Liver Detox: Fact or Fiction? How to Support Your Liver Naturally

The liver is your body’s natural detox powerhouse constantly filtering blood, breaking down waste, and neutralizing toxins to keep you healthy. It processes everything you eat, drink, and breathe, turning harmful substances into safer compounds that your body can easily eliminate. Beyond detoxification, it also supports digestion, stores vital nutrients, and helps regulate metabolism.
You don’t need expensive cleanses or trendy detox products to keep your liver working well. It already performs detoxification naturally and continuously. What really matters are simple, consistent habits: eating a balanced diet, limiting alcohol, staying hydrated, and getting regular health checkups. When you care for your liver through healthy choices, it does the rest keeping your body clean and balanced every day.
Key Takeaways
- The liver detoxifies the body every second, no external “cleanse” needed
- Most detox products lack scientific proof and may cause harm
- Alcohol, poor diet, and certain drugs are major liver stressors
- Balanced diet, hydration, and vaccines keep the liver strong
- Moderate coffee intake supports liver health naturally
- Regular health checks detect silent liver issues early
How the Liver Actually Detoxifies
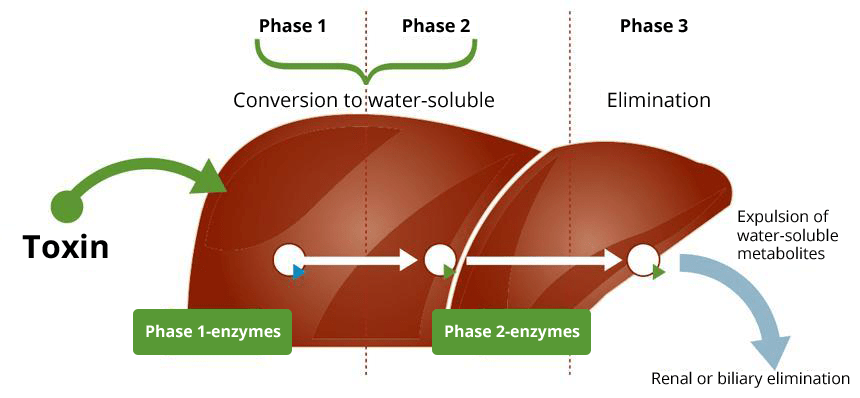
To understand why external detoxes aren’t necessary, it helps to know how the liver’s natural detox system works every day. This complex process runs nonstop, ensuring that harmful substances from food, medications, and the environment are safely broken down and removed. Each phase depends on specific enzymes and nutrients like amino acids, antioxidants, and vitamins that keep the system efficient and balanced.
- Phase One – Breaking Down Substances: Enzymes in liver cells modify chemicals, alcohol, and drugs, preparing them for further processing. This step transforms toxins into intermediate compounds, some of which may be more reactive.
- Phase Two – Neutralizing Toxins: The liver binds these reactive substances with molecules such as sulfur or glutathione, making them harmless, stable, and water-soluble. This step prevents buildup and protects liver cells from damage.
- Phase Three – Removing Them: Finally, the neutralized compounds are excreted from the body either through bile (which exits via stool) or filtered by the kidneys into urine.
Why “Liver Detox” Products Don’t Work
Detox teas, cleanses, and flushes are marketed with vague claims about removing toxins or resetting your body. No credible scientific study has shown that these products improve liver function or accelerate toxin removal.
In reality, some can harm your liver. Herbal ingredients such as kava, comfrey, and high-dose green tea extract have been linked to liver injury. Extreme fasting or laxative-based detoxes may cause dehydration, electrolyte imbalance, or nutrient loss.
These products offer no benefits for a healthy liver and can worsen damage if the liver is already compromised. They also waste money and may lead to unhealthy restriction cycles.
What Actually Harms Your Liver
Instead of searching for toxins to flush, it’s better to understand what truly causes liver damage in everyday life.
- Alcohol: Excessive drinking leads to fat buildup, inflammation, and eventually scarring (cirrhosis). Even moderate drinkers benefit from having a few alcohol-free days each week to give the liver time to recover.
- Acetaminophen (Paracetamol): Safe when used as directed but dangerous in large doses. Exceeding 3,000–4,000 mg per day or combining it with alcohol can trigger acute liver failure. Always check medication labels carefully.
- Hepatitis Viruses: Hepatitis B and C infections can silently damage the liver for years without symptoms. Vaccination (for Hepatitis B) and early screening (for Hepatitis C) are crucial for prevention and treatment.
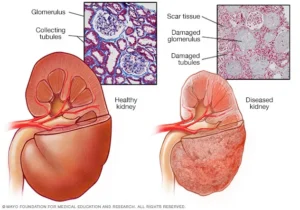
- Fatty Liver Disease: Caused by poor diet, obesity, and insulin resistance, this condition is now one of the most widespread liver disorders globally. It can progress to inflammation, fibrosis, or cirrhosis if untreated.
