Kidney Stones: Causes, Symptoms & Prevention

Kidney stones are hard crystal deposits that form in the kidneys when minerals and salts in urine become too concentrated. They cause intense pain and discomfort but can be largely prevented through hydration, diet, and lifestyle control.
Key Takeaways
- Kidney stones form from excess calcium, oxalate, or uric acid in concentrated urine.
- Common types include calcium oxalate, uric acid, struvite, and cystine stones.
- Dehydration, high sodium intake, and excessive animal protein are major risk factors.
- Symptoms include sharp flank pain, blood in urine, and painful urination.
- Prevention relies on drinking 2–3 liters of water daily, maintaining a balanced diet, and limiting salt and oxalate-rich foods.
- Regular medical checkups and early treatment prevent recurrence and complications.
What Are Kidney Stones?
Kidney stones (also called renal calculi or nephrolithiasis) are solid masses made of crystals that originate in the kidneys. They develop when urine contains more crystal-forming substances such as calcium, oxalate, and uric acid than the fluid in urine can dilute. At the same time, your urine may lack substances that keep crystals from sticking together, creating an ideal environment for stones to form.
Types of Kidney Stones
- Calcium stones : The most common type, usually made of calcium oxalate.
- Struvite stones : Often formed after urinary tract infections.
- Uric acid stones : Common in people who lose too much fluid or eat high-protein diets.
- Cystine stones : Rare, caused by a genetic condition that leads to cystine leaking into urine.
Causes of Kidney Stones
Kidney stones can form due to a combination of dietary habits, fluid intake, and certain medical or genetic factors. Understanding the underlying causes can help prevent their formation and recurrence.
1. Low Urine Volume and Dehydration
When you don’t drink enough fluids, your urine becomes highly concentrated. This increases the likelihood that minerals and salts such as calcium, oxalate, and uric acid will crystallize and form stones. Low urine volume is one of the most common and preventable causes of kidney stones.
- Drink enough water so your urine stays pale yellow, not dark.
- Increase your fluid intake if you exercise regularly, work outdoors, or live in a hot climate.
- Aim for 2–3 liters of water daily, unless otherwise advised by your doctor.
2. Imbalance of Minerals and Salts
Your urine contains a natural balance of substances that either promote or prevent stone formation. When this balance is disrupted too much of promoters (like calcium, oxalate, or uric acid) and too little of inhibitors (like citrate or magnesium) stones can develop.
- Limit salt and processed foods, which can increase calcium levels in urine.
- Eat more fruits and vegetables, as they help maintain a healthier urinary pH and supply natural inhibitors.
- Moderate animal protein (meat, eggs, seafood), which can raise uric acid levels.
3. Diet High in Oxalate or Protein
Foods high in oxalate (such as spinach, beets, nuts, and chocolate) or animal protein (like red meat, poultry, and eggs) can increase stone risk. Oxalate binds with calcium in urine to form calcium oxalate stones, while excess protein increases uric acid levels and reduces urinary citrate, a natural stone inhibitor.
- Limit high-oxalate foods if you’ve had calcium oxalate stones.
- Choose plant-based proteins more often.
- Balance meals with calcium-rich foods (like yogurt or milk) to reduce oxalate absorption.
4. High Sodium Intake
Too much salt causes your kidneys to excrete more calcium into urine, raising the risk of stone formation. A high-sodium diet also reduces citrate levels, further encouraging crystal growth.
- Avoid adding extra salt at the table.
- Limit processed snacks, canned soups, and fast foods.
- Aim for less than 2,300 mg of sodium per day (about 1 teaspoon of salt).
5. Obesity and Metabolic Conditions
Obesity changes the acid balance in urine, making it more acidic, a condition that promotes uric acid and calcium oxalate stones. Conditions like metabolic syndrome and diabetes are also linked to increased stone risk.
- Maintain a healthy weight through a balanced diet and regular exercise.
- Manage blood sugar levels if diabetic.
- Consult your doctor about weight management plans that suit your health.
6. Medical Conditions and Medications
Certain health issues can increase stone risk:
- Gout : raises uric acid levels.
- Hyperparathyroidism: causes high calcium levels in blood and urine.
- Inflammatory bowel disease (IBD): affects calcium and water absorption.Some medications (like diuretics, calcium-based antacids, or certain antivirals) may also contribute.
Pointers
- Discuss potential side effects of long-term medications with your doctor.
- Treat and monitor underlying conditions regularly.
- Get periodic urine and blood tests if you’re prone to stones.
7. Family History or Genetic Predisposition
If kidney stones run in your family, your risk increases. Some genetic disorders, such as cystinuria, cause certain amino acids to accumulate in urine, leading to cystine stones.
