Everything You Need to Know About Your Liver Health
The liver is a vital organ managing metabolism, detoxification, immunity, and nutrient storage. Despite its size, it performs hundreds of functions daily, filtering toxins, processing nutrients, producing bile, and regenerating damaged tissue to maintain overall health.
Key Takeaways on Liver Health
- The liver has dual blood supply and specialized cells (hepatocytes, Kupffer, stellate) for metabolism, detox, and immune defense.
- Main functions include energy balance, bile production, detoxification, nutrient storage, and protein synthesis.
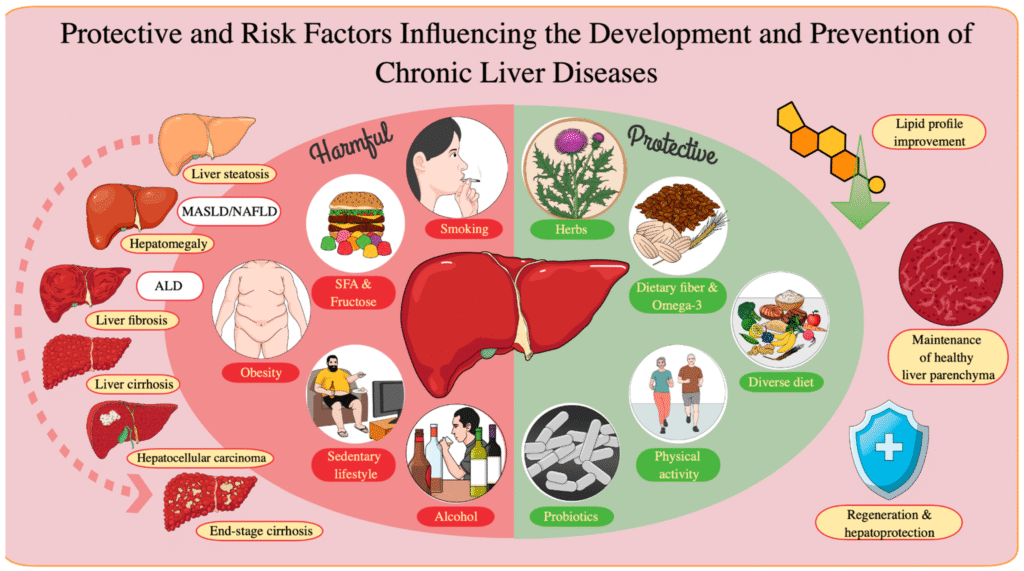
- Major risks: viral infections, excessive alcohol, metabolic fatty liver (MASLD), drugs, poor diet, and genetic disorders.
- Early liver disease is often silent; subtle symptoms include fatigue, nausea, appetite loss, mild abdominal discomfort, or bloating.
- Disease progression: fatty liver, inflammation, fibrosis, cirrhosis, liver failure or cancer.
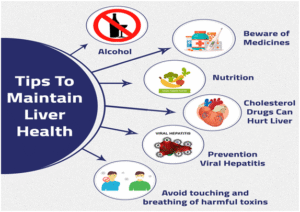
- Prevention: balanced diet, exercise, weight control, limited alcohol, vaccinations, stress management, regular check-ups, and cautious medication use.
How the Liver Works in Your Body
The liver operates like a central hub, receiving, processing, and distributing everything that enters your body, ensuring each system runs smoothly and stays in balance.
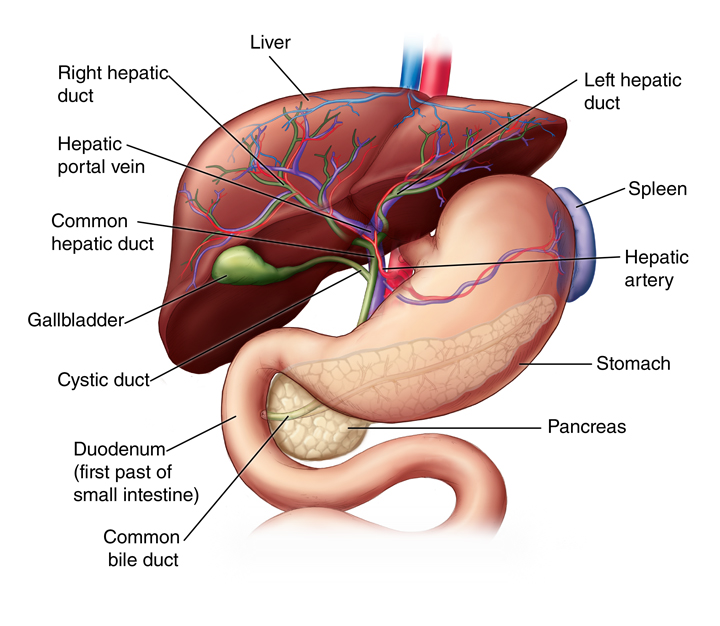
Blood supply
The liver has a unique dual blood supply. One line, the hepatic artery, brings in oxygen-rich blood from the heart. The other, the portal vein, carries nutrient-rich blood from your stomach and intestines. This setup ensures the liver receives everything it needs both oxygen and raw materials to process and distribute nutrients efficiently.