Common Liver Detox Myths vs. Facts
Before trusting every “detox” trend, it’s important to separate fact from marketing fiction. Many popular beliefs about liver health sound convincing but aren’t backed by science. Understanding these myths helps you make smarter, safer choices for your liver and overall well-being.
| Myth | Fact |
| You need a yearly detox. | The liver detoxifies the body continuously; it doesn’t require cleanses or resets. |
| Teas and supplements can reverse liver damage. | No over-the-counter product heals scarring or chronic inflammation; only medical care and lifestyle changes help. |
| You can judge liver health by how you feel. | Liver disease often shows no symptoms until advanced; only routine blood tests reveal issues early. |
| Natural equals safe. | Many herbs and “natural” ingredients can harm the liver, especially in high doses or poor-quality supplements. |
How to Support Your Liver Naturally
Supporting your liver doesn’t require expensive detoxes or miracle supplements. The key lies in maintaining healthy habits that reduce strain and allow this vital organ to do its job effectively. Here are practical ways to care for your liver naturally:
- Limit Alcohol and Give It Breaks: Alcohol is one of the most common causes of preventable liver disease. Regular overconsumption can lead to inflammation, fatty liver, or even cirrhosis. Try to have at least two to three alcohol-free days each week and avoid binge drinking. If you find it hard to cut back, seek medical or counseling support and your liver will thank you.
- Use Medications Safely: Many over-the-counter painkillers and cold remedies contain acetaminophen (paracetamol), which can harm the liver if overused or mixed with alcohol. Always read medication labels, follow dosage guidelines, and talk to your doctor if you take several prescriptions or supplements regularly.
- Get Vaccinated and Screened: Vaccinations and early detection are powerful forms of prevention.Hepatitis B, A vaccine offers lifelong protection. Hepatitis C, A simple blood test can detect it, and modern treatments can cure more than 95% of cases. Hepatitis A, Especially important for travelers or those with existing liver issues.
- Maintain a Healthy Weight: Excess body fat, especially around the abdomen, increases the risk of fatty liver disease. Even a modest 5–10% reduction in weight can improve liver fat levels and reduce inflammation. Sustainable lifestyle habits, regular exercise, adequate sleep, and mindful eating work best over time.
- Eat a Balanced Diet: A nutrient-rich diet supports liver repair and function. Focus on fruits, vegetables, legumes, whole grains, lean proteins, nuts, and olive oil. Limit processed meats, sugary foods, fried items, and trans fats. Choose whole grains and beans for steady blood sugar and lean proteins to maintain muscle mass while losing weight. Balance and variety matter more than strict restriction.
- Drink Coffee: Research shows that drinking 2–3 cups of regular or decaf coffee daily may protect against liver fibrosis and cirrhosis. Coffee’s natural antioxidants seem to play a role, not caffeine itself. Just avoid adding excessive sugar or creamers.
- Stay Hydrated and Limit Sugary Beverages: Water helps the liver filter toxins and transport nutrients. Replace sugary sodas, energy drinks, or packaged juices with plain water, infused water (like lemon or cucumber), or unsweetened herbal tea. Hydration supports every aspect of liver function.
- Be Cautious With Supplements and Herbs: Natural doesn’t always mean safe. Some herbal or “detox” products can stress or damage the liver. While herbs like milk thistle and turmeric show mild benefits in studies, their results are inconsistent. Avoid high doses or unverified supplements, and always consult your doctor before starting any new product.
- Protect Yourself From Environmental Exposure: Chemicals from paints, cleaning agents, or industrial products can be absorbed through the skin or inhaled. Use gloves, masks, and proper ventilation when handling such materials to reduce long-term exposure risks.
- Manage Stress and Sleep: Chronic stress and poor sleep disrupt hormone balance and metabolism, indirectly affecting liver health. Aim for 7–8 hours of sleep each night and practice relaxation techniques like yoga, meditation, or walking outdoors. A calmer mind often leads to a healthier body and liver.
Medical Approaches to Liver Support
When lifestyle measures aren’t enough or when liver disease is present, medical management plays a key role in supporting liver function and preventing progression. Treatment depends on the underlying cause and the stage of liver impairment.
1. Medication Management
Doctors may prescribe or adjust medications to reduce liver inflammation, control metabolic factors, or treat specific liver conditions:
- Antivirals for hepatitis B or C to prevent viral replication and liver damage.
- Insulin sensitizers (like metformin) for metabolic-associated steatotic liver disease (MASLD).
- Corticosteroids or immunosuppressants for autoimmune hepatitis.
- Chelation therapy for genetic conditions such as Wilson’s disease (copper buildup).
- Ursodeoxycholic acid (UDCA) for cholestatic liver diseases like primary biliary cholangitis.
2. Monitoring and Screening
Regular medical checkups help detect liver damage early and track disease progression:
- Liver function tests (LFTs) to measure enzymes and bilirubin levels.
- Ultrasound or FibroScan to assess fat accumulation or fibrosis.
- Blood markers and imaging for early detection of cirrhosis or liver cancer (hepatocellular carcinoma).
3. Nutritional and Supplement Guidance
Medical professionals may recommend specific dietary changes or supplements under supervision:
- Vitamin D, E, or zinc for deficiency-related liver issues.