- Stay extra vigilant about hydration and diet if you have a family history.
- Inform your doctor about genetic predispositions for preventive guidance.
Types of Kidney Stones and Their Causes
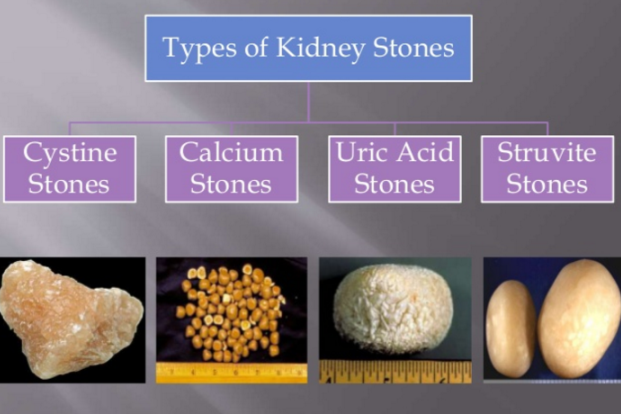
Each type of kidney stone forms under different urinary conditions and has unique contributing factors. Knowing the stone type is important because it guides both prevention and treatment strategies.
1. Calcium Oxalate Stones
These are the most common type of kidney stones. They form when calcium combines with oxalate, a naturally occurring substance found in certain foods and also produced by the liver.
Causes:
- High levels of calcium or oxalate in urine
- Low levels of citrate, which prevents crystal formation
- Diets high in oxalate-rich foods (e.g., spinach, nuts, tea, chocolate)
- Dehydration or low urine volume
Prevention Tips:
- Stay well-hydrated
- Limit oxalate-rich foods
- Maintain adequate dietary calcium intake
- Reduce salt and animal protein
2. Calcium Phosphate Stones
These stones form when calcium combines with phosphate in alkaline (less acidic) urine.
Causes:
- Urinary tract conditions that make urine too alkaline
- Overactive parathyroid glands (hyperparathyroidism)
- Certain renal tubular disorders that affect acid-base balance
Prevention Tips:
- Manage urinary pH through diet or prescribed medication
- Treat underlying kidney or parathyroid disorders
- Stay hydrated to keep urine diluted
3. Uric Acid Stones
These stones develop when urine is too acidic. Uric acid is a waste product formed from the breakdown of purines, which are found in animal protein.
Causes:
- Diet high in red meat, organ meats, and shellfish
- Gout or high uric acid levels in the blood
- Chronic dehydration
- Metabolic disorders affecting purine metabolism
Prevention Tips:
- Drink plenty of water to dilute urine
- Eat more fruits and vegetables to make urine less acidic
- Limit intake of red meat and seafood
- Take prescribed medication (e.g., allopurinol) if needed
4. Struvite Stones
Struvite stones form in response to urinary tract infections (UTIs), especially those caused by bacteria that produce ammonia. These stones can grow quickly and become quite large.
Causes:
- Chronic or recurrent urinary tract infections
- Bacteria that raise urine pH (make it alkaline)
Prevention Tips:
- Treat UTIs promptly and completely
- Regular urine tests for people with recurrent infections
- In severe cases, surgery may be required to remove large stones
5. Cystine Stones
These are rare stones that form due to a genetic disorder called cystinuria, in which excess cystine (an amino acid) leaks into the urine and forms crystals.
Causes: Inherited genetic condition leading to high cystine concentration in urine
Prevention Tips:
- Drink large amounts of water throughout the day and night
- Take medications that help dissolve cystine or reduce its concentration
- Follow up regularly with a nephrologist for long-term management
Medical Conditions and Medications
Certain health conditions and medications can increase the risk of kidney stone formation by altering urine composition, promoting mineral buildup, or changing urine acidity.
- Gout: Increases uric acid levels in the blood and urine, leading to uric acid stones.
- Obesity: Alters the body’s acid-base balance and increases calcium and uric acid in urine.
- Inflammatory bowel disease (IBD): Reduces calcium absorption and increases oxalate levels.
- Diabetes: Causes more acidic urine, favoring uric acid stone formation.
- Hyperparathyroidism: Raises calcium levels in both blood and urine.
Medications
Some medicines can also raise stone risk, especially with long-term use:
- Certain diuretics (water pills) that increase calcium in urine.
- Calcium-based antacids that elevate calcium levels.
- Antiseizure medications such as topiramate.
- HIV treatment drugs (like indinavir) that can crystallize in urine.
Pointers:
- Discuss your medications and medical conditions with your doctor if you have recurring stones.