Functional units
Inside the liver are millions of tiny, repeating units called lobules. You can think of each lobule as a small work cell filled with specialized workers called hepatocytes. These cells handle critical tasks such as converting nutrients into usable forms, storing sugar as glycogen, and detoxifying chemicals or medications. Blood flows through the lobules in a specific pattern, allowing the hepatocytes to filter and modify it before it exits through the hepatic vein.
Support cells
Alongside hepatocytes, the liver contains other important cell types. Kupffer cells act like tiny guards that trap bacteria and waste, keeping your blood clean. Stellate cells store vitamin A and help repair tissue if the liver gets injured, though if they become overactive during chronic damage, they can also form scar tissue.
Together, these cells make the liver both powerful and resilient. It can even regenerate if part of the liver is removed or injured, the remaining tissue can grow back to its original size. This ability makes it one of the most adaptable organs in the human body.
Major Functions of the Liver
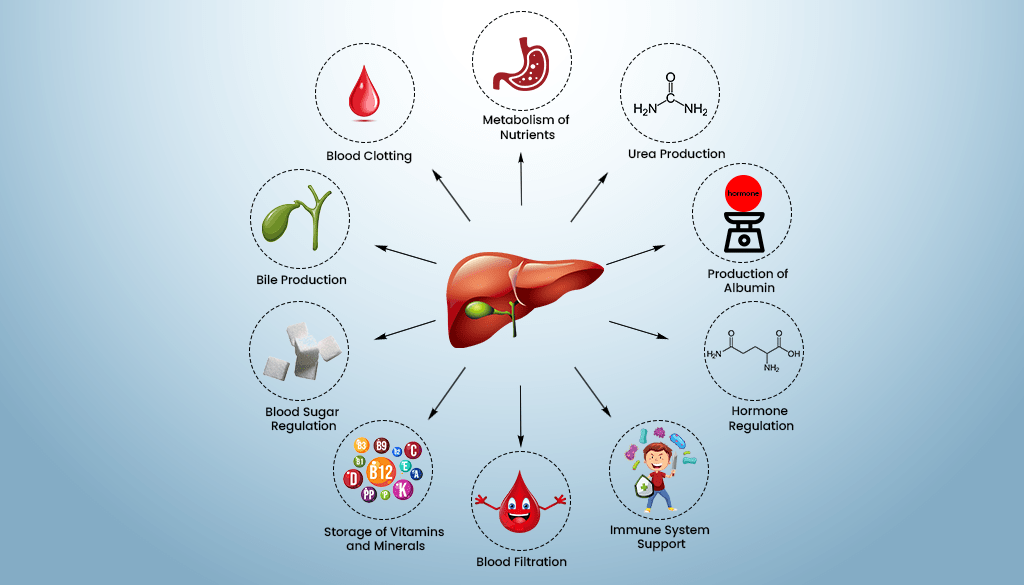
The liver carries out more than 500 essential functions. Most of these can be grouped into five main categories that sustain metabolism, immunity, and detoxification.
1. Metabolism and Energy Balance
Your liver decides how your body uses and stores energy.
- Converts carbohydrates into glucose and stores it as glycogen.
- Breaks down fats into energy and produces cholesterol used for hormones.
- Helps balance amino acids from protein for repair and growth.
2. Detoxification
The liver filters out chemicals, alcohol, drugs, and by-products of metabolism. It converts harmful substances into harmless ones for elimination through bile or urine.