- Avoiding unverified “liver detox” supplements, which can cause toxicity.
- Consultation with a dietitian to manage calorie intake, protein balance, and metabolic risk factors.
4. Managing Complications
In advanced liver disease, treatment focuses on controlling symptoms and preventing further injury:
- Diuretics and low-sodium diets for fluid buildup (ascites).
- Lactulose for hepatic encephalopathy (to reduce toxin buildup).
- Endoscopic or surgical treatments for variceal bleeding.
5. Liver Transplantation
When irreversible liver failure occurs, liver transplantation becomes the definitive option. Advances in surgical techniques and immunosuppressive therapy have significantly improved outcomes and survival rates.
Signs You Should See a Doctor
Although the liver can regenerate and handle a significant workload, many liver problems develop quietly over time. Often, noticeable symptoms only appear once substantial damage has occurred. Recognizing these early warning signs and seeking prompt medical attention can make a major difference in outcomes. If you experience any of the following symptoms, it’s important to consult a healthcare professional as soon as possible:
- Yellowing of the skin or eyes (jaundice): This occurs when bilirubin builds up in the blood, indicating that the liver isn’t processing it properly. It’s one of the most visible and serious signs of liver distress.
- Dark urine or pale stools: These changes suggest disruptions in bile production or flow, often linked to liver or gallbladder dysfunction.
- Persistent fatigue or nausea: Chronic tiredness, loss of appetite, or unexplained nausea can signal impaired liver metabolism or toxin buildup in the body.
- Pain or swelling in the upper right abdomen: The liver sits in the upper right side of the abdomen; discomfort or fullness here can indicate inflammation, enlargement, or fluid accumulation.
- Easy bruising, confusion, or swelling in the legs and abdomen: These may reflect advanced liver disease, where the liver can no longer produce enough proteins for blood clotting or manage fluid balance effectively. Confusion can occur when toxins affect brain function, a condition known as hepatic encephalopathy.
Conclusion
Your liver doesn’t need detox teas or cleanses, it needs smart daily care. The real detox happens when you avoid what harms it and strengthen what supports it. Limit alcohol, use medications safely, eat a balanced diet, and stay hydrated. Vaccinate against hepatitis, get regular checkups, and maintain a healthy weight. Habits like moderate coffee intake, physical activity, and good sleep protect your liver better than any supplement ever could. The liver works tirelessly to detoxify your body every second; your role is to help it do that efficiently through consistent, healthy choices.
Frequently Asked Questions
- Do liver cleanses remove toxins?
No. Your liver naturally filters and neutralizes toxins on its own. Cleanses or detox teas don’t speed this process and may even irritate your system. - Is a short juice fast safe for the liver?
A one-day light juice fast is generally safe, but longer juice diets can deprive your body of protein and essential nutrients, putting stress on the liver. - Which tests check liver health?
Common tests include ALT, AST, ALP, bilirubin, and GGT. These help detect early signs of inflammation, blockage, or liver cell damage. - Can coffee really protect the liver?
Yes. Drinking two to three cups of coffee daily has been linked to lower risks of fibrosis and liver cancer due to its antioxidant compounds. - Are detox teas or supplements safe with medications?
Not always. Many herbal ingredients can interact with prescription drugs or harm the liver. It’s safest to check with your doctor before using them. - What’s the safe limit for acetaminophen?
Keep intake below 3,000 mg per day and avoid alcohol while taking it. Even slight overdoses can cause serious liver injury or failure. - Can fatty liver be reversed?
Yes. Losing weight gradually, staying active, and eating a balanced diet can reverse fatty liver and reduce inflammation over time. - How long does it take the liver to recover after quitting alcohol?
Fat and inflammation start to improve within a few weeks, though healing from scarring or fibrosis may take several months. - Do colon cleanses help liver detox?
No. The liver and colon have separate detox roles, and cleansing the colon does not improve liver function or toxin removal. - Is decaf coffee still beneficial?
Yes. Decaf coffee retains many protective antioxidants found in regular coffee, offering similar liver benefits without caffeine.
Reference
- https://www.nccih.nih.gov/health/detoxes-and-cleanses-what-you-need-to-know
- https://www.hopkinsmedicine.org/health/wellness-and-prevention/detoxing-your-liver-fact-versus-fiction
- https://www.health.harvard.edu/staying-healthy/the-dubious-practice-of-detox
- https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-021-10991-7
- https://www.gimed.net/blog/the-truth-about-liver-detox-diets/
Dr. Amiah Rainey researches diet–disease relationships with expertise in vitamins, minerals, and biomarker methods. She earned a PhD from Harvard T.H. Chan School of Public Health (2019) and completed a postdoctoral fellowship at the NIH/NIDDK. With ~20 peer-reviewed publications (example) and experience on NIH-funded cohort studies, Amiah translates complex evidence into practical guidance. She advises on study design, evidence grading, and data transparency. Profiles: ORCID, Google Scholar; list affiliations and any disclosures.