- Managing underlying health problems and adjusting medications where appropriate can lower your risk.
Family History and Lifestyle Factors
A family history of kidney stones greatly increases your likelihood of developing them, as genetic factors can affect how your body processes minerals, salts, and certain compounds. In addition, several lifestyle habits can contribute to stone formation:
- High-sodium diet : Raises calcium levels in urine.
- Excess animal protein intake : Increases uric acid and reduces citrate.
- Lack of physical activity : Slows metabolism and affects calcium balance.
- Prolonged dehydration or working in hot environments : Concentrates urine and promotes crystallization.
Pointers:
- If kidney stones run in your family, be proactive about hydration and diet.
- Maintain a balanced lifestyle with regular exercise and a nutrient-rich diet.
- Monitor urine color and volume pale, plentiful urine usually means good hydration.
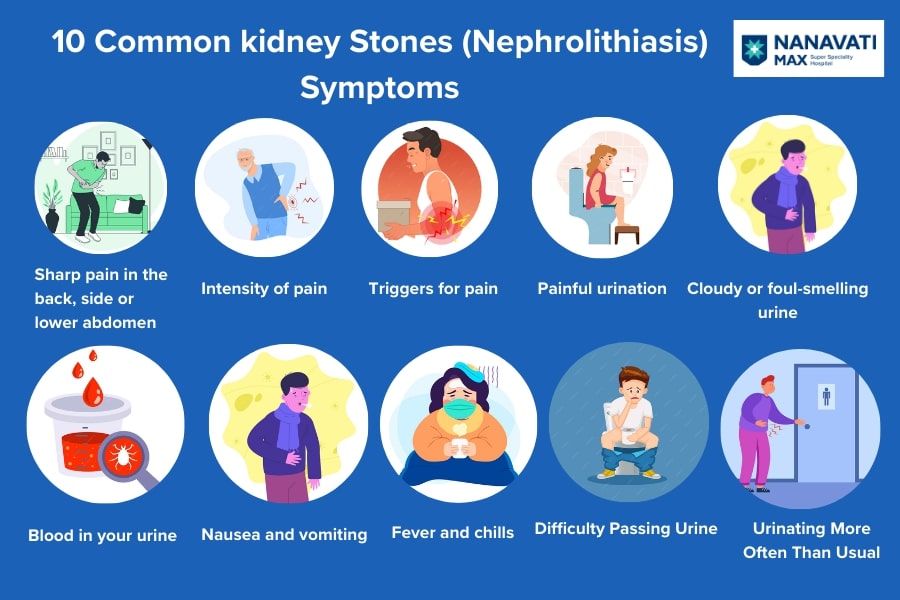
Symptoms & When to Seek Help
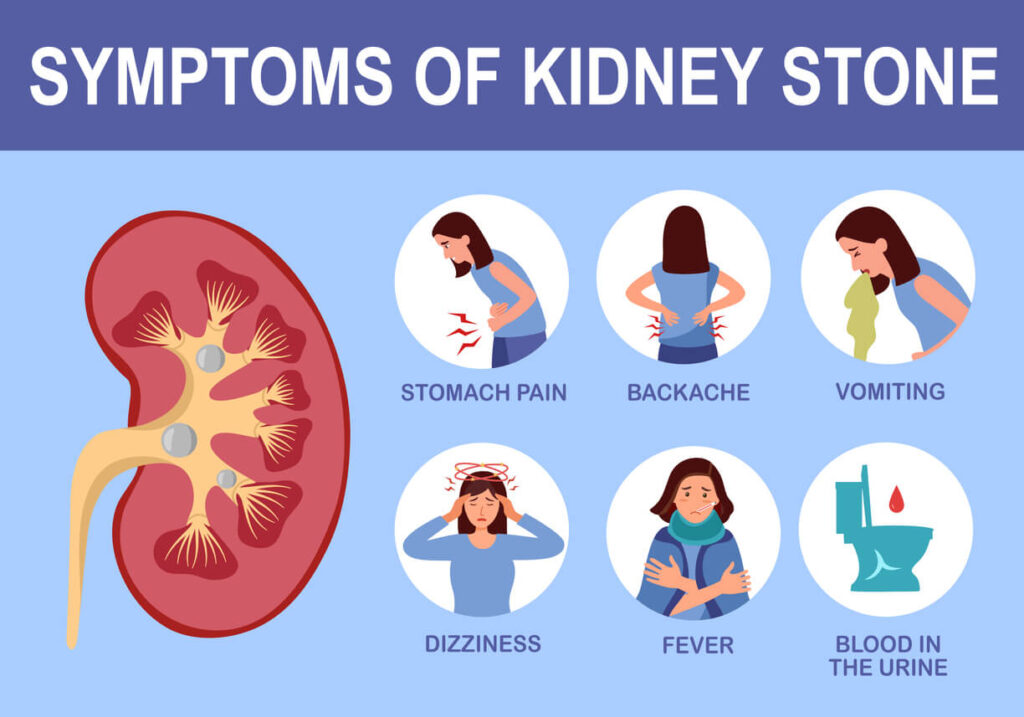
Recognizing early symptoms of kidney stones can help prevent complications and allow for timely treatment. The intensity and location of pain may vary depending on the size and movement of the stone within the urinary tract.