- Neutralizes ammonia into urea.
- Breaks down medications and alcohol safely.
- Handles phase I and II detox reactions that neutralize toxins.
3. Bile Production and Digestion
Bile is a digestive fluid produced by the liver and stored in the gallbladder. Its main role is to break down fats in the small intestine, making them easier to absorb. Bile also helps remove waste products from the body, including excess cholesterol and bilirubin, a by-product of red blood cell breakdown. Proper bile flow is essential for efficient digestion and nutrient absorption. When bile flow is reduced or blocked, it can lead to indigestion, bloating, diarrhea, or deficiencies in fat-soluble vitamins like A, D, E, and K. Maintaining liver and gallbladder health through diet, hydration, and avoiding excessive alcohol or fatty foods helps ensure bile is produced and released effectively, supporting digestion and overall metabolic balance.
4. Storage and Synthesis
The liver acts as a warehouse, storing vitamins A, D, E, K, and minerals like iron and copper. It also produces important proteins such as:
- Albumin: Maintains fluid balance in blood.
- Clotting factors: Help stop bleeding.
5. Immune and Protective Role
The liver doesn’t just process nutrients it also acts as a key immune organ. Kupffer cells, specialized immune cells within the liver, patrol the blood that flows through it. They capture and destroy bacteria, viruses, and old or damaged blood cells, preventing infections and keeping the bloodstream clean. By removing harmful particles before they spread through the body, Kupffer cells help regulate and balance the immune system. This filtering function also supports overall health by reducing inflammation and protecting other organs from damage caused by toxins or pathogens. Essentially, the liver acts like a frontline defense checkpoint, combining metabolism and immunity in one organ.
Major Causes and Risk Factors of Liver Damage
Liver problems rarely happen overnight. They often develop slowly and quietly, sometimes showing no symptoms for years. Understanding what harms the liver helps you take early steps to protect it and prevent irreversible damage.
1. Viral Infections
Certain viruses directly attack liver cells and cause inflammation. The most common are Hepatitis A, B, and C.
- Hepatitis A usually spreads through contaminated food or water and often resolves without lasting damage.
- Hepatitis B and C, however, spread through infected blood or body fluids and can become chronic.
2. Alcohol Consumption
The liver is the main organ responsible for breaking down alcohol. But it can only process a limited amount at a time. Excessive drinking forces liver cells to convert alcohol into harmful substances like acetaldehyde, which inflames and damages tissue.
With continued heavy use, this damage progresses through stages:
- Fatty liver (steatosis): the earliest and most reversible stage
- Alcoholic hepatitis: inflammation and cell injury
- Cirrhosis: ermanent scarring and loss of function
Even moderate drinking over many years can slowly weaken the liver’s ability to heal itself.
Knowing the impact of alcohol on liver health helps in setting safe consumption limits and preventing long-term damage.
3. Metabolic Fatty Liver Disease
Previously known as non-alcoholic fatty liver disease (NAFLD), this condition is now called metabolic dysfunction-associated steatotic liver disease (MASLD). It’s closely linked to obesity, insulin resistance, high blood sugar, and high cholesterol. When too much fat builds up inside liver cells, the organ becomes swollen and inflamed. Over time, this can progress to metabolic steatohepatitis (MASH), which can cause scarring similar to alcohol-related liver disease. Because it develops quietly, many people only discover it during routine blood tests or imaging. Regular exercise, balanced diet, and blood sugar control are the most effective preventive measures.
4. Drug and Chemical Damage
The liver filters and breaks down medications, chemicals, and supplements but excessive or improper use can overwhelm it.
- Acetaminophen (paracetamol) overdose is the most common cause of sudden liver failure.
- Long-term or high-dose use of painkillers, steroids, antibiotics, or herbal remedies can also harm liver cells.
5. Poor Diet and Lifestyle
Unhealthy habits often place quiet but steady stress on the liver. Diets high in sugar, refined carbs, and processed foods promote fat buildup inside liver cells. Sedentary lifestyles, irregular sleep, and chronic stress further disrupt metabolism, reducing the liver’s ability to clear toxins and manage fats. Over time, these combined factors can lead to fatty liver, insulin resistance, and inflammation, a chain reaction that raises long-term disease risk.
6. Genetic Disorders
A small number of liver diseases are inherited.
