardiovascular disease risk
What Patients Should Know
People with diabetes can take several steps to protect their liver. Simple lifestyle habits and regular monitoring go a long way in preventing severe liver damage. Understanding what actions truly make a difference helps patients take control of both their blood sugar and liver health effectively.
- Get checked for fatty liver regularly.
- Focus on losing weight gradually but consistently.
- Eat whole, unprocessed foods and stay physically active.
- Ask your doctor about medications that support both blood sugar and liver health.
- Avoid excess alcohol and unnecessary supplements.
- Manage cholesterol and blood pressure carefully.
Research and Future Treatments
New therapies and diagnostic tools are being developed to treat liver disease in diabetes more precisely.
- Dual and triple incretin therapies (targeting multiple hormones) show promise.
- Noninvasive biomarkers and imaging may soon replace liver biopsies.
- Combination therapy (metabolic + antifibrotic) is the next frontier.
Conclusion
Diabetes and liver health are deeply interconnected, sharing the same metabolic roots. High blood sugar and insulin resistance can gradually overload the liver, leading to fat buildup, inflammation, and scarring that may progress to cirrhosis or liver cancer if ignored. The good news is that this damage is often preventable and, in early stages, even reversible. Regular liver screening, healthy weight management, a balanced diet, and physical activity are the strongest defenses. Certain diabetes medications like GLP-1 receptor agonists, pioglitazone, and SGLT2 inhibitors also show liver-protective benefits. Recognizing the signs early and maintaining consistent follow-up with healthcare professionals can make a life-changing difference. Protecting your liver is not just about liver health—it’s about improving your entire metabolic and cardiovascular future.
FAQs
1. Do all people with diabetes need liver screening?
Yes. Everyone with type 2 diabetes should have at least an initial liver assessment through simple blood tests or imaging. Regular follow-ups help detect silent fatty liver changes early.
2. Can I have liver disease if my liver enzymes are normal?
Absolutely. Many people with fatty liver or even fibrosis show normal ALT and AST levels, so normal results don’t always mean your liver is healthy. Imaging or FibroScan can provide a clearer picture.
3. What kind of diet helps most?
A Mediterranean-style diet rich in vegetables, fruits, whole grains, fish, and olive oil supports liver repair and reduces fat accumulation. It also helps balance blood sugar and cholesterol levels.
4. How much weight loss improves liver health?
Losing just 7–10% of your body weight can significantly reduce liver fat and inflammation. Even modest weight loss improves insulin sensitivity and liver enzyme levels.
5. Are statins safe if I have fatty liver?
Yes, statins are generally safe for people with fatty liver. In fact, they help reduce cardiovascular risk, which is higher in those with liver and metabolic conditions.
6. Can fatty liver cause diabetes?
Yes. Excess fat in the liver worsens insulin resistance, making it harder for your body to control blood sugar. Over time, this can lead to or aggravate type 2 diabetes.
7. What medications help both diabetes and liver disease?
Medications like pioglitazone, GLP-1 receptor agonists, and SGLT2 inhibitors benefit both conditions. They reduce liver fat, improve glucose control, and may slow fibrosis progression.
8. Should I avoid alcohol completely?
If you have fatty liver, it’s best to avoid alcohol entirely or limit it to rare occasions. Even small amounts can worsen inflammation and liver damage over time.
9. How often should I check liver health?
If your condition is stable, testing every 1–2 years is sufficient. Those with fibrosis or cirrhosis should get checked more frequently as advised by their doctor.
10. What are danger signs that need urgent medical review?
Seek immediate medical attention for jaundice, abdominal swelling, confusion, or vomiting blood. These signs may indicate severe liver damage or failure.
Reference
CDC – Type 2 Diabetes and Liver Disease: https://www.cdc.gov/diabetes/diabetes-complications/type-2-diabetes-liver-disease.html
University of Chicago Medicine – Type 2 Diabetes and Liver Disease: https://www.uchicagomedicine.org/forefront/gastrointestinal-articles/2024/march/type-2-diabetes-liver-disease
Mayo Clinic – Diabetes: How do I help protect my liver?: https://www.mayoclinic.org/diseases-conditions/diabetes/expert-answers/diabetes/faq-20058461
Verywell Health – Diabetes and Liver Cancer: What Is the Relationship?: https://www.verywellhealth.com/diabetes-and-liver-cancer-6824448
Times of India – Diabetes: How it silently impacts liver, kidneys, and heart: https://timesofindia.indiatimes.com/life-style/health-fitness/health-news/diabetes-how-it-silently-impacts-liver-kidneys-and-heart/articleshow/121746416.cms
Autum Harkins is a CNS with an MS in Clinical Nutrition from Maryland University of Integrative Health (2017) and 8 years in integrative clinics. She develops individualized protocols for deficiencies, digestive health, and women’s wellness, prioritizing third-party-tested supplements. Autum contributes to case series and webinars and mentors practitioners on lab interpretation. Credentials: CNS Board (ANA/BCNS) number, state nutrition licensure where applicable, and professional memberships with links.