Sleep disturbances are conditions that affect the quality, duration, or timing of sleep, with insomnia (difficulty falling or staying asleep) and hypersomnia (excessive daytime sleepiness) being most common. They arise from medical, psychological, lifestyle, or environmental causes and can severely impact mental and physical health.
Key Takeaways
- Insomnia causes poor sleep initiation or maintenance, leading to fatigue, mood issues, and low focus.
- Hypersomnia results in persistent drowsiness and unrefreshing sleep, often linked to other medical or mental conditions.
- Diagnosis involves sleep diaries, questionnaires, and sleep studies for accurate assessment.
- Treatments include cognitive-behavioral therapy, medications, lifestyle changes, and devices like CPAP.
- Prevention relies on consistent sleep routines, reduced screen time, stress control, and optimizing the sleep environment.
- Managing underlying conditions and practicing good sleep hygiene support long-term sleep health.
What Are Sleep Disturbances?
Sleep disturbances refer to any conditions that interfere with the quantity, quality, or timing of your sleep. Disruptions may take the form of trouble falling asleep, staying asleep, waking too early, feeling unrefreshed after adequate sleep, or experiencing excessive daytime sleepiness. Sleep disturbances range from short-term challenges (like jet lag) to chronic disorders that require medical evaluation and intervention.
- Difficulty initiating or maintaining sleep (insomnias)
- Excessive daytime sleepiness (hypersomnias)
- Irregular sleep-wake cycles
- Disruptive behaviors during sleep (parasomnias)
- Sleep-related breathing disorders (e.g., sleep apnea)
Insomnia: Causes, Symptoms, and Effects

Insomnia is the most prevalent sleep disorder. It is generally defined as trouble falling asleep, staying asleep, or waking too early and not being able to fall back asleep despite having adequate opportunities for sleep. Chronic insomnia lasts at least three nights a week for three months or more.
Symptoms of Insomnia
Insomnia is a sleep disorder that makes it hard to fall asleep, stay asleep, or feel well-rested. Its symptoms show up both at night and during the day.
At Night
- Difficulty Falling Asleep: You may lie in bed for a long time before you can drift off, even if you’re tired and ready for sleep.
- Frequent Night Awakenings: It’s common to wake up multiple times during the night, sometimes staying awake for long periods before falling back asleep.
- Early Morning Awakenings: You might wake up much earlier than you want and find it impossible to get back to sleep, even if you still feel sleepy.
- Feeling Unrefreshed Upon Waking: Even after what seems like a full night in bed, you wake up feeling tired or like you didn’t sleep at all.
During the Day
Insomnia doesn’t just affect your nights. It also causes problems during the day, such as:
- Daytime Fatigue: You feel unusually tired, low on energy, or sleepy.
- Mood Changes: Irritability, anxiety, or low mood are common, making it harder to handle stress or interact with others.
- Difficulty Concentrating: It’s hard to focus, remember things, or make decisions, which can affect work or school performance.
- Reduced Performance: You might make more mistakes, have slower reaction times, or find it hard to stay productive.
- Worry About Sleep: Constant thoughts about your inability to sleep can increase stress and make insomnia worse.
Causes of Insomnia
Insomnia can happen for many reasons. Sometimes it’s a problem by itself (primary insomnia), but often it’s linked to other health issues or lifestyle factors (secondary insomnia). Let’s look at some of the most common causes:
1. Medical and Physical Conditions
Chronic pain, menopause, hormonal changes, and problems like asthma or frequent urination often disrupt sleep and can cause or worsen insomnia.
- Chronic Pain and Illness: Ongoing pain from conditions like arthritis, back pain, or injuries can make it hard to fall or stay asleep.
- Menopause and Hormonal Changes: Night sweats and hot flushes during menopause can disrupt sleep, and hormonal shifts at any age can affect sleep quality.
- Respiratory or Urinary Problems: Breathing difficulties (such as asthma) or needing to use the bathroom frequently at night (due to bladder issues) can interrupt sleep.
2. Other Sleep Disorders
Conditions such as sleep apnea and restless legs syndrome can interrupt normal sleep, making it hard to fall or stay asleep and often leading to insomnia.
- Sleep Apnea: Causes breathing pauses that wake you up.
- Restless Legs Syndrome: An uncomfortable urge to move your legs, especially at night, can make falling and staying asleep hard.
3. Substances and Medications
Caffeine, nicotine, alcohol, certain medications, and recreational drugs can interfere with falling asleep or staying asleep, often triggering or worsening insomnia.
- Caffeine and Nicotine: Both are stimulants that can keep you awake if used in the afternoon or evening.
- Alcohol: May help you fall asleep at first but can disrupt sleep later in the night.