- Sharp, cramping pain in the back, side (flank), or lower abdomen often described as coming in waves.
- Pain that moves toward the groin as the stone travels down the urinary tract.
- Blood in the urine (a reddish, pink, or brown tint), also called hematuria.
- Nausea or vomiting, often due to intense pain.
- Frequent urge to urinate or a burning sensation while passing urine.
- Cloudy or foul-smelling urine (sometimes a sign of infection).
Red-Flag Signs: When to Seek Urgent Care
Seek immediate medical attention if you experience any of the following symptoms:
- Severe pain that doesn’t improve with pain medication.
- High fever, chills, or signs of infection (may indicate a serious kidney infection).
- Inability to urinate or producing very little urine, which could signal a blockage.
- Persistent vomiting or signs of dehydration (dry mouth, weakness, dark urine).
- Blood clots in urine or intense pain on both sides of the body.
Prevention Tips for Kidney Stones
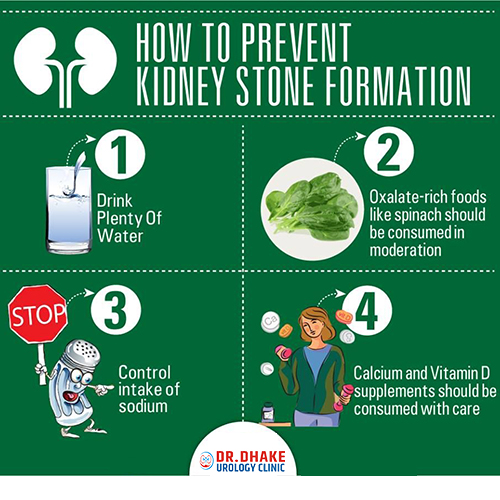
Preventing kidney stones involves making simple, consistent changes in hydration, diet, and lifestyle habits. Most kidney stones can be prevented or their recurrence greatly reduced through these proactive measures.
1. Stay Hydrated
Proper hydration keeps your urine diluted, reducing the concentration of minerals that can form stones.
- Drink 2–3 liters of fluids daily, unless otherwise advised by your doctor.
- Aim for light-colored urine throughout the day. Dark urine usually means you need more fluids.
- Increase fluid intake during hot weather, exercise, or heavy physical work.
- Water is best, but lemon water or citrus juices can also help by raising urinary citrate levels.
2. Smart Eating Habits
Diet plays a major role in kidney stone prevention. The goal is balance, not extreme restriction.
- Control salt: Excess sodium increases calcium in urine and promotes stones.
- Eat adequate calcium: Normal dietary calcium helps bind oxalate in the gut, preventing absorption into the bloodstream.
- Moderate animal protein: Too much meat increases uric acid and reduces protective citrate levels.
- Limit high-oxalate foods: Spinach, nuts, beets, and soy products should be eaten in moderation, especially if you’ve had calcium oxalate stones.
- Cut back on sugary drinks: High added sugar and cola-type sodas can raise stone risk.
- Include citrus fruits: Lemons, oranges, and limes naturally boost citrate in urine, reducing stone formation.
3. Maintain a Healthy Lifestyle
Everyday choices can significantly impact kidney health and stone risk.
- Maintain a healthy body weight through a balanced diet and regular activity.
- Exercise regularly to improve circulation and kidney function.
- Avoid long periods of sitting or inactivity, which can affect calcium balance.
- Treat urinary tract infections promptly to prevent infection-related (struvite) stones.