- Hemochromatosis causes the body to absorb too much iron, which accumulates in the liver and other organs.
- Wilson’s disease leads to copper buildup, which damages the liver and brain if untreated.
Recognizing Symptoms of Liver Disease
Liver disease is often called a “silent condition” because it can develop slowly without obvious signs. Many people feel perfectly fine in the early stages, which is why knowing subtle warning signals is critical. Early detection allows treatment before serious damage occurs.
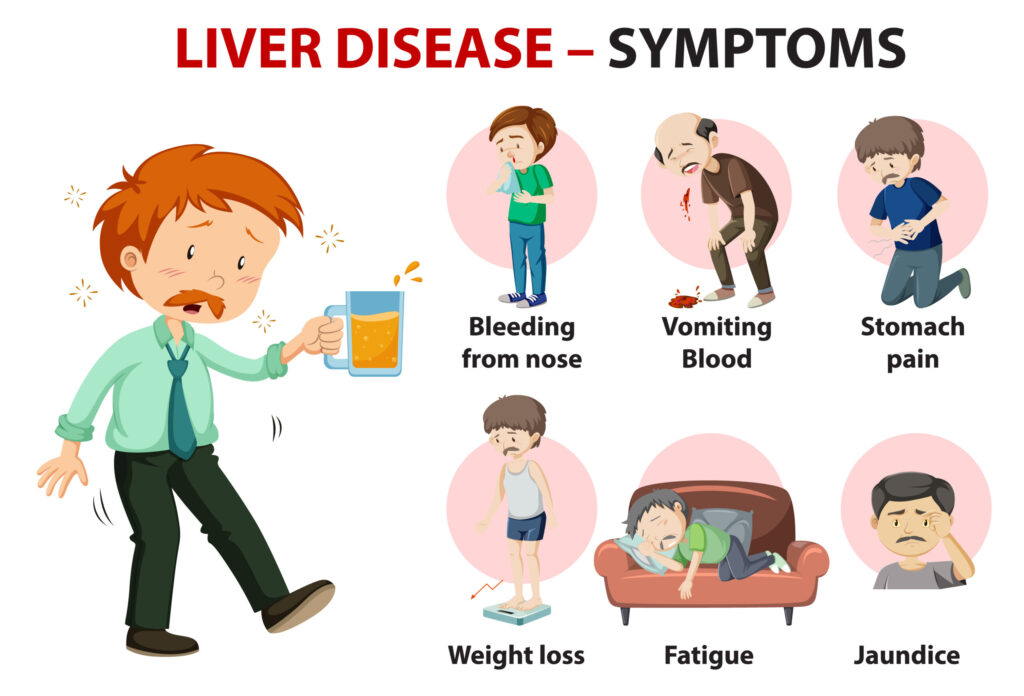
Early Symptoms
In the initial phase, liver problems may produce mild or vague symptoms that are easy to overlook:
- Tiredness and weakness: Feeling unusually fatigued despite normal rest can indicate the liver is struggling to manage energy.
- Loss of appetite: Reduced interest in food may result from changes in liver metabolism and toxin buildup.
- Mild nausea or abdominal discomfort: Slight digestive discomfort, especially in the upper right abdomen, can reflect liver inflammation or enlargement.
- Subtle bloating or right-side heaviness: A feeling of fullness or heaviness near the liver may be an early sign of swelling or fat accumulation.
Progressive or Advanced Symptoms
As liver damage worsens, signs become more noticeable and may indicate serious complications:
- Yellowing of the skin or eyes (jaundice): Caused by bilirubin buildup when the liver cannot process waste properly.
- Dark urine, pale stools: Changes in excretion reflect impaired bile production or flow.
- Persistent itching: Toxins accumulating in the skin may trigger constant itchiness.
- Swelling in legs or abdomen (ascites): Fluid buildup occurs when the liver cannot manage blood protein levels and pressure.
- Easy bruising or bleeding: Reduced production of clotting factors increases bleeding risk.
- Confusion or poor concentration (hepatic encephalopathy): Toxins affecting brain function can cause mental fog, memory problems, and mood changes.