- Medications: Some prescriptions and over-the-counter drugs, including certain antidepressants, blood pressure medications, or allergy drugs, can interfere with sleep.
- Recreational Drugs: Many can disrupt the sleep cycle.
4. Mental Health and Emotional Factors
Anxiety, depression, stress, grief, and relationship issues can keep the mind active at night, making it difficult to relax and fall or stay asleep.
- Anxiety and Depression: Worry, rumination, and low mood are common reasons for trouble sleeping.
- Stress and Grief: Big life changes, ongoing stress, or the loss of a loved one can keep your mind active at night.
- Relationship Issues: Arguments or breakups can also affect sleep.
5. Poor Sleep Habits (Sleep Hygiene)
Irregular sleep schedules, late-night screen time, long naps, and an inconsistent bedtime routine can all disrupt the body’s natural sleep rhythm and contribute to insomnia.
- Irregular Sleep Schedules: Going to bed and waking up at different times each day confuses your body clock.
- Too Much Screen Time Before Bed: Phones, tablets, and TVs emit blue light, which can interfere with the hormone melatonin, making it harder to fall asleep.
- Frequent Napping: Long or late-day naps can reduce your ability to sleep at night.
6. Environmental Factors
Excess noise, light, uncomfortable bedding, or extreme temperatures in your sleep environment can disturb your rest and make it harder to get quality sleep.
- Noise: Loud or sudden sounds can wake you up or prevent you from falling asleep.
- Light: Bright rooms or light from electronic devices can disturb sleep.
- Uncomfortable Sleep Environment: Poor mattress, extreme temperatures, or shared beds can make sleep difficult.
Hypersomnia: Causes, Symptoms, and Effects
Hypersomnia is characterized by excessive daytime sleepiness or excessive time spent sleeping. People with hypersomnia struggle to stay awake during the day or sleep longer than normal, yet still feel unrefreshed.
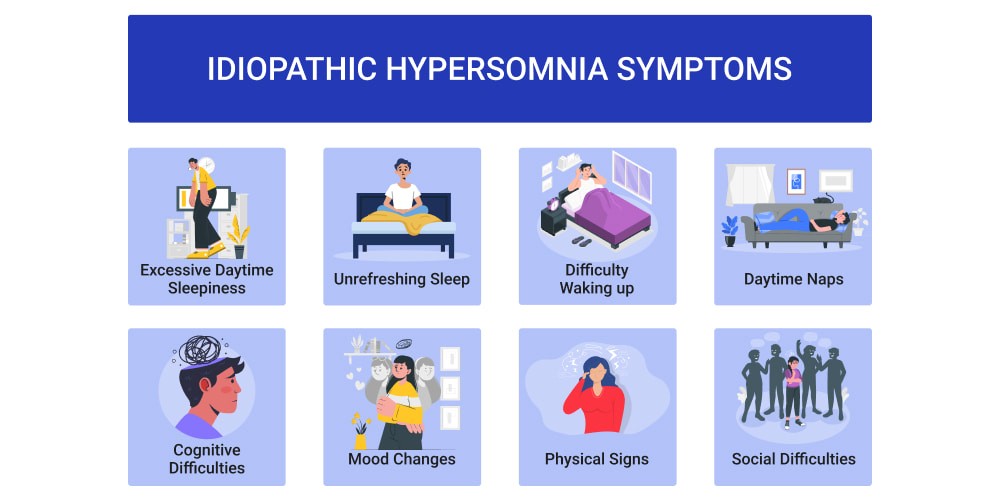
Symptoms of Hypersomnia
Symptoms of hypersomnia include persistent daytime sleepiness, long unrefreshing naps, difficulty waking up, mental fog, poor concentration, apathy, and increased accident risk.
- Persistent daytime sleepiness: Feeling tired all day, even after enough sleep.
- Long, unrefreshing naps: Taking naps that do not help you feel rested.
- Difficulty waking up: Trouble getting out of bed, sometimes feeling confused.
- Poor concentration and memory: Struggling to focus or remember things.
- Trouble thinking clearly: Experiencing mental fog or slow thinking.
- Apathy and lack of motivation: Little interest or energy for activities.
- Increased accident risk: More likely to make mistakes or have accidents due to drowsiness.
Causes of Hypersomnia
Hypersomnia can result from a range of medical, psychological, and lifestyle factors, including:
- Other Sleep Disorders: Conditions like sleep apnea and narcolepsy can disrupt nighttime sleep and cause excessive daytime sleepiness.
- Medical Conditions: Illnesses such as head injuries, brain tumors, multiple sclerosis, hypothyroidism, and certain neurological disorders can lead to hypersomnia.
- Medications: Some prescription drugs, especially those used for anxiety, depression, or allergies, can cause drowsiness as a side effect.