4. Targeted Prevention Based on Stone Type
Once your doctor determines the type of stone you form, specific strategies can help prevent recurrence:
| Stone Type | Targeted Prevention Strategy |
| Calcium oxalate stones | Balance calcium and oxalate intake; avoid excess salt and dehydration. |
| Uric acid stones | Limit red meat and alcohol; eat more fruits and vegetables to keep urine alkaline. |
| Cystine stones | Stay extremely well-hydrated (even at night) and use prescribed medications. |
| Struvite stones | Prevent urinary infections through timely diagnosis and treatment. |
Conclusion
Kidney stones are solid mineral buildups that develop when urine is highly concentrated. The main types are calcium oxalate, uric acid, struvite, and cystine stones. Common causes include dehydration, high sodium and protein diets, obesity, and metabolic disorders. Symptoms often include severe back pain, blood in urine, nausea, and frequent urination. Staying hydrated, limiting salt, balancing calcium intake, and eating more fruits and vegetables help prevent them. Early medical care is vital to avoid complications such as infection or kidney damage. Most stones can be prevented with consistent hydration and dietary balance.
FAQs
- How much water should I drink each day?
Aim for 2–3 liters (8–12 cups) of fluids daily, unless your doctor advises otherwise. Adjust your intake if you sweat a lot, exercise frequently, or live in a hot environment. Keep your urine light yellow or nearly clear to ensure proper hydration. - Do I need to avoid all high-oxalate foods?
No. Eat high-oxalate foods like spinach, nuts, and beets in moderation and pair them with calcium-rich foods such as milk or yogurt. Calcium binds oxalate in the gut, preventing it from reaching the kidneys. - Is bottled water better than tap water?
Clean tap water is usually fine if it meets safety standards. If your area’s tap water is very hard or unsafe, use filtered or bottled water instead. - How can I raise citrate levels naturally?
Include lemon or orange juice in your diet, eat more fruits and vegetables, and stay well hydrated. Citrate prevents crystals from forming by binding with calcium. - When should I go to the emergency room?
Seek immediate medical attention if you experience severe pain, fever or chills, little or no urine output, or persistent vomiting. These signs may indicate infection or blockage. - Do vitamin C or D supplements cause kidney stones?
High doses of vitamin C (over 1,000 mg/day) can increase oxalate levels, and excess vitamin D can raise calcium levels in urine. Take supplements only as advised by your doctor. - If I’ve had uric acid stones, what diet helps?
Limit red meat, organ meats, seafood, and alcohol. Eat more fruits and vegetables to make urine less acidic. Drink plenty of water and discuss medications like allopurinol with your doctor if recommended. - How often should I have follow-ups after passing a stone?
Schedule a follow-up within 6–12 months after passing a stone. Tests may include urine and blood analysis or imaging like ultrasound. Recurrent stone formers may need more frequent checkups. - Can I drink coffee or tea if I’ve had stones?
Yes, in moderation. Coffee and tea can be part of your fluid intake, but avoid excessive caffeine and sugary additives. Balance them with plenty of water. - What’s the safest imaging method to check for stones?
Ultrasound is the safest method because it’s radiation-free and effective for most cases. A CT scan may be used if more detail is needed. - Can kidney stones come back after treatment?
Yes. Kidney stones can recur in 30–50% of people within five years. Staying hydrated, adjusting your diet, and regular medical checkups help prevent recurrence. - Are kidney stones dangerous if untreated?
Yes. Untreated stones can block urine flow, cause infection, and lead to kidney damage. Prompt medical care prevents complications.
Reference
- “Kidney stones – Symptoms and causes” (Mayo Clinic)
https://www.mayoclinic.org/diseases-conditions/kidney-stones/symptoms-causes/syc-20355755 Mayo Clinic - “Eating, Diet, & Nutrition for Kidney Stones” (National Institute of Diabetes and Digestive and Kidney Diseases – NIDDK)
https://www.niddk.nih.gov/health-information/urologic-diseases/kidney-stones/eating-diet-nutrition NIDDK - “Kidney Stones: Causes, Symptoms, Diagnosis & Treatment” (Cleveland Clinic)
https://my.clevelandclinic.org/health/diseases/15604-kidney-stones Cleveland Clinic - “Kidney Stone Diet Plan and Prevention” (National Kidney Foundation)
https://www.kidney.org/kidney-topics/kidney-stone-diet-plan-and-prevention National Kidney Foundation - “Nephrolithiasis – Prevention” (BMJ Best Practice)
https://bestpractice.bmj.com/topics/en-gb/225/prevention
Dr. Amiah Rainey researches diet–disease relationships with expertise in vitamins, minerals, and biomarker methods. She earned a PhD from Harvard T.H. Chan School of Public Health (2019) and completed a postdoctoral fellowship at the NIH/NIDDK. With ~20 peer-reviewed publications (example) and experience on NIH-funded cohort studies, Amiah translates complex evidence into practical guidance. She advises on study design, evidence grading, and data transparency. Profiles: ORCID, Google Scholar; list affiliations and any disclosures.