Stages of Liver Disease
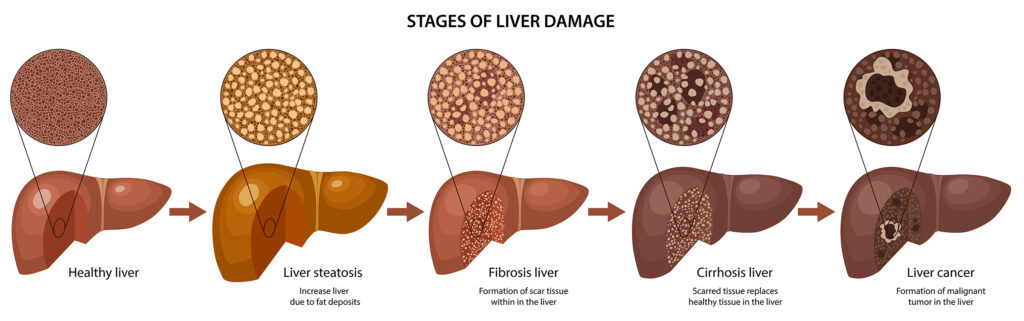
Liver damage usually develops gradually and follows a predictable progression, although the speed varies between individuals. Understanding the stages helps identify problems early and take steps to prevent permanent damage.
1. Fatty Liver (Steatosis)
This is the earliest stage, where fat starts accumulating inside liver cells. Most people do not experience symptoms at this point. Fortunately, it is often reversible through:
- Healthy diet and regular exercise
- Reducing sugar and processed foods
- Maintaining a healthy weight
If addressed early, the liver can recover fully without lasting damage.
2. Inflammation (Steatohepatitis)
When fat buildup triggers irritation, the liver becomes inflamed. This stage is called steatohepatitis, which can be caused by alcohol (alcoholic steatohepatitis) or metabolic factors (non-alcoholic). Chronic inflammation starts to injure liver cells and may cause mild fatigue, abdominal discomfort, or slightly elevated liver enzymes in blood tests.
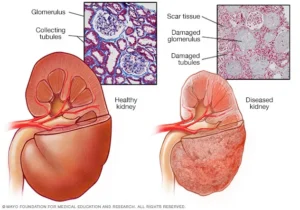
3. Fibrosis
The liver attempts to repair itself from ongoing inflammation, forming scar tissue called fibrosis. Initially, scar tissue is limited, but over time it accumulates, making the liver stiffer and less efficient. Lifestyle changes and medical treatment at this stage can slow or stop progression.
4. Cirrhosis
Cirrhosis occurs when scarring becomes widespread, permanently affecting liver function. Blood flow through the liver is disrupted, toxins build up, and the risk of serious complications rises, including fluid retention (ascites), variceal bleeding, and mental confusion (hepatic encephalopathy).
5. Liver Failure or Cancer
In the most advanced stage, liver cells can no longer perform essential functions, leading to liver failure. Chronic cirrhosis or long-standing hepatitis infections also increase the risk of hepatocellular carcinoma (HCC), the most common type of liver cancer. At this stage, medical intervention, including transplantation, may be required.
How Liver Diseases Are Diagnosed
Early detection is key to preventing irreversible liver damage. Diagnosis typically involves a combination of blood tests, imaging, and sometimes biopsy.
1. Blood Tests
Blood tests assess how well the liver is functioning and detect early cell damage:
- ALT and AST: Enzymes that rise when liver cells are injured.
- Bilirubin: Measures how efficiently the liver clears waste.
- Albumin and INR: Indicate the liver’s ability to produce proteins and support blood clotting.
2. Imaging Tests
Imaging helps visualize structural changes in the liver:
- Ultrasound: Detects fat accumulation, swelling, or early cirrhosis.
- Elastography: Measures liver stiffness to identify scarring levels.
- CT/MRI: Provides a detailed view when more precision is needed for diagnosis or planning treatment.
3. Liver Biopsy
In certain cases, doctors may take a small tissue sample for microscopic examination. A biopsy provides definitive information about inflammation, fibrosis, or cirrhosis and helps guide treatment decisions.
4. Monitoring and Follow-Up
After initial diagnosis, doctors often repeat blood tests or imaging every few months to track disease progression or improvement. Monitoring ensures timely intervention if the condition worsens.
Prevention and Daily Liver Care
Keeping your liver healthy doesn’t require complicated routines. Consistency in everyday habits and smart choices can protect your liver and prevent disease. Small, manageable daily actions often make the biggest difference. Adopt liver-friendly lifestyle habits like exercise, quality sleep, and stress management. Avoid risks of diet sodas and processed foods for liver health to reduce fat buildup and inflammation.