- Substance Use: Alcohol and recreational drugs can disrupt normal sleep patterns and cause increased sleepiness.
- Depression and Mental Health Disorders: Mood disorders often affect sleep regulation, leading to excessive sleepiness.
- Genetics: A family history of hypersomnia or related sleep conditions can increase risk.
- Lack of Quality Sleep: Poor sleep quality due to frequent interruptions, even with enough hours in bed, can cause hypersomnia.
- Obesity: Being overweight increases the risk of sleep disorders that may result in hypersomnia.
How Sleep Disorders Are Diagnosed
Sleep disorders are diagnosed using a combination of methods:
- Medical history: A doctor reviews your symptoms, health conditions, medications, and lifestyle.
- Sleep diary: You may be asked to track your sleep patterns, naps, and how you feel during the day for one to two weeks.
- Questionnaires: Standardized tools assess the severity and type of sleep problems (such as the Epworth Sleepiness Scale).
- Physical exam: Checks for medical issues that may cause sleep disturbances.
- Sleep studies (polysomnography): An overnight test records brain activity, breathing, heart rate, and movements while you sleep, often done in a sleep clinic.
- Home sleep tests: Portable monitors may be used for some conditions, like sleep apnea, in your own home.
Sleep Disorder Treatments
Treatment options for sleep disorders are tailored to the specific condition, focusing on addressing symptoms, improving sleep quality, and enhancing overall well-being. Below are detailed explanations of the key approaches:

- Cognitive Behavioral Therapy for Insomnia (CBT-I): Structured therapy targets negative thoughts and behaviors about sleep. Uses techniques like sleep restriction, stimulus control, and relaxation. Proven in randomized trials as the first-line treatment for chronic insomnia, with durable results.
- Sleep Hygiene Improvements: Establishes regular sleep-wake times, limits screen time before bed, and creates a quiet, dark, and comfortable environment. Evidence supports improved sleep quality by reducing behavioral and environmental triggers.
- Medications: Prescribed according to disorder. Sedative-hypnotics or melatonin agonists for insomnia, stimulants for narcolepsy, and dopamine agonists or anticonvulsants for restless legs syndrome. Used short-term or with therapy, with close monitoring for side effects and dependency.
- Continuous Positive Airway Pressure (CPAP): Device delivers pressurized air via mask, keeping airways open for patients with obstructive sleep apnea. Multiple trials show CPAP improves sleep architecture, reduces daytime sleepiness, and lowers cardiovascular risks.
- Light Therapy: Timed exposure to bright light resets circadian rhythms. Used for delayed sleep phase disorder and seasonal affective disorder, with clinical trials showing benefit in improving sleep-timing and mood.
- Lifestyle Modifications: Regular exercise, management of stress with meditation or yoga, and avoiding caffeine/alcohol in the evening. Lifestyle changes are associated with better long-term outcomes in observational and interventional studies.
- Hypoglossal Nerve Stimulation: Implanted device stimulates tongue muscle via hypoglossal nerve to maintain airway for obstructive sleep apnea. Effective for patients who do not tolerate CPAP, supported by clinical trial data.
Sleep Disorder Prevention and Management
While not all sleep disorders can be prevented, certain lifestyle changes can improve sleep quality and significantly reduce the risk of developing sleep-related issues. Here’s how each measure helps.
- Maintaining a Consistent Sleep Schedule: Going to bed and waking up at the same time every day helps regulate your body’s internal clock, making it easier to fall asleep and wake up refreshed. This consistency is especially important for preventing circadian rhythm disorders.
- Creating a Relaxing Bedtime Routine: Engaging in calming activities like reading, meditation, or a warm bath signals your brain that it’s time to wind down. This routine prepares your mind and body for restful sleep and reduces insomnia symptoms.
- Optimizing the Sleep Environment: Keeping the bedroom quiet, dark, and cool, along with investing in a comfortable mattress and pillows, enhances sleep quality. A well-designed environment minimizes disturbances and promotes deeper sleep cycles.
- Limiting Exposure to Screens Before Bedtime: Blue light emitted by screens suppresses melatonin production, delaying sleep onset. Avoiding electronic devices an hour before bed helps reset your natural sleep-wake cycle.
- Managing Stress Through Relaxation Techniques: Practices such as yoga, deep breathing, and mindfulness reduce stress and anxiety, which are common contributors to sleep disturbances. Relaxation lowers cortisol levels, allowing the body to transition into sleep more easily.
- Avoiding Caffeine, Alcohol, and Heavy Meals Close to Bedtime: Stimulants like caffeine and alcohol disrupt sleep by interfering with natural sleep stages. Similarly, heavy meals can cause discomfort, keeping you awake longer.