1. Eat a Liver-Friendly Diet
Nutrition has a direct impact on liver health. Whole, minimally processed foods provide nutrients without overloading the liver with toxins or sugars. Key components include:
- Fresh vegetables and fruits: Rich in antioxidants, they help neutralize free radicals that can damage liver cells and reduce inflammation. Examples include broccoli, spinach, carrots, and berries.
- Lean proteins: Chicken, fish, tofu, and legumes provide amino acids that repair liver tissue without adding unhealthy fat.
- Healthy fats: Olive oil, nuts, seeds, and fatty fish supply omega-3 fatty acids, which reduce inflammation and support fat metabolism in the liver.
- Whole grains: Foods like oats, brown rice, and quinoa stabilize blood sugar and prevent excessive fat accumulation in liver cells.
- Reduce sugary drinks and artificial sweeteners: Soda, sweetened teas, and energy drinks can increase liver fat and stress metabolic pathways.
- Antioxidant-rich foods: Berries, leafy greens, green tea, and certain herbs help support detoxification and liver metabolism.
Adopting this dietary approach strengthens the liver’s natural ability to process nutrients, eliminate toxins, and maintain energy balance.
2. Maintain a Healthy Weight
Carrying excess body fat, especially around the abdomen, increases the risk of fatty liver and inflammation. Even a modest weight loss of 5–10% of total body weight can significantly reduce fat buildup, lower inflammation, and improve liver enzyme levels. Maintaining a healthy weight also improves insulin sensitivity, which protects the liver from metabolic stress.
3. Exercise Regularly
Physical activity enhances liver function by helping metabolize fats, regulate blood sugar, and reduce fat deposits. Aim for 150 minutes of moderate-intensity exercise per week, such as brisk walking, swimming, or cycling. Exercise also helps prevent obesity and insulin resistance, two major contributors to fatty liver disease.
4. Avoid Excess Alcohol
Alcohol is processed primarily by the liver, and even small amounts consumed daily can accumulate over time, causing liver stress. Taking alcohol-free days each week gives the liver a chance to recover, reducing the risk of fatty liver, alcoholic hepatitis, or cirrhosis. For those with existing liver problems, avoiding alcohol entirely is essential.
5. Limit Medications and Toxins
Many medications and supplements are metabolized in the liver, which can strain the organ if overused. Key precautions include:
- Follow dosage instructions carefully.
- Avoid mixing alcohol with medications.
- Be cautious with herbal supplements or high-dose vitamins, as some can be toxic to the liver in large amounts.
Minimizing unnecessary exposure to toxins allows the liver to focus on essential metabolic and detoxification tasks.
6. Get Vaccinated
Vaccines for hepatitis A and B protect the liver from viral infections that can cause long-term damage or chronic liver disease. Vaccination is especially important for high-risk groups such as healthcare workers, travelers to endemic regions, and people with existing liver conditions.
7. Manage Stress and Sleep
Chronic stress and poor sleep contribute to inflammation and disrupt liver metabolism. Prioritizing 7–9 hours of quality sleep per night and practicing stress-reducing techniques such as meditation, yoga, deep breathing, or mindful walking helps maintain liver health and overall metabolic balance.
8. Regular Check-Ups
Annual liver function tests and imaging can detect early liver changes before symptoms appear. Early intervention allows lifestyle adjustments or medical treatments to prevent disease progression, often stopping liver damage before it becomes serious.
Treatment Options and Medical Care
How liver disease is treated depends largely on the type of liver problem and its stage. Early detection and lifestyle adjustments can often reverse damage, but advanced disease may require medical interventions to prevent serious complications.
1. Fatty Liver and MASLD
For liver disease caused by metabolic issues, such as metabolic dysfunction-associated steatotic liver disease (MASLD), lifestyle interventions are the main treatment:
- Weight loss and a healthy diet: Reducing excess body fat decreases liver fat and inflammation. A diet rich in whole foods, vegetables, lean protein, and healthy fats supports recovery.
- Managing blood sugar, cholesterol, and blood pressure: Controlling these metabolic factors reduces stress on the liver and lowers the risk of progression to inflammation or scarring.
2. Hepatitis
Viral infections such as hepatitis B and C require medical treatment:
- Hepatitis B: Antiviral medications suppress viral replication and reduce liver inflammation, preventing long-term complications.
- Hepatitis C: Modern short-course antiviral therapies can cure the infection in most cases, stopping disease progression and significantly lowering the risk of liver cancer.
3. Cirrhosis Management
When liver scarring (cirrhosis) occurs, treatment focuses on preventing complications:
- Reduce salt intake: Helps prevent fluid buildup in the abdomen (ascites).
- Medications: May be prescribed to reduce the risk of bleeding, infections, or fluid retention.
- Avoid alcohol and unnecessary drugs: Protects remaining liver tissue from further damage.
4. Liver Transplant
In cases of end-stage liver failure or liver cancer, a liver transplant may be the only life-saving option.
- The liver’s unique ability to regenerate allows partial donor livers to grow and restore full function in recipients.
- Transplantation significantly improves survival and quality of life, but requires lifelong follow-up and immunosuppressive therapy.
5. New and Emerging Treatments
Medical research continues to explore advanced therapies to repair or slow liver damage:
- Stem cell therapy: Potential to regenerate damaged liver tissue.
- Antifibrotic drugs: Aim to reduce scar formation and prevent cirrhosis progression.
- Metabolic regulators: Target the root causes of fat accumulation, insulin resistance, and inflammation to improve liver function.
For more awareness on liver cancer prevention and early detection, early diagnosis and monitoring are key.
Living Well with Liver Disease
Living with a liver condition can feel overwhelming, but with proper care and lifestyle management, many people lead full, active, and productive lives. Understanding daily habits, emotional health, and long-term outlook is key to maintaining quality of life.
Day-to-Day Management Tips
Managing liver disease daily involves following medical guidance and making small, consistent lifestyle adjustments:
- Follow prescribed medication and diet plans: Take medications exactly as directed and adhere to dietary recommendations to reduce liver stress.
- Stay hydrated and eat small, balanced meals: Frequent, moderate meals help maintain energy and prevent metabolic overload on the liver.
- Avoid smoking and limit caffeine: Both can increase liver stress and interfere with metabolic balance.
- Track lab results and symptoms: Keep a personal health log to monitor changes and report concerns promptly to your doctor.
- Stay updated on vaccinations and medical checkups: Regular health monitoring prevents complications and detects early changes in liver function.
These habits support liver function naturally , reduce the risk of complications, and empower patients to take control of their health.
Emotional and Social Health
Chronic liver disease can affect mental and emotional well-being. Patients may experience anxiety, stress, or feelings of isolation. Support is essential:
- Counseling and therapy: Professional guidance helps manage emotional challenges.
- Support groups and community programs: Sharing experiences with others facing similar conditions can reduce stress and provide practical coping strategies.
- Family and social support: Encouragement from loved ones improves adherence to treatment and quality of life.
Outlook and Prognosis
The long-term outlook depends on the stage of liver disease and the underlying cause:
- Early-stage liver disease: Fatty liver or mild inflammation can often be reversed with diet, exercise, and lifestyle changes.
- Moderate liver damage: With consistent medical care, progression can be slowed, and complications minimized.
- Advanced disease: Even in cirrhosis or chronic hepatitis, disciplined lifestyle management, timely medical interventions, and monitoring improve survival rates and maintain quality of life.
Understanding the connection between diabetes and liver health is also important, as diabetes increases liver risk.
Conclusion
The liver is a powerhouse organ responsible for over 500 functions, including energy metabolism, detoxification, bile production, nutrient storage, and immune defense. Damage develops slowly from viral infections, alcohol, fatty liver, drugs, poor diet, or genetics. Early signs are often subtle: fatigue, nausea, mild abdominal discomfort, or bloating. Progressive damage can lead to fibrosis, cirrhosis, liver failure, or cancer. Prevention focuses on a balanced diet, exercise, maintaining healthy weight, limiting alcohol, managing medications, vaccinations, stress reduction, and regular check-ups. Early detection allows effective lifestyle or medical interventions, while the liver’s regenerative capacity offers remarkable recovery if cared for promptly.
Frequently Asked Questions
- What are the first warning signs of liver trouble?