- Regular Exercise (but Not Too Close to Bedtime): Physical activity promotes better sleep by reducing stress and increasing time spent in deep sleep stages. However, exercising too close to bedtime can elevate energy levels, making it harder to fall asleep
Conclusion
Sleep disturbances are conditions that affect how well or how long you sleep, impacting daily functioning and health. The most common types are insomnia, where people struggle to fall or stay asleep, and hypersomnia, marked by persistent daytime sleepiness and unrefreshing naps. Causes range from chronic pain, hormonal changes, and mental health issues to poor sleep habits, medications, or other sleep disorders.
Symptoms include tiredness, mood swings, poor concentration, and higher risk of accidents. Diagnosis often involves sleep diaries, questionnaires, physical exams, and overnight sleep studies. Treatments can include cognitive-behavioral therapy, medication, devices such as CPAP, and healthy lifestyle changes. Prevention focuses on maintaining consistent routines, creating a comfortable sleep environment, and managing stress.
FAQs
What are sleep disturbances?
Sleep disturbances are conditions that interfere with your ability to get enough quality sleep, including trouble falling asleep, staying asleep, waking too early, or feeling sleepy during the day.
What is insomnia?
Insomnia is difficulty falling asleep, staying asleep, or waking too early and not being able to fall back asleep, even when you have time and opportunity to rest.
What causes insomnia?
Insomnia can be caused by stress, medical or mental health conditions, other sleep disorders, medications, poor sleep habits, or environmental factors like noise and light.
What is hypersomnia?
Hypersomnia means experiencing excessive sleepiness during the day or sleeping for unusually long periods, yet still feeling tired and unrefreshed.
What are common symptoms of hypersomnia?
Symptoms include persistent daytime sleepiness, long but unrefreshing naps, difficulty waking up, poor focus, and increased risk of accidents.
Can sleep disturbances be prevented?
Some sleep disturbances can be prevented or reduced by maintaining a regular sleep schedule, creating a restful sleep environment, managing stress, and practicing good sleep habits.
When should I see a doctor about sleep problems?
See a healthcare provider if you have trouble sleeping for several weeks, feel tired during the day despite enough sleep, or experience loud snoring, breathing pauses, or unusual behaviors during sleep.
How are sleep disorders diagnosed?
Diagnosis may involve a review of your medical history, sleep diaries, questionnaires, physical exams, and sometimes overnight sleep studies in a clinic or at home.
What treatments are available for sleep disorders?
Treatment options include cognitive-behavioral therapy, medication, lifestyle changes, and devices such as CPAP for sleep apnea.
How can I naturally improve my sleep?
Stick to a consistent sleep schedule, avoid caffeine and screens before bed, keep your bedroom quiet and dark, and manage stress with relaxation techniques.
References
- MedlinePlus. (1999). Sleep disorders. Retrieved from https://medlineplus.gov/sleepdisorders.html
- American Psychiatric Association. (2024). What are sleep disorders? Retrieved from https://www.psychiatry.org/patients-families/sleep-disorders/what-are-sleep-disorders
- HelpGuide.org. (2025). Sleep therapy: Treating sleep problems with CBT. Retrieved from https://www.helpguide.org/wellness/sleep/therapy-for-sleep-disorders
- National Center for Biotechnology Information. (2023). Sleep disorder. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK560720/
- Care Insurance. (2024). Sleep disorders: Types, causes, symptoms & treatment. Retrieved from https://www.careinsurance.com/blog/health-insurance-articles/8-tips-to-make-sleep-disorders-ineffective
- Mayo Clinic. (2024). Sleep disorders – Diagnosis and treatment. Retrieved from https://www.mayoclinic.org/diseases-conditions/sleep-disorders/diagnosis-treatment/drc-20572160
- American Academy of Family Physicians. (2022). Common sleep disorders in adults: Diagnosis and management. Retrieved from https://www.aafp.org/pubs/afp/issues/2022/0400/p397.html
- Cleveland Clinic. (n.d.). Sleep disorders: Types, causes, symptoms & treatment. Retrieved from https://my.clevelandclinic.org/-/scassets/images/org/health/articles/11429-sleep-disorders
- PubMed. (n.d.). Overview of sleep & sleep disorders. Retrieved from https://pubmed.ncbi.nlm.nih.gov/20308738/
Autum Harkins is a CNS with an MS in Clinical Nutrition from Maryland University of Integrative Health (2017) and 8 years in integrative clinics. She develops individualized protocols for deficiencies, digestive health, and women’s wellness, prioritizing third-party-tested supplements. Autum contributes to case series and webinars and mentors practitioners on lab interpretation. Credentials: CNS Board (ANA/BCNS) number, state nutrition licensure where applicable, and professional memberships with links.