Early liver problems are often subtle and easy to overlook. Common warning signs include persistent fatigue, unexplained nausea, loss of appetite, mild abdominal discomfort, bloating, or yellowing of the eyes and skin (jaundice). These indicate that the liver is struggling to process toxins, manage metabolism, or produce bile efficiently. Catching these early can prevent more serious damage. - Can the liver repair itself naturally?
Yes, the liver is remarkably resilient. It can regenerate new cells and restore its function if damage is detected early and the underlying cause such as alcohol, poor diet, or infection is addressed. This regenerative ability is why lifestyle changes and medical treatment can reverse many early-stage liver conditions. - How much alcohol is safe for the liver?
No level of alcohol is entirely risk-free. Even moderate consumption over time can slowly stress the liver. Limiting intake to occasional, small servings and including alcohol-free days allows the liver to recover and reduces the risk of fatty liver, inflammation, or long-term damage. - Are sugar-free sodas or artificial sweeteners bad for the liver?
Yes, overconsumption can still burden the liver. Artificial sweeteners, chemical additives, and certain metabolic by-products force the liver to work harder, potentially leading to fat buildup, inflammation, or metabolic stress over time. Moderation is key. - Is fatty liver reversible?
In most cases, yes. Fatty liver caused by metabolic issues, poor diet, or obesity can often be reversed through weight loss, balanced nutrition, and regular exercise. Early intervention is crucial to prevent progression to inflammation, fibrosis, or cirrhosis. - What foods cleanse or support the liver naturally?
Certain foods help detoxify and strengthen liver function, including leafy greens, garlic, turmeric, green tea, cruciferous vegetables, and fiber-rich foods. These foods support bile production, reduce inflammation, and help the liver process toxins efficiently. Incorporating foods that support liver health into your daily diet strengthens detoxification and reduces inflammation. - How often should I check my liver function?
For healthy adults, an annual liver function test is recommended. Those who drink alcohol, take medications regularly, have diabetes, or other risk factors should check more frequently to detect early changes before symptoms appear. - What are the worst habits for liver health?
Excessive alcohol, diets high in processed foods and sugar, chronic stress, poor sleep, and sedentary lifestyles all place steady stress on the liver. Over time, these habits contribute to fat buildup, inflammation, insulin resistance, and other liver problems. - Can liver disease exist without symptoms?
Yes, many liver conditions progress silently for years. Fatty liver, viral hepatitis, and other chronic liver issues often show no noticeable symptoms in the early stages, which is why routine monitoring is essential. - When should I see a doctor about my liver?
Medical attention is necessary if you experience persistent fatigue, jaundice (yellow eyes or skin), dark urine, pale stools, abdominal pain, swelling, or easy bruising. Early evaluation allows interventions that can prevent permanent liver damage.
Reference
- Physiology, Liver” — NCBI Bookshelf (StatPearls)
https://www.ncbi.nlm.nih.gov/books/NBK535438/ NCBI - “Liver: Anatomy and Functions” — Johns Hopkins Medicine
https://www.hopkinsmedicine.org/health/conditions-and-diseases/liver-anatomy-and-functions Johns Hopkins Medicine - “Diagnosis and Management of Nonalcoholic Fatty Liver Disease” — American Academy of Family Physicians
https://www.aafp.org/pubs/afp/issues/2023/0500/practice-guidelines-nonalcoholic-fatty-liver-disease.html American Academy of Family Physicians - “The Liver and Its Functions” — Columbia Surgery
https://columbiasurgery.org/liver/liver-and-its-functions Columbia Surgery - “The Liver: What It Does, Disorders & Symptoms, Staying Healthy” — Cleveland Clinic
https://my.clevelandclinic.org/health/articles/21481-liver Cleveland Clinic - “Nonalcoholic Fatty Liver Disease — Diagnosis & Treatment” — Mayo Clinic
https://www.mayoclinic.org/diseases-conditions/nonalcoholic-fatty-liver-disease/diagnosis-treatment/drc-20354573
Autum Harkins is a CNS with an MS in Clinical Nutrition from Maryland University of Integrative Health (2017) and 8 years in integrative clinics. She develops individualized protocols for deficiencies, digestive health, and women’s wellness, prioritizing third-party-tested supplements. Autum contributes to case series and webinars and mentors practitioners on lab interpretation. Credentials: CNS Board (ANA/BCNS) number, state nutrition licensure where applicable, and professional memberships with links.